Insulin resistance is a complex condition in which your body doesn’t respond as it should to insulin. Insulin is a hormone your pancreas makes that’s essential for regulating blood sugar levels. Several genetic and lifestyle factors can contribute to insulin resistance.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_lrld1uus/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn about insulin resistance and what insulin does in your body.
Insulin resistance happens when cells in your muscles, fat and liver don’t respond to insulin as they should. This is also known as impaired insulin sensitivity. Insulin is essential for life and regulating blood glucose (sugar) levels.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Insulin helps move glucose from your blood into your cells so your body can use it for energy. For several reasons, your cells can respond inappropriately to insulin. This means they can’t efficiently use the glucose for energy or for storage. As a result, glucose continues to build up in your blood. Your pancreas makes more insulin to try to overcome your increasing blood glucose levels. This is called hyperinsulinemia.
As long as your pancreas can make enough insulin to balance out your blood sugar levels, they’ll stay in a healthy range. If your cells become too resistant to insulin, it leads to elevated blood glucose levels (hyperglycemia).
Over time, hyperglycemia can lead to prediabetes and Type 2 diabetes.
The condition is also associated with:
Insulin resistance can affect anyone — you don’t have to have diabetes — and it can be temporary (for example, using steroid medication for a brief period causes insulin resistance) or chronic. The two main factors that seem to contribute to insulin resistance are excess body fat, especially around your belly, and a lack of physical activity.
Advertisement
Having a family history of insulin resistance (family members with prediabetes, type 2 diabetes, and/or PCOS) can also contribute to insulin resistance.
People who have prediabetes and Type 2 diabetes usually have insulin resistance. People with Type 1 diabetes can also experience insulin resistance.
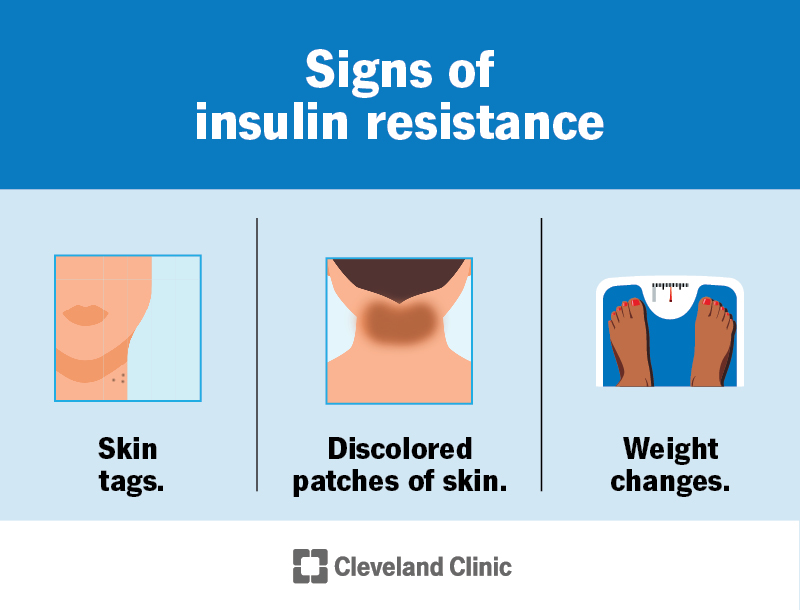
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22206-insulin-resistance)
If you have insulin resistance, but your pancreas can increase insulin production to keep your blood sugar levels in range, you won’t have any symptoms.
But over time, the condition can get worse, and the cells in your pancreas that make insulin can wear out. Eventually, your pancreas can’t produce enough insulin to overcome it, leading to elevated blood sugar.
People with consistently high blood sugar levels can experience the following symptoms:
Many people have no symptoms of prediabetes, often for years. Prediabetes may be invisible until it develops into Type 2 diabetes. Some people with prediabetes may experience the following symptoms:
If you’re experiencing any of these symptoms, it’s important to see your healthcare provider.
Scientists still have a lot to discover about how exactly it develops. So far, they’ve identified several genes that make a person more or less likely to develop insulin resistance. Providers also know that gaining weight can worsen it, and losing weight can help improve it. Other factors and conditions can cause varying degrees of the condition.
Acquired causes of the condition, meaning you’re not born with the cause, include:
Issues with certain hormones can affect how well your body uses insulin. Hormonal disorders that can cause insulin resistance include:
Advertisement
Certain inherited genetic disorders — conditions you’re born with – can cause the condition for various reasons. These are rare but include Type A insulin resistance syndrome and Donohue syndrome.
Other inherited conditions that can cause it include:
Advertisement
Insulin resistance is difficult to diagnose because there isn’t routine testing for it. As long as your pancreas is producing enough insulin to overcome the resistance, you won’t have any symptoms.
Your healthcare provider will consider several factors when evaluating you for the condition. These might include your:
Your healthcare provider may order the following blood tests to diagnose the condition:
Not all factors that contribute to the condition can be treated, such as genetic factors and age. For this reason, lifestyle modifications are the primary treatment for insulin resistance. Lifestyle modifications include:
Advertisement
Over time, these lifestyle modifications can:
Your healthcare provider might refer you to a specialist, like a dietitian or endocrinologist. They’ll work together with you to come up with an individualized treatment plan.
There are currently no medications that treat the condition specifically. Your healthcare provider may prescribe medications to treat coexisting conditions. Some examples include:
The condition has several causes and contributing factors, and not all causes are reversible. But lifestyle changes can make a difference. Eating nutritious foods, exercising regularly and losing excess weight may decrease your insulin resistance. Talk to your healthcare provider about what you can do to best manage it.
What you eat can have a big impact on your blood sugar and insulin levels. The glycemic index (GI) is a tool that can help you determine what foods have the biggest impact on your blood sugar levels.
High-GI foods generally have a lot of carbohydrates and/or sugar. They cause your blood sugar to increase quickly and require a lot of insulin to bring blood sugar back down. You’ll want to avoid high-sugar drinks like regular soda and juices, and avoid eating excess amounts of the following foods:
Low-GI foods cause a steadier rise in blood sugar. Your pancreas doesn’t have to work as hard to release insulin. Eating foods that are lower on the glycemic index is generally better for people with insulin resistance:
Always talk to your healthcare provider before making extreme changes to your eating patterns.
If you have the condition, ask your healthcare provider about what you can expect and how best to manage it.
What you can expect depends on several factors, including:
People can have mild insulin resistance that never turns into prediabetes or Type 2 diabetes. People can also have insulin resistance that’s reversible or manageable with lifestyle changes.
Complications can occur when the condition isn’t managed. Possible complications include:
Not everyone who has insulin resistance will have complications. If you’ve been diagnosed with it, it’s important to try to prevent these complications. Be sure to see your healthcare provider regularly and follow your treatment plan.
Certain genetic and lifestyle risk factors make it more likely that you’ll develop insulin resistance or prediabetes. Risk factors include:
You may have a higher risk of developing it if you are:
You can’t change certain risk factors for insulin resistance, such as family history or age. But you can try lowering your chances of developing it by maintaining a healthy weight for you and exercising regularly.
If you’ve been diagnosed with the condition, it’s important to see your healthcare provider regularly. They’ll check to make sure your blood sugar levels are in a healthy range and that your treatment is working.
If you’re experiencing symptoms of high blood sugar or prediabetes, contact your healthcare provider. They can run simple tests to check your blood sugar levels.
If you have a family history of diabetes or insulin resistance, talk to your healthcare provider about your risk of developing it.
If you receive a diagnosis, it may be helpful to ask your healthcare provider the following questions:
Insulin resistance is a complex condition that can affect your health in several ways. It doesn’t have any symptoms until it turns into prediabetes or Type 2 diabetes. The best thing you can do is try to prevent or reverse it by maintaining a healthy weight, exercising regularly and eating nutritious foods. Unfortunately, though, not all causes of the condition are preventable or treatable. If you have any questions about your risk of developing insulin, talk you your healthcare provider. They’re there to help you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you’ve been living with diabetes for years or you’re newly diagnosed, you want experts you can trust. Our team at Cleveland Clinic is here to help.
