Peripheral artery disease (PAD) is when arteries in your limbs — usually, your legs — are narrowed, limiting blood flow. Atherosclerosis is the most common cause. You may have leg discomfort that starts when you’re active and stops when you rest. Medicines, structured exercise therapy and procedures can prevent complications like limb loss.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
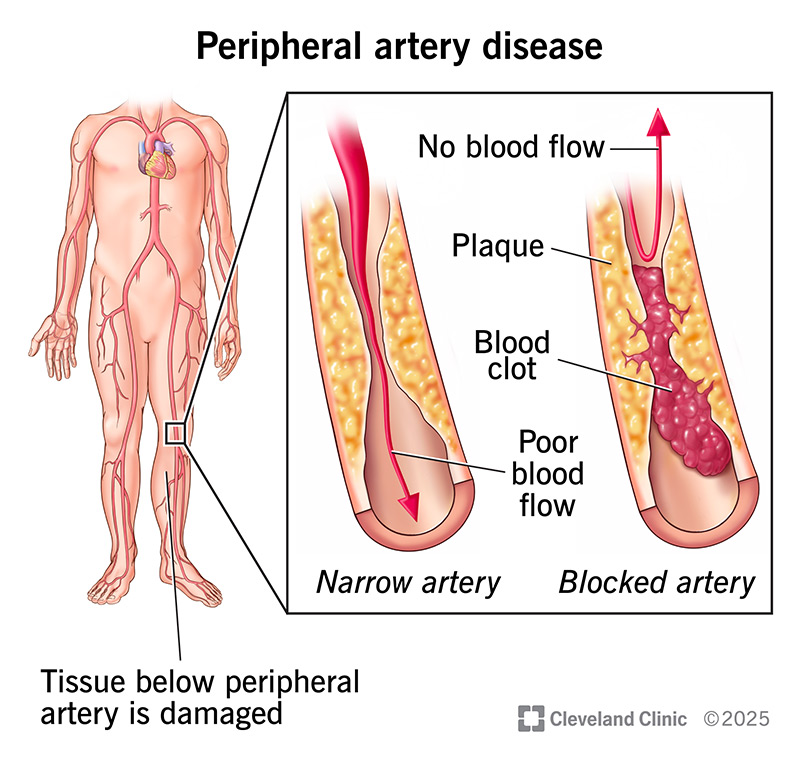
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17357-peripheral-arterial-disease-illustration-2)
Peripheral artery disease (PAD) is a vascular condition where arteries in your legs, pelvic area or arms become narrowed or blocked, usually due to plaque buildup. This limits how much blood can get through and may lead to symptoms like leg pain. This condition is treatable, especially when diagnosed early.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
PAD is common. It affects more than 200 million people around the world and around 12 million adults age 40 or older in the U.S. Anyone can develop peripheral artery disease, but your risk goes up with age. Black people face a higher risk compared to non-Hispanic white people, especially after age 50 (in males) and age 60 (in females).
Peripheral arterial disease is another name for this condition. While it can rarely affect your arms, PAD usually affects your butt, legs or feet. This form, sometimes called lower-extremity PAD, is the focus of this article.
Most often, the first symptom of PAD is leg discomfort when you’re active. This happens when your arteries can’t keep up with your muscles’ increased demand for blood. As PAD progresses, you may have leg or foot pain when you’re resting. But many people have no symptoms and are only diagnosed through screenings.
Possible symptoms include:
Advertisement
Exactly where you feel leg discomfort depends on which artery is too narrow. Symptoms occur below the affected artery:
Males might also experience erectile dysfunction related to peripheral artery disease when there’s narrowing of the lower aorta or iliac arteries.
The gradual buildup of plaque in your arteries (atherosclerosis) is the most common cause of peripheral artery disease. Your arteries are shaped like hollow tubes. They have a smooth lining that prevents blood from clotting and promotes steady blood flow. When you have PAD, plaque slowly forms inside your artery walls. This narrows the space where blood can flow.
Many plaque deposits are hard on the outside and soft on the inside. The hard surface can crack or tear. This allows platelets (disc-shaped particles in your blood that help it clot) to come to the area. Blood clots can form around the plaque, making your artery even narrower.
If plaque or a blood clot narrows or blocks your arteries, blood can’t get through to nourish tissues beyond that point. Those tissues may even start to die. This happens most often in your toes and feet.
Most people use “PAD” to refer to arteries that are narrowed from plaque buildup. But other things, besides plaque, can limit blood flow in your peripheral arteries. Less common causes of PAD include swelling in an artery (vasculitis) and repeated squeezing of an artery behind your knee (PAES).
You have a higher risk of getting peripheral artery disease if you have:
Research shows that smoking and diabetes are two of the strongest risk factors for PAD. People in these groups are two to four times more likely to develop PAD than people who don’t smoke or have diabetes.
If you have coronary artery disease or many risk factors for atherosclerosis, your provider may suspect you have PAD. This will lead them to order a screening test for PAD.
Without treatment, PAD can lead to limb loss. Most people with PAD don’t lose a limb. Providers do everything possible to avoid it. But if there’s enough tissue damage or your life is at risk, you may need surgery to remove your toe, foot or part of your leg.
Conditions like coronary artery disease and cerebrovascular disease often affect people with PAD. These aren’t direct complications. But they often occur together with PAD because plaque tends to build up in multiple spots, not just your leg arteries. That’s why treatment for PAD may also involve medicines to lower your risk of issues like a heart attack or stroke.
Advertisement
Your provider will perform a physical exam and review your medical history. They’ll ask about your symptoms, including what makes them start or end. Your provider will closely examine your bare feet. They’ll also feel your pulse in different areas of your leg.
Tests help your provider diagnose PAD and determine its severity. These include:
There are four main stages:
Advertisement
You may move among these stages over time. For example, your symptoms may suddenly get worse. Or treatment may improve your symptoms.
PAD treatment depends on how far the condition has progressed. If you don’t yet have symptoms or your symptoms are mild, medicines and changes to your daily habits may be enough. But your provider will keep a close eye on your condition and recommend further treatment as needed. If you have severe symptoms or are at risk of losing a limb, you’ll need a procedure or surgery.
Medicines for peripheral artery disease include:
Advertisement
Your healthcare provider may recommend you:
Taking good care of your feet is crucial with PAD. You should:
Your provider can give you more advice, too. It’s important to know that wounds that develop have a more difficult time healing. And infections are difficult to clear when there’s reduced blood flow to your foot.
If other treatments don’t help enough or PAD grows severe, you may need a procedure or surgery. Examples include:
Contact your provider if you:
You should also talk to your provider if you have any risk factors for PAD, even if you don’t yet have symptoms. Your provider may run tests to look for signs of blood flow issues. Early diagnosis and treatment can save your limb and your life.
Get immediate help if you can’t feel or move your foot or if it looks different from your other foot’s skin color. This means you’ve suddenly lost blood flow to your leg.
When you’re living with PAD, you can expect to have frequent follow-up appointments with your provider. These are key to catching signs of problems that need prompt treatment.
Peripheral artery disease is a lifelong condition. Although there’s no cure, you can keep it from getting worse by:
Quitting smoking is one of the best things you can do to improve your life expectancy. About 86 in 100 people who quit smoking after their PAD diagnosis live at least five more years. Of those who continue smoking, only 69 in 100 live at least five more years.
Hearing the word “peripheral” might make you think of something on the outer edges. Something that’s not at the center of your attention. You might even think it’s less important. But don’t let the name mislead you.
It’s true that peripheral artery disease affects arteries farther from your body’s center — like those in your legs and feet. But this doesn’t mean PAD is less important than other conditions, like coronary artery disease. In fact, it needs your attention just as much. Talk to your provider about how PAD is affecting you and how treatment can help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Plaque in your blood vessels can cause tingling, pain and numbness. Cleveland Clinic’s experts treat circulatory problems, including peripheral artery disease.
