Type 1 diabetes is a chronic (lifelong) autoimmune disease that causes a lack of insulin, an essential hormone. It requires daily management with insulin injections and glucose monitoring. Both children and adults can be diagnosed with Type 1 diabetes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_43wexdqi/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn what causes Type 1 diabetes and ways you can treat it.
Type 1 diabetes (T1D) is a lifelong autoimmune disease that prevents your pancreas from making insulin, a hormone. T1D was previously known as juvenile or insulin-dependent diabetes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you don’t have enough insulin, too much sugar builds up in your blood, causing hyperglycemia (high blood sugar). This can lead to serious health problems or even death if it’s not treated.
T1D is one of the most common chronic diseases that affects children in the U.S. But adults can develop it, too. In the U.S., over 1.7 million people live with it.
Receiving this diagnosis is a life-changing event. But many tools and technologies can help you manage T1D. Healthcare providers will be by your side, too.
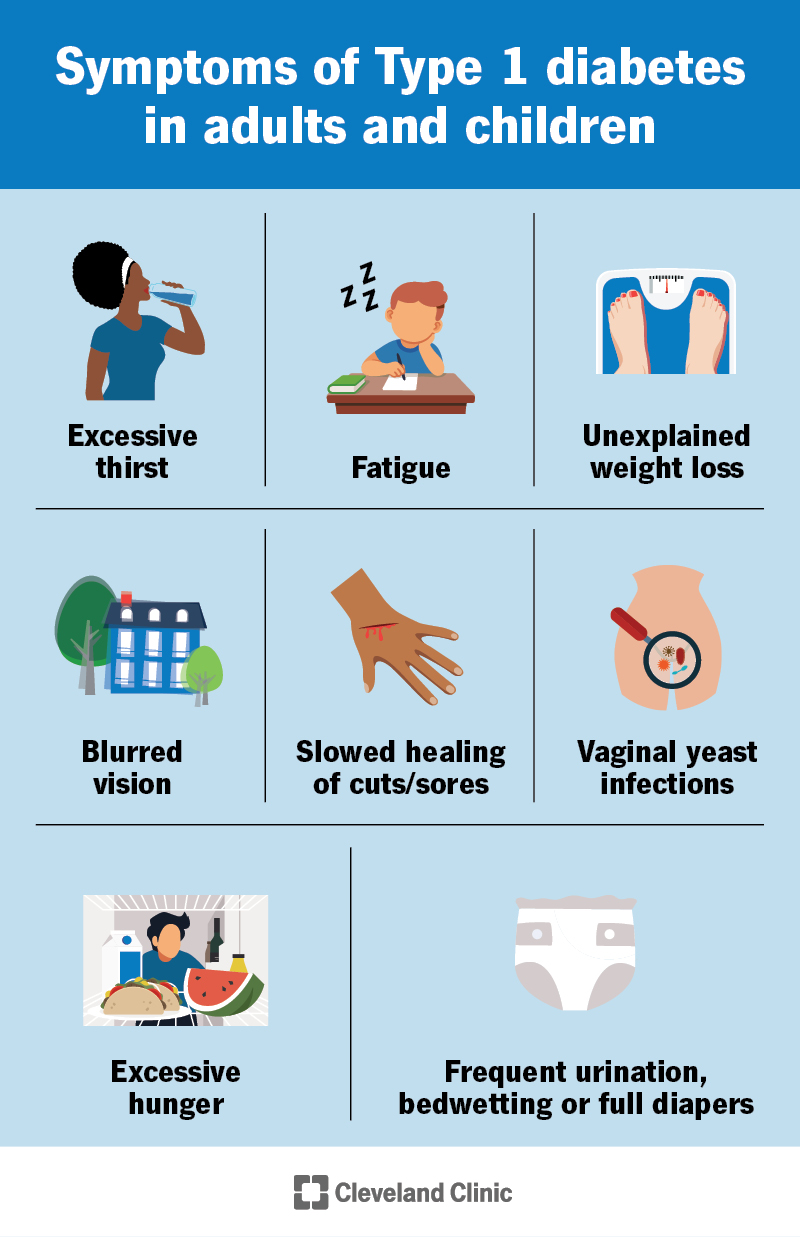
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21500-type-1-diabetes)
Type 1 diabetes symptoms include:
Symptoms usually start mild and get worse over days, weeks or months. If you have these symptoms or notice them in your child or family member, see a healthcare provider as soon as possible. Ask to be tested for Type 1 diabetes.
Emergency signs of undiagnosed T1D from a complication called DKA include:
Go to the emergency room immediately if you have these symptoms. DKA is life-threatening.
Advertisement
Scientists don’t know the exact cause of Type 1 diabetes. It happens when your immune system mistakenly attacks the insulin-making cells in your pancreas. But they don’t know why this happens. The destruction ultimately results in a total lack of insulin.
Studies show that genetics likely play a role. The odds vary based on the genetic connection. Your risk of developing Type 1 diabetes is:
Certain factors, like a virus or environmental toxins, may trigger your immune system’s attack if you have a genetic predisposition for T1D.
Over time, continuous high blood sugar can damage many parts of your body. Potential complications of T1D include:
Close to half of people with Type 1 diabetes will develop a serious complication over their lifetimes. But consistently keeping your glucose in range can help prevent these issues. If you reach the first 20 years after diagnosis without any complications, your prognosis (outlook) is usually good.
People with diabetes are also two to three times more likely to have depression and are 20% more likely to be diagnosed with anxiety than those without diabetes. Taking care of your mental health — and getting professional help when needed — is key.
Type 1 diabetes is usually easy to diagnose. Your healthcare provider will use the following tests:
Your provider may do the following tests to check your overall health and for DKA:
You’ll need to take insulin several times a day to manage Type 1 diabetes. Keeping your blood sugar in range is key. Several factors affect your glucose level. So, T1D management is complex and highly individualized.
Advertisement
An endocrinologist and other diabetes specialists will help you set the framework for treatment. But T1D is mainly a self-managed disease. You’ll make several decisions every day to stay healthy.
The main components of management include:
There are several different types of insulin. They start working at varying speeds and last for different lengths of time. You may need to use more than one type.
You’ll have a background level of insulin (often called basal insulin or long-acting insulin). And you’ll need to give yourself specific amounts of it when you eat and to correct high blood sugar levels.
You can take insulin in the following ways:
Advertisement
The amount of insulin you need from day to day will vary across your lifespan and under specific circumstances. For example, you typically need more insulin during puberty, pregnancy and when you’re taking a steroid medication.
Too much insulin at any given time can lead to low blood sugar. This needs treatment right away — often by eating or drinking sugar.
You’ll need to monitor your glucose level closely throughout the day. You may use a blood glucose meter and/or continuous glucose monitoring (CGM).
Your healthcare provider will give you a target glucose level range or time in range (TIR) to aim for. The right range for you depends on a variety of factors.
Some CGMs and insulin pumps can pair together to create a hybrid closed-loop system. The pump automatically gives you insulin based on your glucose level to keep it in range. But this system isn’t totally automatic. You still have to provide input to the pump in certain situations.
Type 1 diabetes and glucose management are very complex. Because of this, you and your family will need to learn a lot. Most of the education will be right after diagnosis. But you’ll likely learn more as you continue to live with T1D. Especially as your body or life changes.
Advertisement
A team of healthcare providers will help you understand all the aspects of T1D. Education topics include:
There’s currently no cure for Type 1 diabetes. But scientists are working on ways to prevent or slow down the progression of the condition through studies like TrialNet.
T1D can run in families. So, your healthcare provider may be able to test your family members for the autoantibodies that cause the disease. Type 1 Diabetes TrialNet also offers this testing.
The presence of autoantibodies, even without diabetes symptoms, means you’re more likely to develop the condition. If someone has early signs of the autoantibodies, they may be able to take a medication that delays T1D. It’s called teplizumab. It can delay the development of T1D symptoms and the need for insulin injections. It’s an infusion you get once a day over several days.
Two types of transplants may “cure” T1D. But they come with significant risks, like surgery complications and health risks involved with taking immunosuppressants. Providers only approve them for a small number of people with T1D. The transplants include:
You’ll need to see your endocrinologist multiple times a year throughout your life to adjust your management plan. Otherwise, reach out to your diabetes provider if you:
With Type 1 diabetes, you must make countless decisions every day to stay healthy. It’s a complex condition that requires a lot of effort and planning. This can be tough. But it’s also very doable with the right diabetes technology, education and healthcare providers by your side. Getting support from your family and friends is a big help, as well.
You’ll need to prioritize both your physical and mental health to stay healthy in the long term. Maintaining in-range blood sugar levels is key to preventing serious complications.
Getting a Type 1 diabetes diagnosis may drastically change the life you imagined. But it’s still possible to do what you love and live a healthy life with T1D. It’ll take extra planning, education and support. You’ll likely be very overwhelmed at first. After all, you’re manually doing the work of a body system that’s automatic for everyone else. But over time, you’ll get a better grasp on how to manage the condition. And you’ll become more in tune with your body. Lean on your village and healthcare providers for help. They want to see you thrive.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Type 1 diabetes can affect your life in many ways. At Cleveland Clinic, we can help develop a treatment plan that matches you and your goals.
