If you have diabetes, you’re at risk of developing diabetes-related macular edema, a type of diabetes-related eye disease. If you have dark spots, blurred vision or double vision, see your eye care provider. Early treatment is best.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
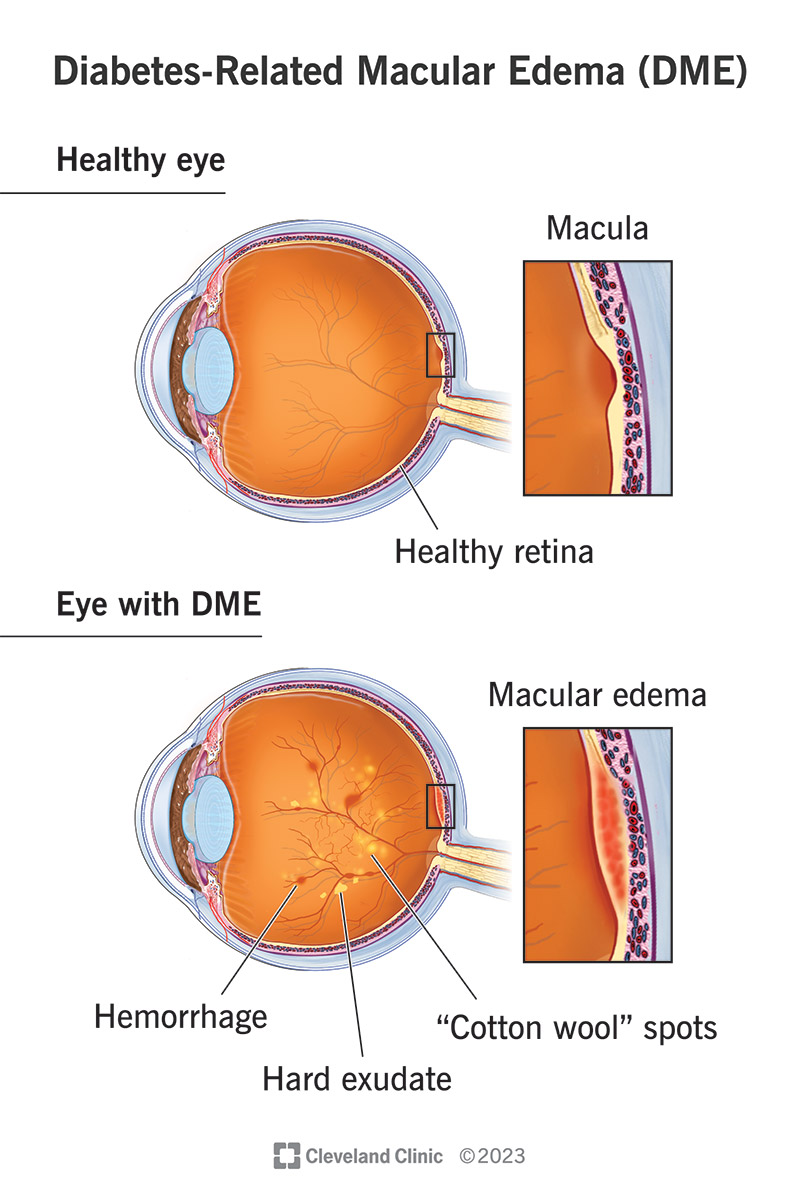
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24733-diabetes-related-macular-edema)
Diabetes-related macular edema (DME) is swelling in the macula, or central, part of the retina of your eye. Your retina is in the back of the eye and is the part of your eye that houses the light-sensing cells. Your macula lets you see fine details.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You can get DME if you have diabetes-related retina disease (diabetes-related retinopathy). Diabetes affects the blood vessels in your eyes, making them weaker and more likely to leak blood. It may also cause new and more fragile blood vessels to grow where they shouldn’t grow.
About 1 in 14 people with diabetes develop diabetes-related macular edema. In the U.S., more than 37 million adults have diabetes currently.
The signs and symptoms of diabetes-related macular edema may include:
Diabetes-related macular edema happens when high blood sugar levels affect the blood vessels in your eyes. Your blood vessels leak, which causes fluid to build up and thicken your retina.
Issues with blood vessels happen to people who have diabetes-related retinal disease or diabetes-related retinopathy (DRR). Blood vessels become weak and form pouches. The pouches leak. This is non-proliferative DRR.
If you begin to grow new blood vessels in your eyes that don’t belong there, you have proliferative DRR. These new blood vessels aren’t as strong as they should be, so they also leak and allow blood to build up in your macula and retina.
Advertisement
A serious complication of untreated diabetes-related macular edema is vision loss.
You can’t see swelling in your retina, but your eye care specialist can see this when they do a thorough eye examination. This is one reason that you need to have regular eye exams. Following an eye exam schedule is especially important if you have diabetes.
In addition to the eye exam, which includes a slit lamp exam, your provider may use the following tests to diagnose and monitor DME:
Treatment options for DME have improved. In fact, some newer medications work well enough to reverse the damage in some cases.
One form of treatment blocks vascular endothelial growth factor (VEGF), a protein that helps new blood vessels grow. Steroids that manage inflammation are another form of treatment that’s applied to your eyes.
In addition, your provider will work with you to manage your blood sugar levels and your blood pressure. This process might involve other types of medications.
One of the ways that providers treat DME is with a series of intravitreal injections of medications (shots into the vitreous humor of your eye). These medications include:
Ozurdex and Iluvien are steroid implants that your provider injects into your eye.
Providers may use laser therapy (photocoagulation) to seal the blood vessels in your eyes to stop the leakage.
Another procedure that your provider might suggest is a vitrectomy. This surgery can remove scar tissue and cloudy vitreous fluid from your eye.
The chance of complications with DME treatments is low, but there are always risks, such as infection, when anything penetrates your eye.
Other potential complications could be that you develop air bubbles in your eyes after the injections. These air bubbles will be similar to floaters and resolve within a few days.
Likely side effects of injections include eye redness and irritation, which can be from the cleaning solution used prior to the injection to reduce infection risk. Using artificial tears on the day of injection can help with irritation.
Advertisement
Steroid treatments may have additional complications, such as cataracts or higher eye pressure (intraocular pressure).
Normally, you don’t have pain with diabetes-related macular edema, so you won’t really “feel better” after having injections. The treatments should stop or reverse damage to your macula, retina and vision. You don’t have to wait to go back to work or school.
Recovering from a vitrectomy will take longer than other therapies. You’ll need to take off for two to four weeks.
If you have DME and you have successful treatments, your outlook is good. Some of the newer medications seem to restore some lost vision, but this is primarily when your provider can diagnose and treat DME early.
Without treatment, DME can result in a significant loss of vision, which could have an impact on the way that you live your life.
You may be able to reduce your risk of developing diabetes-related macular edema by:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_hii8rqwl/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn how nutrition can help slow the progression of diabetes-related macular edema.
Although DME is a condition that affects your eyes, you can help yourself by taking care of your entire body.
Advertisement
Diabetes is a disease that can affect so many parts of your body, including your eyes. If you have diabetes and diabetes-related retinopathy, you’re at risk of developing diabetes-related macular edema. This is especially true if you’ve had diabetes for a long time. It’s so important to have regular eye exams so your provider can find swelling or new blood vessels early. Early diagnosis and treatment are crucial to protecting and preserving your eyesight. Early treatment may be able to reverse damage from diabetes-related macular edema.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Your eyes are one of your most important senses. If something goes wrong, it can change your world. Cleveland Clinic can help treat all types of retinal disease.
