An A1C test measures the average amount of sugar in your blood over the past few months. Healthcare providers use it to help diagnose prediabetes and Type 2 diabetes and to monitor how well your diabetes treatment plan is working.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_cpdiy60v/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn how the A1C test works and what the results mean.
An A1C test measures the average amount of glucose (sugar) in your blood over the past three months. The result is reported as a percentage. The higher the percentage, the higher your blood glucose levels have been, on average.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A1C is a simple blood test that healthcare providers use to:
Healthcare providers do A1C tests in one of two ways:
The vein blood test is generally more accurate than the finger prick blood test.
Other names for an A1C test include:
Glucose (sugar) mainly comes from carbohydrates in the food and drinks you consume. It’s your body’s main source of energy. Your blood carries glucose to all of your body’s cells to use for energy.
Several bodily processes help keep your blood glucose in a healthy range. Insulin, a hormone your pancreas makes, is the most significant contributor to maintaining healthy blood sugar.
Advertisement
If you have consistently elevated blood glucose levels (hyperglycemia) — and an elevated A1C result — it usually indicates diabetes. Diabetes develops when your pancreas doesn’t make any insulin or enough insulin, or your body isn’t using insulin properly.
If you have diabetes, you should have an A1C test two or more times a year to see how well your management plan is working. Your healthcare team will recommend exactly how often you should get this test.
If you don’t have a diabetes diagnosis, a healthcare provider may order an A1C test if you have symptoms of the condition, including:
You may also get an A1C test to screen for Type 2 diabetes if you’re at risk for the condition. Risk factors include:
A1C testing relies on hemoglobin. Hemoglobin is the part of the red blood cell that carries oxygen throughout your body. When you have glucose in your blood, it sticks to hemoglobin. This is called glycation. The more glucose is in your blood, the more it sticks. And it can stay there for around three months — about how long the average red blood cell lives.
The A1C test measures the average amount of glucose that’s been attached to hemoglobin over time. Because the A1C test measures glucose levels over a period of time, it provides more information about blood sugar than a single blood sugar test.
No, you don’t need to fast before getting an A1C test.
You can expect the following during an A1C test that involves a sample from your vein, or a blood draw:
You can expect the following during a finger prick A1C test:
Advertisement
Blood tests are a very common and essential part of medical testing and screening. There’s very little risk to having either type of A1C test. You may have slight tenderness or a bruise at the site of the blood draw or finger prick, but this usually resolves quickly.
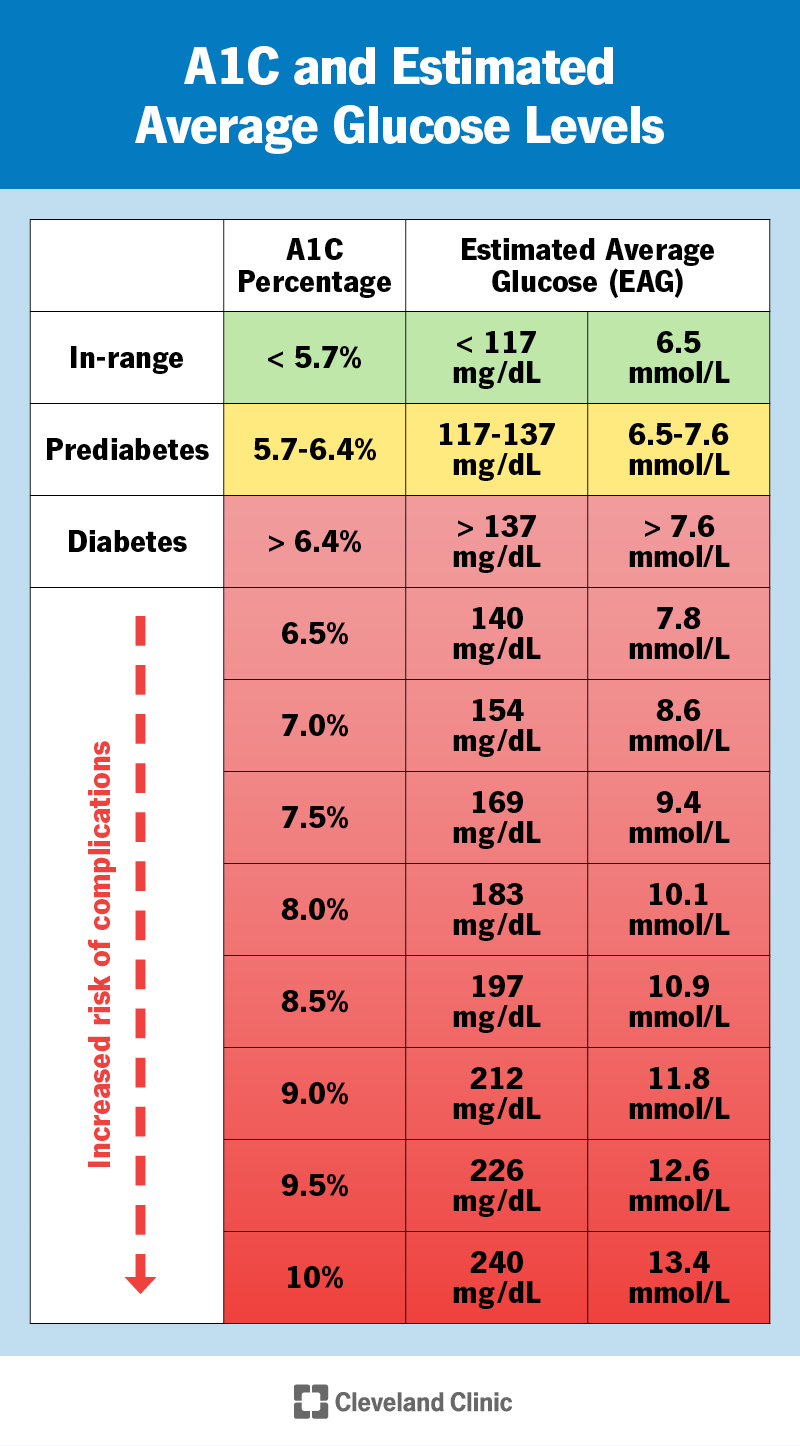
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9731-a1c-glucose-levels)
An A1C test result is reported as a percentage. The number represents the portion of hemoglobin proteins that are glycated, or holding glucose. The higher the percentage, the higher your blood sugar levels have been over the last few months.
For diagnosing purposes, an A1C level of:
If you already have diabetes, an A1C result is a glimpse into how well your management plan has been working over the last three months. Management may involve oral pills, taking insulin, monitoring blood sugar levels and/or lifestyle changes, such as diet and exercise. Your A1C can help you and your provider determine if you should adjust any part of your treatment plan.
It’s important to remember that your A1C (if you have diabetes) is just an average measurement of your blood sugar over a few months. It’s not a grade or the ultimate determiner of whether you’re living a healthy life. Know that your A1C will change over your lifetime and that there are steps you can take to improve your diabetes management and A1C level, if needed.
Advertisement
Some laboratories report your A1C results as a percentage in addition to the corresponding estimated average glucose (eAG).
The eAG calculation converts the A1C percentage to the same units you use with at-home glucose meters (glucometers) — milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). Just like your A1C is an average, the eAG is a single number that represents your average blood sugar level over the past three months.
For example, an A1C level of 7% equates to an eAG of 154 mg/dL (8.6 mmol/L). An A1C level of 9% equates to an eAG of 212 mg/dL (11.8 mmol/L).
For people without diabetes, a normal A1C is below 5.7%.
For people with diabetes, what’s “normal” and healthy for you depends on your goals and access to diabetes management medication and tools. Together, you and your healthcare provider will determine an A1C range that should be your target goal. This will likely change throughout your life.
In general, the American Diabetes Association recommends that the goal for most adults with diabetes should be an A1C of 7% or lower.
Your A1C goals may be above 7% if you have:
Advertisement
On the other hand, healthcare providers typically recommend that people with Type 1 diabetes who are pregnant try to maintain an A1C of 6.5% or lower throughout their pregnancy. This is to try to lower potential health risks for the fetus and to try to prevent fetal macrosomia.
The higher your A1C levels, especially if they’re consistently high over several years, the more likely you’ll develop complications, such as:
Studies have shown that people with diabetes may be able to reduce the risk of diabetes complications by consistently keeping their A1C levels below 7%.
It’s important to remember that other factors can contribute to the development of diabetes complications, such as genetics and how long you’ve had diabetes.
Certain factors can affect the accuracy of A1C tests, including:
These factors can make your result falsely low or falsely high. Most of the factors are due to differences in the lifespan and health of your red blood cells.
Hemoglobin variants can affect the results of some A1C tests.
The form of hemoglobin in your blood depends on the genes you inherit from your biological parents. There are many different forms. The most common form is hemoglobin A. Other, less common forms of hemoglobin are called hemoglobin variants.
A hemoglobin variant doesn’t increase your risk of developing diabetes, but it can affect A1C results. Labs have different ways to do A1C tests on blood with a hemoglobin variant.
The most common variants include:
A blood test can detect hemoglobin variants. Talk to your healthcare provider if you think you might have a hemoglobin variant that could affect your A1C results.
The following conditions and situations can cause falsely low A1C results, meaning the result is lower than your actual A1C level:
The following conditions and situations can cause falsely high A1C results, meaning the result is higher than your actual A1C level:
If you have an elevated A1C (above 6.5%) for the first time, it doesn’t always mean that you have diabetes. Other factors, such as certain medications (like steroids) or sickness can temporarily increase your blood sugar levels. Anemia and other conditions can cause a falsely high A1C result, as well. There also could’ve been an error in the collection, transport or processing of the test.
Healthcare providers rely on more than one test to diagnose diabetes. For example, they may order a fasting blood glucose test or another A1C test. In any case, your provider will carefully interpret your results and discuss them with you.
For decades, healthcare providers and people with diabetes have relied on A1C as the main way to gauge how well their management of the condition is working.
For people with Type 1 diabetes, in particular, blood sugar can fluctuate significantly throughout the days, weeks and months. Because of this, A1C isn’t always an accurate measurement of management since it’s based on an average.
For example, a person who has frequent blood sugar fluctuations between significantly low and high episodes may have an A1C of 7%. A person who has blood sugar levels that stay more consistently around 154 mg/dL may also have an A1C of 7%.
More recently, with the invention of continuous glucose monitoring (CGM) devices, providers and people with diabetes have found time in range (TIR) to be a more helpful and accurate representation of diabetes management.
Time in range is the amount of time your blood sugar levels are in a recommended target range. TIR is measured as a percentage. Blood sugar range goals can vary for each person, but a typical target range is between 70 and 180 mg/dL. For most adults with Type 1 or Type 2 diabetes, providers recommend aiming to have a TIR above 70% (about 17 hours of a 24-hour day).
With CGMs and TIR, providers and people with diabetes can see how often they’re experiencing high or low blood sugar episodes. This can help them more accurately adjust treatment strategies.
It can be stressful to see an abnormal or higher-than-you-expected A1C result. Know that having an elevated A1C for the first time doesn’t necessarily mean you have diabetes. Several factors can cause inaccurate results. Your healthcare provider will let you know if you need to undergo further tests. Don’t be afraid to ask your provider questions. They’re available to help you.
If you have diabetes, it’s important to remember that your A1C is just a temporary average of your blood sugar levels. Know that there are steps you can take to change your A1C level. If you’re feeling overwhelmed with diabetes management, talk to your healthcare provider. Together, you can formulate a plan to get closer to your management and A1C goals.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Whether you’ve been living with diabetes for years or you’re newly diagnosed, you want experts you can trust. Our team at Cleveland Clinic is here to help.
