Gangrene is when lack of blood flow causes tissues in your body to die. It often starts on the edges of limbs, like toes or fingers. But it can form anywhere blood’s not reaching. Gangrene looks like a patch of discolored skin (red, brown, purple, green, black). The area may have blisters that leak blood or pus. Prompt treatment is lifesaving.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
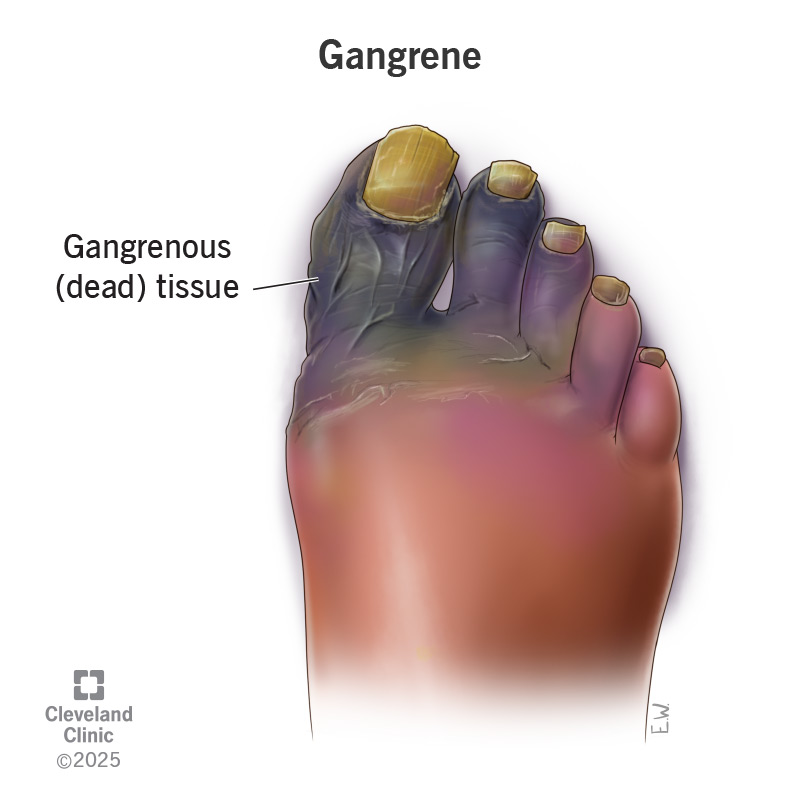
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21070-gangrene)
Gangrene is a medical emergency in which blood stops flowing to a specific part of your body, and tissues in that area die. Gangrene can develop anywhere in your body, but it often starts in your foot or hand.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Gangrene always involves tissue death, but it doesn’t always involve an infection. A gangrene infection is when bacteria grow in the affected area. Without prompt treatment, gangrene (with or without an infection) can lead to serious complications or death.
There are several types of gangrene:
Advertisement
Gangrene symptoms vary by type and may include:
Gangrene causes skin color changes that may occur in stages:
It may be more difficult to see these color changes if you have a darker skin tone.
If there’s an infection, you’ll notice sores or blisters with smelly fluid coming out.
Lack of blood flow to a specific part of your body causes gangrene. Blood delivers oxygen, nutrients and antibodies to your tissues. When your tissues don’t receive blood, they start to die.
Causes of blocked blood flow include:
You face an increased risk of gangrene if you have a condition that affects your blood vessels. Examples include:
You also face a higher risk of gangrene if you have:
If you have any risk factors, see your provider for regular checkups and keep all your follow-up appointments. Your provider will tell you what you can do at home to lower your risk of gangrene — like taking good care of your feet and tending to wounds.
Advertisement
Some medications have been associated with an increased risk of Fournier’s gangrene. Your provider should counsel you on this before starting the medications.
Gangrene is serious and can be life-threatening. It may lead to:
Gangrene is sometimes fatal.
See a healthcare provider right away if you think you have gangrene. Your provider will:
Tests you may need include:
These tests help your provider learn:
Gangrene treatments aim to stop gangrene from spreading, remove dead tissue and help blood flow better. You may need one or more treatments, including:
Advertisement
After gangrene treatment, you may choose to have skin graft surgery. A provider uses healthy skin from another part of your body to cover scars or damaged skin.
Call 911 (or your local emergency service number) or go to your local emergency room if you have gangrene symptoms. You should also seek emergency help if you have symptoms of septic shock:
What you can expect, including your life expectancy, depends on many factors, including:
Your healthcare provider knows your situation best and can give you the most accurate prognosis.
Without treatment, gangrene can quickly become fatal. How long it takes for gangrene to cause death depends on the type of gangrene you have. Gas gangrene progresses very fast. The area of dead tissue can expand several inches with every hour that passes. Gas gangrene is always fatal without treatment, and sometimes fatal even with treatment.
For any type of gangrene, the sooner you get treatment, the better your chances of survival.
Advertisement
Gangrene itself isn’t contagious. That means gangrene doesn’t spread from person to person. But it may be possible for the bacteria that cause a gangrene infection to spread to others. How the bacteria affect an exposed individual depends on many things, like whether they have an open wound at the site of contact and their overall health status.
Talk to a healthcare provider if you or someone in your household has a gangrene infection. They’ll let you know if there are any precautions you should take.
A gangrene diagnosis is scary, whether it happens to you or a loved one. As with any diagnosis, remember that knowledge can give you power. Learn as much as you can about the condition and treatment options. Prompt treatment gives you or your loved one the best chance of surviving.
As you recover, work with your provider to manage underlying conditions. Targeting the root cause of gangrene can help lower your risk of future issues.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you need stitches, a broken bone set or think your appendix might be causing your abdominal pain, Cleveland Clinic’s emergency medicine team is here to help.
