Type 2 diabetes (T2D) is a chronic condition that happens when you have constant high blood sugar. This happens because your body can’t use insulin properly. You can manage this condition with lifestyle changes, medications and regular check-ins with your healthcare team.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Type 2 diabetes (T2D) happens when your body can’t use insulin properly and/or doesn’t make enough of it. This leads to high blood sugar (hyperglycemia). It’s a condition you have to manage for the rest of your life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthy blood sugar (glucose) levels are 70 to 99 milligrams per deciliter (mg/dL). If you have undiagnosed Type 2 diabetes, your levels are typically 126 mg/dL or higher.
This condition is very common. About 1 in 10 people in the U.S. has diabetes. And about 90% to 95% of them have T2D. Researchers estimate that it affects about 6.3% of the world’s population.
Most people who have T2D are over 45. But people younger than 45 can have it as well, including children.
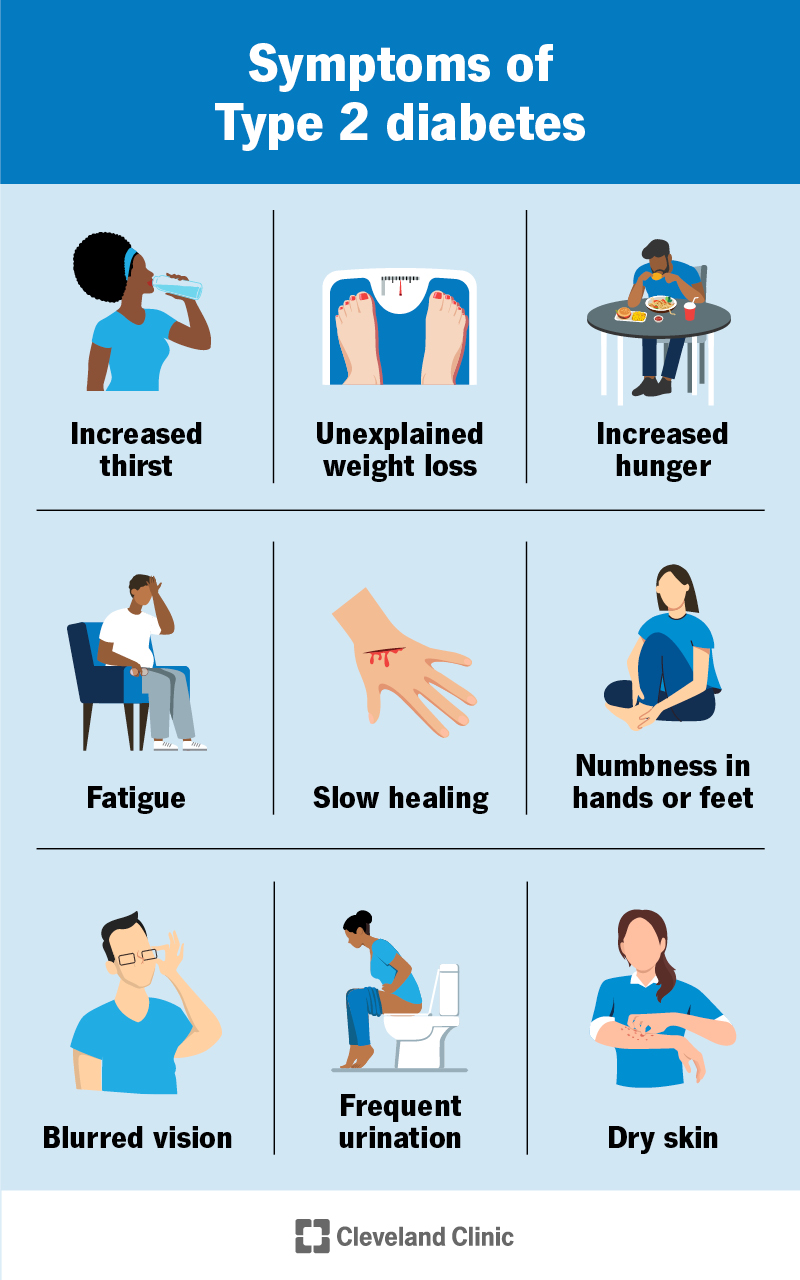
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21501-type-2-diabetes)
Type 2 diabetes symptoms tend to develop slowly. They can include:
Females may experience frequent vaginal yeast infections and/or urinary tract infections (UTIs).
If you have these symptoms, see your healthcare provider. Blood tests can diagnose T2D.
The main cause of Type 2 diabetes is insulin resistance.
Insulin resistance happens when certain cells in your body don’t respond as they should to insulin. Insulin is a hormone your pancreas makes that keeps your glucose levels in range.
With this resistance to insulin, your pancreas must make more of it to overcome increasing glucose levels. If your cells become too resistant to insulin and your pancreas can’t make enough, it leads to T2D.
Advertisement
Several factors can contribute to insulin resistance, including:
The cause of T2D is complex. But researchers know that genetics plays a strong role. Your lifetime risk of developing T2D is 40% if you have one biological parent with T2D. It’s 70% if both of your biological parents have it.
Researchers have identified at least 150 DNA variations linked to the risk of developing T2D. Some raise your risk, and others lower it. Some of these variations may directly play a role in insulin resistance and production. Others may increase your risk by increasing your tendency to have overweight or obesity.
These gene changes likely act together with other factors to influence your overall risk of T2D.
You’re more likely to develop Type 2 diabetes if you:
T2D symptoms typically come on slowly. So, it’s important to see your primary care provider regularly if you have risk factors. This way, they can do screenings to check on your blood sugar levels. It’s better to catch T2D earlier rather than later.
Having undiagnosed or undermanaged Type 2 diabetes can damage several areas of your body. Long-term complications of T2D can include:
An acute (sudden and severe) complication of T2D is hyperosmolar hyperglycemic state (HHS). It’s life-threatening. HHS happens when your glucose levels are very high for days to weeks, leading to severe dehydration and confusion.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_5f76yxwg/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn about the early signs of diabetes.
The following blood tests help your healthcare provider diagnose Type 2 diabetes:
Advertisement
In some cases, your provider may order an autoantibody blood test to see if you have Type 1 Diabetes instead of T2D.
The key parts of managing Type 2 diabetes include:
You mainly manage T2D on your own with medical guidance and support from your healthcare team. This could include your:
Your team should also include family members and other important people in your life. Managing T2D can be challenging — you must make several decisions every day for it. Loved ones can help carry this mental load.
Regular physical activity is helpful for managing T2D because it:
Talk to your provider before starting an exercise program. You may need to take special steps before, during and after physical activity. Especially if you take insulin. The general goal is to get at least 150 minutes per week of moderate-intensity physical activity.
Advertisement
Together, you and your healthcare provider or a dietitian will form a meal plan that works for you. What and when you eat impact your blood sugar.
Most providers recommend eating a variety of nutritious foods. In general, the following types of foods can help support healthy glucose levels:
Your provider may recommend taking medication for Type 2 diabetes. These include:
Monitoring your glucose helps you know how well your current treatment plan is working. It can help you make decisions about food, physical activity and medication needs.
Advertisement
Several things can affect your blood sugar. You can learn to predict some of these impacts with time and practice. But others are very difficult or impossible to predict. That’s why it’s important to check your glucose regularly if your healthcare provider recommends doing so. Your provider will also give you a goal glucose range.
The two main ways you can monitor your glucose at home are with a glucose meter and/or a continuous glucose monitor (CGM).
Type 2 diabetes is a chronic (long-term) disease. This means you must manage it for the rest of your life. There’s no cure for T2D. But you can manage it in a way that keeps your blood sugar levels in a healthy range. If you stop managing it or undermanage it, your blood sugar levels will go back up.
You’ll need regular appointments with your healthcare team to be sure you’re on track with your T2D management plan. As your body, life and routines change, your management will change, as well. Your healthcare team can provide new strategies tailored to your needs.
If you develop symptoms of any complications, see your provider as soon as possible.
With Type 2 diabetes, you must make decisions every day to stay healthy. It’s a complex condition that requires a lot of effort and changes. This can be tough. But it’s also very doable with the right education and healthcare providers by your side. Getting support from your family and friends is a big help, too.
You’ll need to prioritize both your physical and mental health to stay healthy long-term. Maintaining in-range blood sugar levels is key to preventing serious complications.
In general, your outlook depends on several factors, like:
Aside from getting proper medical care and guidance, the following can help you thrive with T2D:
Certain strategies can help lower your risk of getting Type 2 diabetes or delay its onset, like:
Some people have such strong genetic risk factors that even lifestyle changes aren’t enough to prevent developing T2D.
Type 2 diabetes involves constant day-to-day care and management. It’ll likely be very overwhelming at first. But over time, you’ll get a better grasp on how to manage the condition. You’ll learn to be in tune with your body.
Managing Type 2 diabetes involves a team effort — you’ll want both medical professionals and loved ones on your side. Don’t hesitate to reach out to them if you need help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Type 2 diabetes can affect your life in many ways. At Cleveland Clinic, we can help develop a treatment plan that matches you and your goals.
