Insulin pumps can help people with diabetes conveniently manage their blood sugar. These small, wearable devices deliver doses of insulin at specific times and are an alternative to multiple daily injections. There are several types of insulin pumps on the market, each with unique features.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
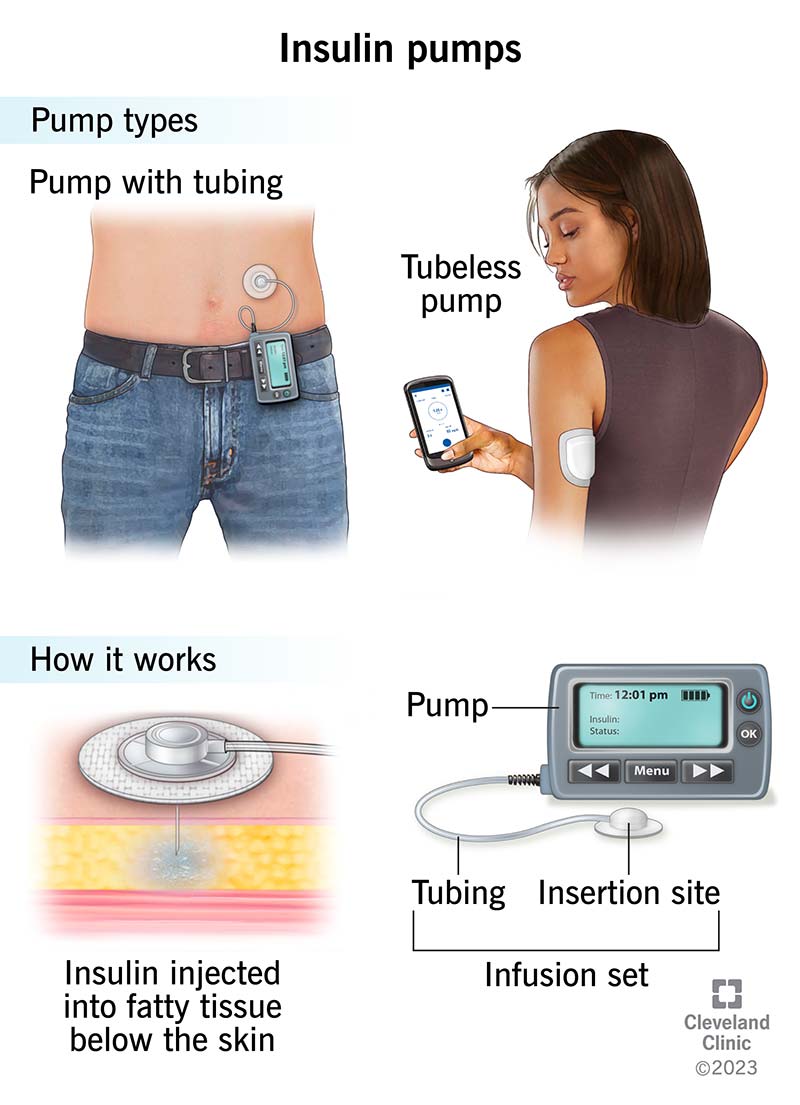
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9811-insulin-pumps)
An insulin pump is a wearable medical device that supplies a continuous flow of rapid-acting insulin underneath your skin. Most pumps are small, computerized devices that are roughly the size of a juice box or a deck of cards.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Insulin pumps are an alternative to multiple daily injection (MDI) insulin therapy (syringe or pen injections) for people with diabetes who require insulin to manage the condition.
The technology for insulin pumps is rapidly evolving. All pumps available in the United States today integrate with CGM (continuous glucose monitoring) technology and offer the ability to automatically adjust your insulin needs based on your current glucose levels.
An insulin pump mimics how your pancreas would naturally release insulin. It delivers insulin in one of two ways:
Advertisement
Each type and brand of pump has various settings and technology. Examples include:
There are two main types of insulin pumps: those with tubing and those without tubing.
As its name suggests, a tubed (tethered) insulin pump has a long, thin tube that connects the pump itself to a cannula under your skin to deliver insulin. Parts of a tubed insulin pump include:
You should change most reservoirs and infusion sets every two to three days. You must change your reservoir if it runs out of insulin. You use new infusion sets, reservoirs and tubing every time. But the pump itself typically lasts for multiple years.
While some tubed insulin pumps are waterproof, people typically disconnect them from the infusion site when they take a shower, bathe or swim. You can then reconnect the pump and tubing to the infusion site afterward. Some tubed pumps are just water resistant, not waterproof.
Tubeless insulin pumps (patch pumps) also use a flexible plastic tube (cannula) under your skin. But the insulin reservoir and the cannula are part of one “pod” that sits on your skin with an adhesive patch. There’s no external tubing. You then operate the pump wirelessly with a handheld controller.
You use each pump — or pod — one time. Like a tubed pump, you change it every two to three days and must change it if the reservoir runs out of insulin.
Before attaching the pod, you fill the reservoir with insulin and attach the adhesive to your skin. You then push a button that releases a needle that’s threaded through the cannula in the pod. The needle retracts back into the pod, and the cannula remains under your skin. You can wear the pump on your upper arm, belly, hip, buttock or thigh.
Advertisement
Tubeless insulin pumps are waterproof, so you can bathe and swim with them on.
Brands of insulin pumps currently on the market in the United States include:
Another tubeless pump, the Accu-Chek® Solo Micropump System, is only available in the United Kingdom but is awaiting U.S. FDA approval.
Anybody with diabetes who requires synthetic insulin may use an insulin pump. This includes people with Type 1 diabetes — both children and adults — and some people with Type 2 diabetes. People with Type 3c diabetes or monogenic diabetes may use a pump, as well.
Each insulin pump has different Food and Drug Administration (FDA) approvals regarding how old you can be to use it. Some insulin pumps have approval for children as young as 2. Most other pumps have approval for people 7 years and older.
Insulin pumps are one insulin therapy option for diabetes management — they’re a personal choice. You may want to use an insulin pump if you (or your child):
Advertisement
Insulin pumps aren’t the best option for everyone — for a variety of reasons. Some things that may not make you or your child an ideal candidate for an insulin pump include:
Compared to multiple daily injections, the benefits of an insulin pump include:
Advertisement
Most endocrinologists and diabetes specialists encourage the use of insulin pumps due to their evidence-based benefits.
A significant disadvantage of insulin pumps — compared to multiple daily injections — is insulin delivery issues. These can happen for a variety of reasons, including:
In some cases, your insulin pump will recognize that there’s a blockage (occlusion) and will alert you to change the pump or infusion set. In other cases, like if your set becomes disconnected from the tubing, the pump can’t recognize the issue. If you use a CGM, you may notice an insulin delivery issue if your glucose level rises for an unexpected reason.
If you go without insulin for a certain amount of time — typically hours — it increases your risk of severe high blood sugar (hyperglycemia) and diabetes-related ketoacidosis (DKA), which is life-threatening.
Because of insulin delivery issues, it’s important to always have a backup plan if you use a pump and act fast. This may look like:
To try to prevent these issues or catch them early, get in the habit of checking your pump and/or infusion set at least once a day. It’s also important to monitor your blood sugar levels regularly.
Other factors that you might see as disadvantages of insulin pumps include:
There are countless factors to consider when choosing an insulin pump. And it’s a big decision. The good news is that pump manufacturers have lots of information on their pumps as well as trainers that can answer your questions. Your diabetes healthcare provider can also be a great resource.
Some things to consider and ask when choosing a pump include:
Insulin pumps can offer a flexible option for insulin delivery. Many people with diabetes find insulin pumps to be more convenient than injections. It’s important to remember that insulin pumps aren’t permanent. You can change your mind and return to injections if you don’t like using a pump. It may be overwhelming to choose from the variety of pumps on the market. But know that your diabetes healthcare provider will help you make the best decision for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you’ve been living with diabetes for years or you’re newly diagnosed, you want experts you can trust. Our team at Cleveland Clinic is here to help.
