Glioblastoma (GBM) is a grade IV brain tumor. It starts in a type of glial cell called astrocytes. These are in your brain and spinal cord. Glioblastoma cancer cells grow and multiply quickly. The cancer invades and destroys healthy surrounding tissue. There isn’t a cure, but treatment may improve your quality of life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
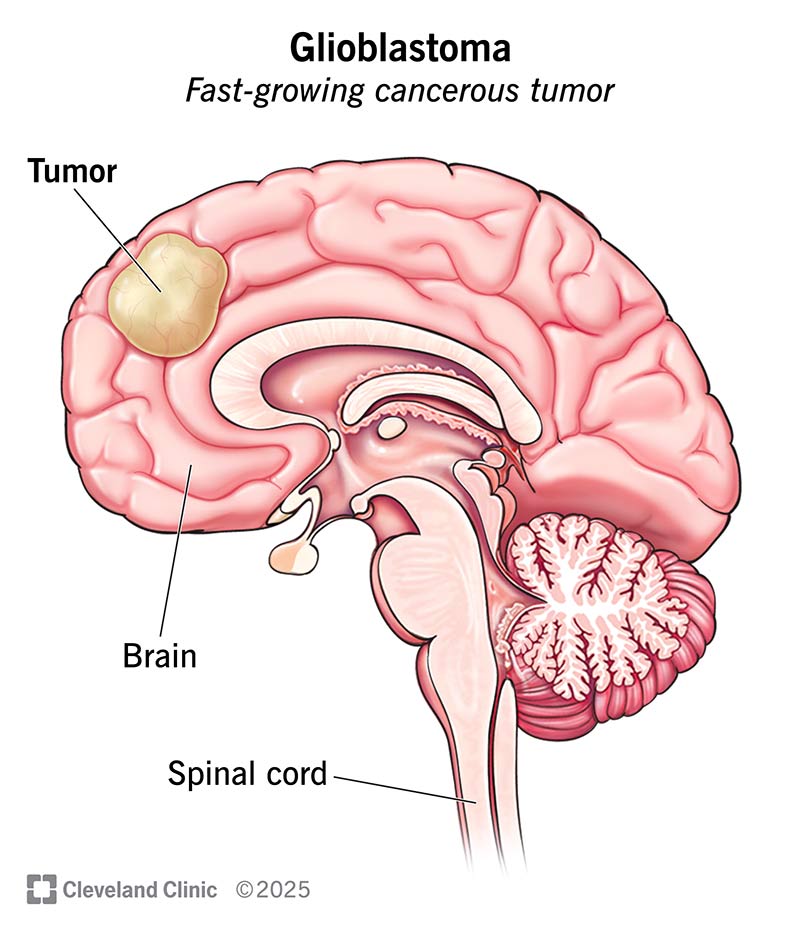
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/glioblastoma)
Glioblastoma (GBM) is the most common type of malignant (cancerous) brain tumor in adults. It starts in a type of glial cell in your brain and spinal cord called astrocytes. Cancer cells rapidly grow and multiply. They can spread into other areas of your brain and spinal cord. Rarely, cancer spreads beyond these areas.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Glial cells, including astrocytes, are vital to help nerve cells function. GBMs are the fastest-growing astrocytoma (a tumor that forms in astrocytes).
Glioblastoma, formerly known as glioblastoma multiforme, is a devastating type of cancer that can result in death in fewer than six months without treatment. More than 13,000 Americans are diagnosed with GBM every year.
If you notice any symptoms like vision changes, memory problems, headaches or seizures, visit a healthcare provider as soon as possible.
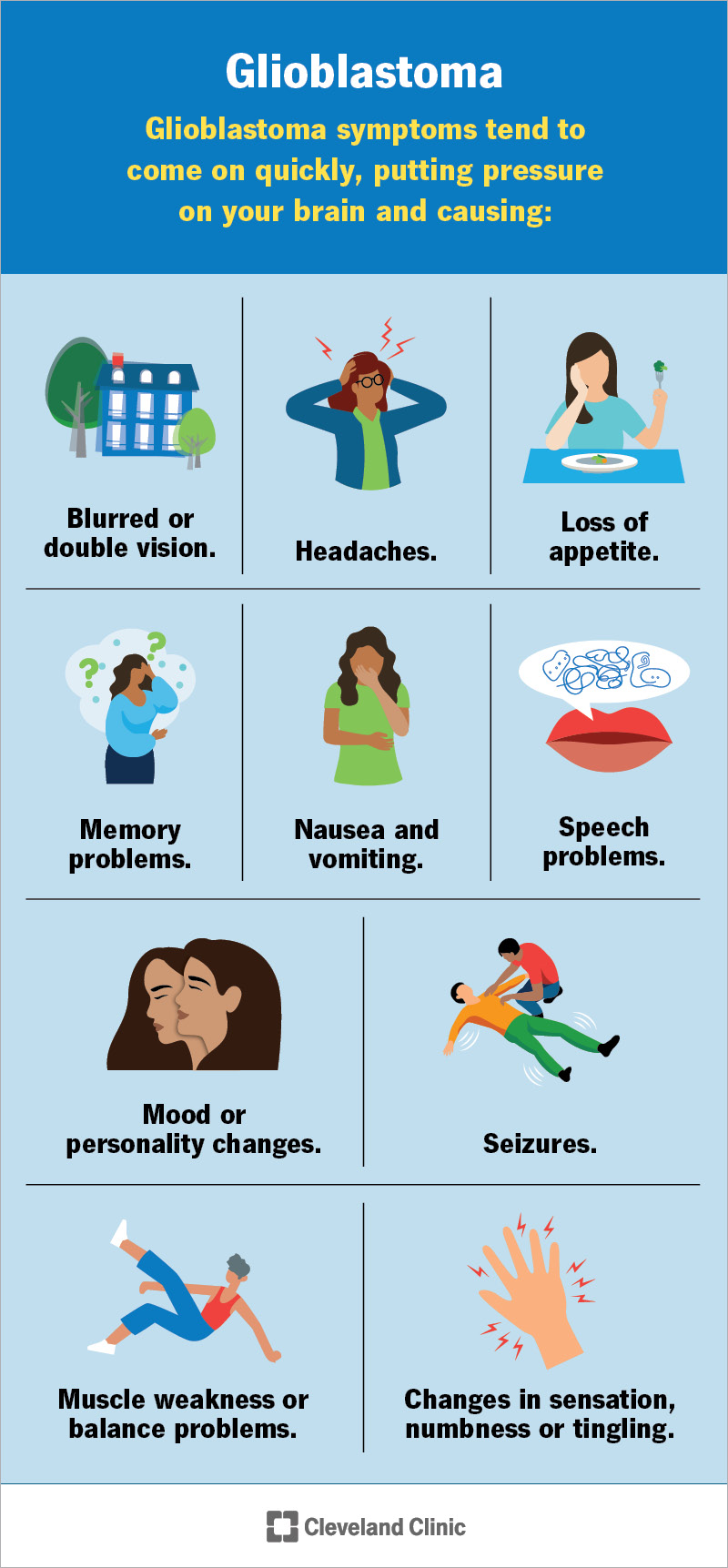
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17032-glioblastoma)
Glioblastoma symptoms may include:
Glioblastoma symptoms tend to come on quickly. The growing tumor puts pressure on your brain and can destroy healthy brain tissue.
Researchers don’t know the exact cause. Like other gliomas (tumors that form in your brain and spinal cord), researchers suggest that changes in your DNA lead to the development of glioblastoma brain tumors. Your genes contain DNA. They give instructions to your cells about how to grow and multiply. Mutations, or changes, to the DNA in your genes can cause cells to multiply out of control.
Advertisement
It’s possible to inherit genetic variations from your biological parents. But inherited GBMs are rare. Most commonly, these mutations happen randomly during your lifetime.
Glioblastoma most often affects people ages 45 to 70. The average age at diagnosis is 64.
These factors may increase your risk:
Glioblastoma and its treatments may affect brain function. You could experience mood changes and memory problems. Most people with GBM eventually have to stop working and driving. You may need full-time care. These changes could lead to anxiety disorders or depression.
A healthcare provider will evaluate your symptoms and perform a neurological exam. If they suspect you may have a brain tumor, you may have these tests:
Healthcare providers use a grading system from I (1) to IV (4) to indicate brain tumor behavior. Grade I brain tumors grow slowly and are the least aggressive. Grade IV tumors grow rapidly and are more aggressive. Glioblastoma tumors are grade IV.
Glioblastoma can be either primary or secondary:
Treatment may include tumor removal surgery (craniotomy), radiation and chemotherapy. If surgery isn’t a safe option, your care team may suggest radiation and chemotherapy to try to manage the tumor.
Glioblastoma treatment options include:
Advertisement
There isn’t a cure for glioblastoma.
You should call your healthcare provider if you experience:
Glioblastoma may result in early death shortly after a diagnosis without treatment. But treatments are available. They may help you ease symptoms and stay comfortable or prolong your life.
Clinical trials are underway to find new treatments. And therapies that target specific cancer cell genes show promise. Researchers are also looking at ways to deliver chemotherapy directly to the brain tumor. Your provider will let you know if a clinical trial is right for you.
Most people live an average of 12 to 18 months after diagnosis. The five-year survival rate for glioblastoma is only about 5%. That means about 5% of people with GBM are still alive five years after their diagnosis.
Genetic mutations that cause glioblastoma aren’t preventable. But early detection and treatment may slow the progression of a tumor.
If brain tumors run in your biological family, you may want to consider genetic testing. Talk to a healthcare provider or a genetic counselor about the risks and benefits of genetic testing.
Advertisement
Finding out you have glioblastoma (GBM) can be difficult. The tumor grows quickly and treatment is challenging. Researchers continue to look for new ways to treat GBM. For now, treatments can minimize symptoms and improve your quality of life. Your provider can guide you through the next steps and help you find the care and support you need.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A brain tumor diagnosis can change your life. At Cleveland Clinic, we know what it takes to treat glioma and glioblastoma and give you the support you need.
