Diabetes-related neuropathy is nerve damage that affects people with diabetes. The most common type is peripheral neuropathy, which often affects your feet. There’s no cure for diabetes-related neuropathy. But you can manage it with medication, therapies and tighter blood sugar management.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Diabetes-related neuropathy happens when you experience nerve damage due to high blood sugar (hyperglycemia) that lasts a long time. It can affect people with long-term diabetes, like Type 1 diabetes and Type 2 diabetes. But not everyone with diabetes develops it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Neuropathy can develop from other causes, too, like pinched nerves, inflammation, nutrient deficiencies and injuries affecting your nerves. Healthcare providers diagnose neuropathy as diabetes-related if you have diabetes and they can’t find another cause for it.
Diabetes-related neuropathy can damage different nerves throughout your body. Types of diabetes-related neuropathy include:
Overall, diabetes-related neuropathy is fairly common. Studies show that up to 50% of people with diabetes have peripheral neuropathy. More than 30% of people with diabetes have autonomic neuropathy.
Advertisement
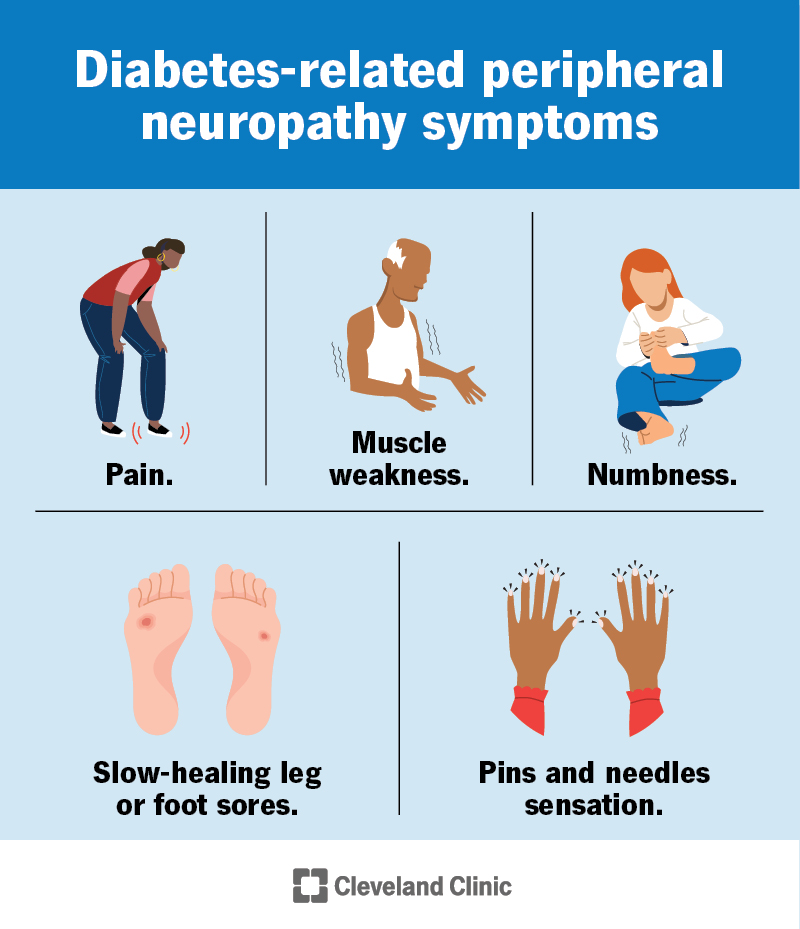
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21621-diabetic-neuropathy)
Your symptoms will depend on which type of diabetes-related neuropathy you have.
Diabetes-related peripheral neuropathy commonly affects your feet. Symptoms include:
Nerve damage that causes peripheral neuropathy typically develops over many years. You may not notice symptoms of mild nerve damage for a long time.
Autonomic neuropathy can have many different symptoms because it can affect several body systems. Examples include:
Autonomic neuropathy can also cause hypoglycemia unawareness. This means you don’t experience the typical warning signs of low blood sugar, like shakiness, confusion and intense hunger.
Symptoms of proximal neuropathy include:
Perpetually high blood sugar levels can damage small blood vessels that provide oxygen and nutrients to your nerves. Without enough oxygen and nutrients, nerve cells can die, affecting the function of your nerve. This causes neuropathy.
Each person is different, so it’s almost impossible to predict how high blood sugar levels have to be — and for how long — to cause neuropathy. One study of people with Type 2 diabetes shows that having an A1C over 7% for at least three years increases your risk of diabetes-related neuropathy. An A1C of 7% means your blood sugar is 154 mg/dL on average.
If you have diabetes, your chance of developing diabetes-related neuropathy increases the older you get and the longer you’ve had diabetes.
Studies show that peripheral neuropathy affects at least 20% of people with Type 1 diabetes who’ve had diabetes for at least 20 years. It affects 15% to 50% of people with Type 2 diabetes who’ve had diabetes for at least 10 years.
Advertisement
You’re also more likely to develop neuropathy if you have diabetes along with:
Studies show that genetics may also increase your risk of diabetes-related neuropathy.
To start, a healthcare provider will ask detailed questions about your medical history and diabetes management. They’ll ask about your symptoms and do a physical exam. Tests that help confirm a diabetes-related neuropathy diagnosis include:
Tests to diagnose autonomic neuropathy vary depending on which body system is affected. For example, an ultrasound can show how well your bladder empties when you pee. Tests like gastric emptying scintigraphy (GES) can help diagnose digestive system issues.
Advertisement
It may take more time to get an autonomic neuropathy diagnosis, as many other conditions can cause the same symptoms.
Diabetes-related neuropathy treatment involves carefully managing your blood sugar. This is the most important step to prevent nerve damage from getting worse. Your healthcare provider and other diabetes specialists — like a CDCES (Certified Diabetes Care and Education Specialist) — will work with you to achieve realistic blood sugar goals.
Treatment for the symptoms of neuropathy varies depending on the type you have. The following medications can help treat painful symptoms that disturb your sleep or daily activities:
Therapies are also helpful, including:
Advertisement
Treatments for autonomic neuropathy vary based on the specific issue. Your provider will work with you to find the best option for you.
With improved blood sugar management, symptoms of diabetes-related neuropathy like numbness and other abnormal sensations may fade within one year. The more severe neuropathy is, the less likely it is that it’ll be reversible.
If you have diabetes-related neuropathy, your prognosis (outlook) depends on several factors, like:
Your healthcare provider will be able to give you a better idea of what to expect.
Without proper treatment, peripheral neuropathy can affect your quality of life. This is why it’s essential to seek medical help as soon as you notice signs of it.
Autonomic neuropathy can be serious because it involves your body’s vital functions. When those don’t work correctly, it can have very severe — and sometimes, life-threatening — effects.
Possible complications of peripheral neuropathy include:
Complications of autonomic neuropathy vary depending on the affected body system(s).
You can decrease your risk of diabetes-related neuropathy by:
It’s also important to do self-examinations of your feet every day to look for blisters, wounds or broken skin. This can help you catch signs of neuropathy — or complications from it — quickly.
Reversing nerve damage is difficult, so diabetes-related neuropathy may affect your day-to-day life. Besides working with your healthcare provider to carefully manage diabetes and getting treatment for neuropathy, you can make the following adjustments to take care of yourself:
You’ll need to see your healthcare provider regularly if you have diabetes-related neuropathy. This is so they can monitor your symptoms and see if they’re getting worse or better. You’ll also need to see your diabetes provider (like an endocrinologist) regularly to make adjustments to your diabetes management plan.
If you have diabetes-related neuropathy or are at risk for developing it, it may be helpful to ask your healthcare provider the following questions:
It can be difficult and feel defeating to come face-to-face with diabetes complications. But it’s important to listen to what your body is telling you. See your healthcare provider as soon as possible if you notice signs of neuropathy. Tighter management of your blood sugar along with other chronic issues like obesity, high cholesterol, high blood pressure and nutrition deficiencies can improve your symptoms — and prevent neuropathy from getting worse.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you’ve been living with diabetes for years or you’re newly diagnosed, you want experts you can trust. Our team at Cleveland Clinic is here to help.
