Imagine your body is a castle and your immune system is an army fighting off invaders like germs. If the army malfunctions and attacks the castle itself, you may have an autoimmune disease. There’s no cure for autoimmune diseases, but your healthcare provider will help you find treatments that manage the symptoms you experience.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
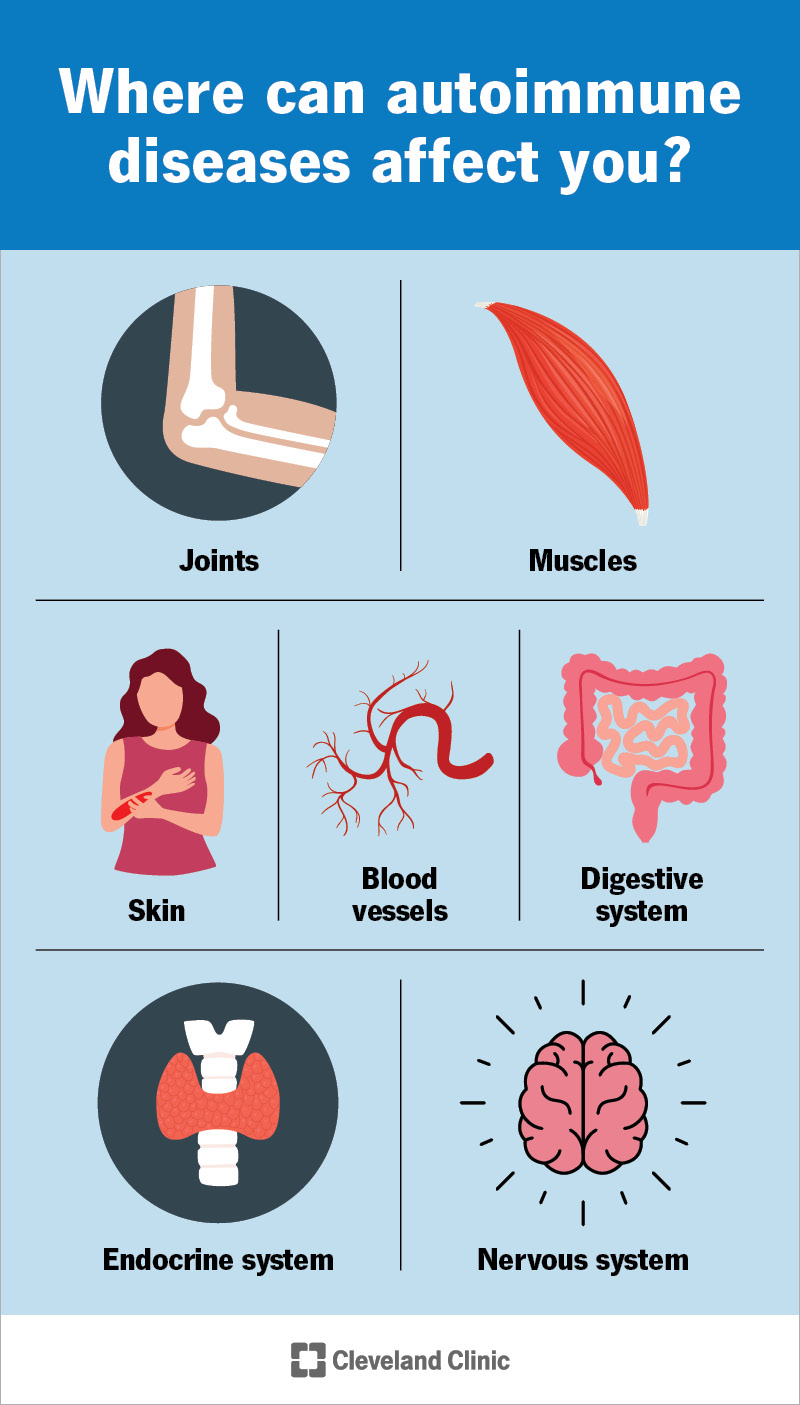
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/autoimmune-diseases-infographic)
Autoimmune diseases are health conditions that happen when your immune system attacks your body instead of defending it. Healthcare providers sometimes call them autoimmune disorders.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Usually, your immune system is like your body’s built-in security system. It automatically detects substances that shouldn’t be in your body (like viruses, bacteria or toxins) and sends out white blood cells to eliminate them before they can damage your body or make your sick.
If you have an autoimmune disease, your immune system is more active than it should be. Because there aren’t invaders to attack, your immune system turns on your body and damages healthy tissue.
Autoimmune diseases are chronic conditions. This means if you have an autoimmune disease, you’ll probably have to manage it and the symptoms it causes for the rest of your life.
There are more than 100 different autoimmune diseases. They can affect almost any tissue or organ in your body, depending on where your immune system malfunctions, including your:
This isn’t a complete list of autoimmune diseases, but some examples of conditions (and where they affect you) include:
Advertisement
Autoimmune diseases are common, especially because there are so many different types. Experts estimate that around 1 in 15 people in the U.S. has an autoimmune disease.
Autoimmune diseases can cause a wide range of symptoms. They can affect your body almost literally from head to toe.
For example, conditions that affect your muscles can cause muscle weakness. You might also have joint pain, swelling or feel stiffness if you have a condition like rheumatoid arthritis. Type 1 diabetes causes high blood sugar (hyperglycemia). Some autoimmune conditions affect your vision.
Many autoimmune diseases cause inflammation, which can include:
Lots of autoimmune diseases cause symptoms that come and go (recur). These episodes of more noticeable or more severe symptoms are called flares or attacks. Tell your provider if you experience symptoms that seem to recur — especially if certain physical activities, times of day, foods or drinks, or anything else makes them noticeably better or worse.
Trust your gut. Nobody knows what’s normal for your body better than you. Visit a healthcare provider if you notice any new symptoms you can’t explain, especially if you don’t feel like yourself more often than usual.
Experts don’t know for certain what causes autoimmune diseases. We know your immune system mistakenly damaging your body instead of protecting it causes the symptoms of an autoimmune disease you experience. But researchers are still studying what makes your immune system start hurting you in the first place.
Some studies have found that certain factors (triggers) might increase your risk of developing an autoimmune disease. Some triggers may include:
Advertisement
Healthcare providers diagnose autoimmune diseases with a physical exam and by discussing your health history. You might also need some tests.
Your provider will examine your body, especially if you’re experiencing symptoms in a specific area. They’ll ask about the symptoms you’re experiencing and when you first noticed them. Tell your provider if you know any of your biological family members have an autoimmune disease.
Diagnosing an autoimmune disease is often a differential diagnosis. This means your provider will test you for several different conditions that can cause the symptoms you’re experiencing until they find the cause.
Your provider might order blood tests to look for specific signs (markers) of autoimmune diseases. These markers are like clues your immune system leaves behind after it damages your body or causes specific issues.
You might need some imaging tests to take pictures of the insides of your body, including:
Autoimmune diseases can need a variety of treatments. Just like the wide variety of symptoms they cause, which treatments you’ll need depends on which condition you have. Everyone’s immune system, genetics and environment are different. That means the treatments that work for you will be unique.
Advertisement
Some common treatments to manage autoimmune disease symptoms include:
You might need specific treatments based on the condition you have. For example, people with Type 1 diabetes need insulin therapy and people with celiac disease need to eat a gluten-free diet.
There’s no cure for autoimmune diseases. They’re chronic (long-term) conditions that usually last your whole life. Some autoimmune diseases enter remission, a long period of time between symptom flares. This isn’t the same as a cure, but it might mean the symptoms impact your daily routine less often.
There might not be any way to prevent autoimmune diseases because experts aren’t sure what causes them.
Everyone’s body and journey with an autoimmune disease is different. Talk to your healthcare provider about the best ways to manage the symptoms you experience. You might need to adjust the kinds of physical activities you do, the foods and drinks you consume or make other tweaks to your day-to-day routine.
Living with an autoimmune disease like lupus, rheumatoid arthritis and multiple sclerosis can be complex and serious. Although there are no cures for these diseases, many of their symptoms can be treated, and sometimes they go into remission. Stay in touch with your healthcare provider about any advances in understanding and treating autoimmune diseases.
Advertisement
It’s hard to give an estimate of how an autoimmune disease will affect your lifespan (how long you live). Some conditions are more serious than others, and can cause fatal complications.
Conditions like multiple sclerosis and myositis are more likely to be fatal than many autoimmune diseases, but that doesn’t mean they always are. Similarly, Type 1 diabetes can be fatal if it’s not managed.
Talk to your healthcare provider. They’ll explain how an autoimmune disease will affect your lifespan (if at all).
Visit a healthcare provider if you’re experiencing new or worsening symptoms you can’t explain — especially if they affect your ability to do all your usual activities.
If you’ve already been diagnosed with an autoimmune disease, tell your provider if it feels like your treatments aren’t working as well as they used to or if the symptoms are recurring more often.
Go to the ER or call 911 (or your local emergency services number) if you experience any of the following severe symptoms:
You may want to ask your provider:
Finding out you have a health condition that you’ll have to manage for the rest of your life can be overwhelming and scary. It might seem even more unfair if your healthcare providers can’t say what caused it.
Having an autoimmune disease can be hard. And it can be tough for others to understand how much effort it can take you just to move through the world on a day-to-day basis. Give yourself credit for how strong you are. Celebrate small victories, and don’t be afraid to feel frustrated or ask for support from your loved ones and providers.
Autoimmune diseases come in all shapes and sizes. Your healthcare providers will help you find treatments that manage the symptoms you experience. You’re not defined by a condition you have, it’s just a part of your health journey.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
