One Researcher’s Mission to Outsmart Brain Cancer

Jennifer Yu, MD, PhD, sums up the work of her laboratory in one sentence: “We study cancer stem cells and try to find ways to kill off these cells more effectively.”
Dr. Yu, who works in Cleveland Clinic Lerner Research Institute’s Department of Stem Cell Biology and Regenerative Medicine, studies glioblastoma, a fast-growing and aggressive form of brain cancer. “We’re figuring it out from all angles,” she says. “Cancer cells can be very sneaky. They try to exploit any advantage they can find, so we have to look at things from many different perspectives.”
She focuses her attention on glioblastoma stem cells, explaining that they’re like the queen termite in a termite colony. “You can kill off the termites but unless you kill off the queen, the colony will just keep coming back.” Because the stem cells are so invasive, they cannot be removed completely by surgery. And because they have found ways to survive radiation and chemotherapy, the cancer stem cells remain behind. Inevitably, the cancer returns in six to nine months, Dr. Yu says.
Research shows that cancer stem cells have certain properties that other cancer cells don’t. They have the ability to self-renew, become different types of cells and are highly resistant to traditional therapies such as radiation and chemotherapy.
Why Do Cancer Stem Cells Thrive?
Scientists have found that cancer stem cells reside in certain areas of a tumor that are hypoxic, meaning that blood circulation and oxygen levels are low, rendering chemotherapy and radiation less effective.
“The hypoxic microenvironment makes these cells more difficult to treat,” Dr. Yu says. “Additionally, the cancer stem cells themselves are more efficient at repairing damage from radiation, and they have found ways to pump out chemotherapy.”
She and her team are studying how hypoxia drives cancer progression and resistance to treatments. They’re working to identify the missing link between glioblastoma stem cells, hypoxia and a pro-cancer cell signaling pathway called Notch, which promotes stem cell survival.
The team found that a protein called vasorin—induced in low-oxygen settings—was abundant in patients with aggressive gliomas and was associated with poorer survival.
Next, the team studied vasorin in cell culture to determine how it affects glioblastoma progression. Under normal conditions, an adaptor protein binds to and inhibits the pro-cancer Notch pathway. However, the researchers discovered that in the hypoxic environment, the abundant vasorin would instead bind to and increase the Notch signaling pathway within the glioblastoma stem cells, leading to unchecked tumor growth.
The team tested their theory in a preclinical model that showed blocking vasorin led to reduced Notch signaling. “More studies are needed, but perhaps inhibiting vasorin can be used in conjunction with radiation therapy or chemotherapy to target the cancer stem cells more effectively," Dr. Yu says.
Using Technology to Target Cancer Stem Cells
Dr. Yu’s lab also is using technology in the quest to understand glioblastoma stem cells. Her team is studying the effects of hyperthermia, a noninvasive method of increasing tumor temperature that works to stimulate blood flow, increase oxygenation and make tumor cells more responsive to radiation.
“We’re trying to understand the molecular mechanisms by which hyperthermia can sensitize a cancer stem cell to radiation,” she says. “Hyperthermia can act on the cancer stem cell itself, and it may also augment the immune response so that the body can fight off the cancer more effectively. In fact, a clinical trial based on these concepts is now underway in glioma patients.”
Dr. Yu hopes to take advantage of the effects of hyperthermia treatment by compressing the time frame in which chemotherapy, radiation and surgery are performed. She says that, eventually, she’d like to do additional clinical trials that include targeted therapies based on the molecular features of each patient’s tumor.
“Once we figure out how best to sequence things and what the best combination treatment is, we could make more of an impact in patient care,” Dr. Yu says.
No Guarantee of Funding
Like many researchers, Dr. Yu is concerned about financial support for her lab. Even though the federal government is the largest funding source for medical research, she says that less than 10 percent of requests are successful in obtaining grants from the NIH, and only about 8 percent from the National Cancer Institute.
“Laboratories are structured differently from clinical departments in the sense that they exist primarily because of grant funding,” she says. “All the people in my laboratory – four postdocs and one technologist – their salaries and projects are funded by grant monies. There is no guarantee it will continue.”
She feels fortunate that her lab has been successful in getting funding but says she always is looking for more support, either from the NIH, private philanthropy or foundations.
“Being able to devote energy to take on high-risk, high-yield projects is important,” she says. “It can take over a year to develop the data required for a competitive NIH grant application. Unfortunately, many talented, young scientists are deterred from going into research fields because of the uncertainty of funding.”
Dr. Yu devotes her work to brain tumor research and glioblastoma, in particular, because she feels those patients need help. “We’ve made so little progress in the last 40 years, and if you think about a cancer population that really needs to do better, the glioblastoma patients are the ones.
“I’m hopeful that we’ll be able to make some big strides with this cancer. With each step, we are that much closer to finding a cure.”
How You Can Help
Your support of innovative medical research like Dr. Yu’s makes a difference in so many ways. Please help our researchers continue their groundbreaking discoveries by making a gift today. Contact Katie Contrera at 216.445.6299.
Parkinson’s: New Insights after 200 Years

Although Parkinson’s disease first was identified in 1817 by London physician James Parkinson, researchers are only beginning to understand its complexities.
“It is not a one-size-fits-all illness. We now know there are numerous subtypes and many, many presentations of Parkinson’s,” Cleveland Clinic neurologist Hubert Fernandez, MD, says. “There are several disorders that have gone through these iterations – breast cancer, for example. Scientists learned that there are different types of breast cancer that need to be treated in different ways. We’re slowly getting into that realm with Parkinson’s.”
He says that current methods of evaluating and monitoring the symptoms of Parkinson’s disease and its progression are highly subjective and lack standardization. He believes that a critical analysis of Parkinson’s leads to the accelerated development of specific therapies to identify and target different clusters and subtypes of the disease.
Getting to the Next Level with Technology
Dr. Fernandez, Director of Cleveland Clinic’s Center for Neurological Restoration, and his team are investigating advanced technologies and working to develop groundbreaking therapies and assessment tools. His research will build on information from PD Optimize, a platform technology that is already developed.
PD Optimize is collecting data from more than 20,000 patients to evaluate their motor and non-motor functions. It uses eight modules to evaluate symptoms of the disease, including tremor, bradykinesia, gait and postural stability, manual dexterity, and processing speed, as well as non-motor symptoms such as working memory, set-switching, depression and quality of life. One unique module tracks a symptom that the patient has identified as the most bothersome. The data is integrated into each patient’s electronic health record, which enhances physician-patient interaction.
The Impact of Accurate Data
Dr. Fernandez and his team are working to expand the PD Optimize technology for large-scale clinical use, along with the development and incorporation of a mixed-reality based tool. He envisions that patients will wear the device in their homes or workplaces to objectively and continuously gather data about their balance, gait and cognitive problems during their normal daily activities. Currently, data is gathered artificially through task-based testing at a doctor’s office. Dr. Fernandez anticipates that this device, that takes a peek into their natural state, would increase the accuracy, duplication and reliability of data from patients. It, along with PD Optimize, would help in categorizing disease clusters and allow physicians and scientists to predict outcomes more accurately.
Results gathered through this mixed-reality based tool would impact other Parkinson’s research, particularly the development of cognitive-sparing deep brain stimulation (DBS), which electrically modulates the parts of the brain that are responsible for movements caused by the disease.
“The best opportunity to readjust DBS setting for cognitive changes is before these cognitive changes are even noticeable to the patient or family and more likely to be reversible,” Dr. Fernandez says.
Doing More With Less
“As we learn more about the nuances and complexities of Parkinson’s, we’re also learning about the enormous variations in how it presents and how it progresses,” Dr. Fernandez says. “Unfortunately, we’re in the era of needing to provide the most cost-effective care to all citizens, meaning doctors are asked to do more and more in less and less time. In other words, as our understanding of Parkinson’s is becoming more complex and demanding us to look at multi-organ systems and treat the patient as a whole, our economy is telling us to be leaner and more efficient, and view patients as populations, not as individuals.”
But he hopes that because this research is based on technology and the digitization of data, his ideas can be implemented.
“Digitization allows us to practice precision medicine in a very effective manner, which is the best of both worlds. Technology can help us bridge that gap.”
How You Can Help
Philanthropic partners can provide the critical financial support that allows our scientists to take risks on new concepts while expanding or accelerating promising ideas. Contact Kristie Burke at 216.445.9412 to contribute.
Your Brain’s Annual Physical
Sometime in the not-so-distant future, a routine doctor’s visit could include a brain health assessment along with the usual blood pressure and weight checks.
Patients would complete a series of brief cognitive tests on a tablet computer while waiting to see their doctor. It would be like playing a game on an app — for example, matching a symbol against its corresponding number in a key.
More than a game, this brain health app would give doctors objective data about the cognitive functioning of their patients. It could be particularly helpful for those who are in the preclinical stage of Alzheimer’s disease, when subtle brain damage can occur.
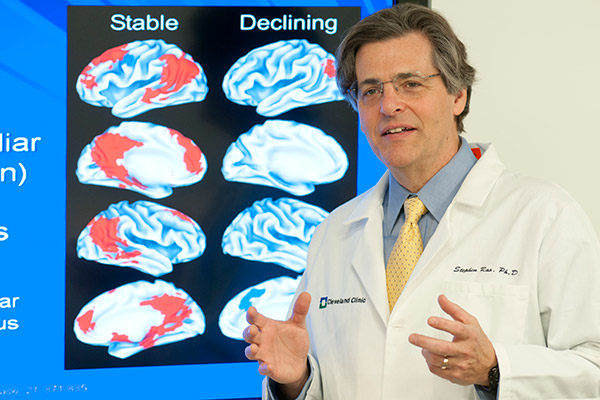
“We know that the pathological changes precede the diagnosis by as much as 10 to 15 years,” says researcher Stephen M. Rao, PhD, who holds the Ralph and Luci Schey Endowed Chair at Cleveland Clinic’s Lou Ruvo Center for Brain Health. “But how do you define these people?”
A Case for Early Intervention
Existing tests, such as MRI, genetic testing and PET scans, are either non-definitive or too costly to give to every patient. And yet the ability to identify preclinical changes in a person’s brain has greater value than just early diagnosis.
“What we’re interested in seeing is if we can prevent or slow down the disease early on before significant brain deterioration has occurred,” Dr. Rao says. “If we can delay the onset of Alzheimer’s by just five years, we cut the number of people who have it by half. If we delay it by 10 years, we practically wipe out the disease.
“Early intervention is where it’s at. The whole field is moving in that direction.”
He says that many Alzheimer’s drugs have failed because they’re given to people who have had the disease for more than a decade.
“A lot of neurons are lost. So if we can intercede early on, either through some kind of lifestyle change, such as increasing physical activity, or a drug designed to change the course of the disease, interventions that don’t work in people diagnosed with Alzheimer’s may work in people who are in the preclinical stage.”
Partners in a New Care Model
Dr. Rao developed the app with Jay Alberts, PhD, holder of the Edward F. and Barbara A. Bell Family Endowed Chair at Lerner Research Institute’s Department of Biomedical Engineering and Vice Chair of Innovation within the Neurological Institute.
Having patients take a 15-minute memory and cognitive battery on an iPad prior to their annual checkup represents a new model of care for Alzheimer’s. “This technology will create a waiting room of the future in which the visit starts as soon as they step in the office,” Dr. Alberts says.
Dr. Rao, who has been studying Alzheimer’s for over two decades, says that he’s not aware of any other hospitals doing this. “There are a lot of computerized cognitive tests out there, but nobody’s integrating it into primary clinical care.”
The goal of such low-cost screening is to make brain health testing as routine as checking your blood pressure and weight. Dr. Rao is working with Lori Posk, MD, FACP, Medical Director for Cleveland Clinic MyChart and of the Twinsburg Family Health & Surgery Center, to introduce the app in Twinsburg.
An example of the screening used to identify people who have subtle cognitive deficits and follow up with further testing to see if they have imaging and cerebrospinal fluid biomarkers that are suggestive of early Alzheimer’s disease.
“If all goes well,” Dr. Rao says, “we will begin screening persons between 65 and 80 early next year. What we want to do is start identifying the people who have subtle cognitive deficits and follow up with further testing to see if they have imaging and cerebrospinal fluid biomarkers that are suggestive of early Alzheimer’s disease.”
Dr. Posk is enthusiastic about the project. “Patients are often asking how they can be tested and identified if they are at risk early on,” she says. “I look forward to having a set of tools in addition to the physical exam and history to identify my patients early.”
Become a Champion of Brain Health
Dr. Rao recently received $8.75 million in funding from the National Institute on Aging (NIA) to investigate why exercise is good for the brain in persons at risk for Alzheimer’s. But the work being done by Dr. Rao’s team to integrate the brain health app into primary care clinics and the electronic health record is not funded, so philanthropic support is needed.
“There are costs associated with programming and development, and also for developing norms for our tests so we can adjust the scores based on participants’ age and lev-el of education,” he says. “So covering the actual costs of getting it into the clinic would be appreciated because NIA will not support such costs.”
Dr. Rao started his career researching multiple sclerosis. He and Dr. Alberts already have had success with an app they developed to assess the cognitive, motor and vision functions of MS patients. Cleveland Clinic’s Mellen Center tests patients before each appointment, and other major MS centers around the world are planning to put the app into use this year.
Much of the cost of developing the MS app was borne by Biogen. The Alzheimer’s app does not have a similar pharmaceutical champion, mainly because there’s no successful drug on the market for that disease right now.
Dr. Rao expects that a drug will be developed and in use within the next five years. And research already has shown that lifestyle interventions such as exercise can be effective with Alzheimer’s.
“What we want to do is use the data from our app to see whether this is a valid and appropriate way of identifying the preclinical stage in patients. If it turns out that we’re very successful at identifying the people who are at risk of developing Alzheimer’s down the road, those are the people we counsel about increasing their physical activity and place them on a drug designed to alter the disease course.
“Our eventual goal,” he says, “is to make Cleveland Clinic a model for other medical centers in screening for preclinical Alzheimer’s disease.”
How You Can Help
The philanthropic support of individuals like you goes a long way in saving and improving the lives of patients the world over. To help people at risk for Alzheimer’s, contact Kristie Burke at 216.445.9412 or make a contribution online.
Power of Love Gala® Set for April 28

Join us for the 22nd annual Power of Love® gala on Saturday, April 28, at the MGM Grand Garden Arena in Las Vegas. The magical evening will feature an exclusive menu from iconic chefs Wolfgang Puck and Jean-Georges Vongerichten, and spectacular entertainment by superstar Michael Bublé.
Presented by Keep Memory Alive, the gala supports Cleveland Clinic Lou Ruvo Center for Brain Health, which is dedicated to helping patients and families affected by Alzheimer’s, Huntington’s and Parkinson’s diseases, as well as multiple system atrophy and multiple sclerosis. For more than two decades, Power of Love galas have raised millions to provide support for the center’s exceptional patient care, robust research projects and diverse education programs. The Power of Love gala underscores the critical role of generous donors, all of whom share the mission of eradicating these devastating brain illnesses.
The gala also is a spectacularly fun evening. Over the past 21 years, the Power of Love has become one of Las Vegas’ signature celebrity events. Legendary A-listers including Tony Bennett, Andrea Bocelli, Jon Bon Jovi, Bono, Gloria Estefan, Jennifer Hudson, Celine Dion, LL Cool J, Queen Latifah, Barry Manilow and many others have entertained guests at the annual benefit.
This year’s one-of-a-kind philanthropic evening features luxury silent and live auctions items, craft cocktails and Dom Pérignon Champagne. World-class wines and spirits selected by master sommeliers will accompany each chef’s tantalizing cuisine; then partygoers will be enchanted by the beguiling vocals of Grammy Award-winner Michael Bublé.
Celebrate the power of love at this extraordinary event to raise funds for researching, treating and – one day – curing cognitive disorders. Visit Keep Memory Alive for more information and to purchase tickets.
Need more reasons to attend the Power of Love gala? Watch our video.

