Overview
Thank you for your interest in Cleveland Clinic’s General Surgery residency program. The training offered here provides an unmatched exposure to the entire spectrum of surgical diseases and procedures with abundant opportunities for research and professional development in a supportive environment. Trainees in our program are in the operating room from the beginning of intern year and finish with around 1000 cases. As a high volume international referral center, our residents operate on and care for some of the most challenging and complex patients. However, they also perform a substantial number of operations commonly seen by General Surgeons in community practice. The result is a robust toolbox of skills that prepares our graduates to take on any surgical problem.
Residents have the option to pursue 1-3 years of supplemental professional development time after the 2nd year of clinical training. This is an optional, flexible experience designed to meet the individual goals of the trainee. The Cleveland Clinic Lerner Research Institute has nearly 200 basic science laboratories with whom our residents can train. An accelerated program is available for physicians who wish to obtain a PhD in Molecular Medicine making it possible to complete during these years. A large number of ongoing clinical trials are also available for those interested in clinical research. Mentoring in outcomes, quality and education research is also offered. The available experience outside the clinical training years augments the multitude of opportunities for scholarship that can be pursued during clinical training. Department funding is available.
One of the most important elements of our program is the collegiality and camaraderie between the residents and faculty. Our structured advising program is supplemented by access to mentors who guide trainees towards their chosen fields. While most of our graduates pursue fellowship training after residency, around 15% go directly into academic or community practice.
On this website you will find more details of our program. If you believe our program fits your personal and professional goals, we invite you to apply for one of our categorical positions through ERAS. If you have further questions, though, please feel free to contact us. We believe it will become clear why Cleveland Clinic’s General Surgery residency program is one of the best.
Sincerely,
Ajita Prabhu, MD, FACS
Program Director, General Surgery Residency
Residency program leadership
R. Matthew Walsh, MD, FACS
Chair, Department of General Surgery
Sofya Asfaw, MD, FACS
Associate Program Director for Wellness and Mentorship
Chelsea (Xiaoxi) Feng, MD
Associate Program Director for Simulation

Daniel Joyce, MBBCh
Associate Program Director for Preliminary Residents
Robert Naples, DO
Associate Program Director for Scholarly Activity
Joseph Trunzo, MD, FACS
Associate Program Director for Didactic Curricula
Site Director, Fairview Hospital, General Surgery Residency

Rickesha Wilson, MD
Site Director, Hillcrest Hospital, General Surgery Residency
Judith French, PhD
Surgical Educator
Clinical Training & Conferences
Our residency program is unique because of its variety, case volume and variety of teaching settings. We are proud to have faculty and residents from a variety of backgrounds and experiences. Resident education and research are at the forefront of our department. Our residents rotate in a variety of clinical settings, including a leading quaternary teaching hospital, two regional Level II trauma centers, a Level I trauma and burn center county hospital as well as ambulatory surgery centers. Trainees care for a large volume of patients with extremely complicated and straightforward surgical diseases. All residents are guaranteed to be exposed to a large number of cases across all aspects of general surgery.
Experience
Our training philosophy is to involve the entire team, especially residents, in patient care at all times – pre-operative decision making in the clinic or in consultation, in the operating room, and during post-operative care. Experience is gained by operating on skill-appropriate cases at our high volume quaternary care hospital, regional hospitals, and ambulatory surgery centers. Leadership is developed by conferring a high level of responsibility early in the training program with progressive autonomy and responsibility. The most senior resident on a service is charged with assigning operative cases to residents and fellows, ensuring an optimal experience that is tailored to each resident.
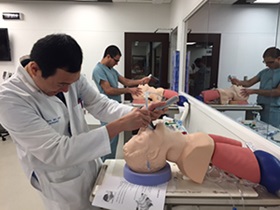
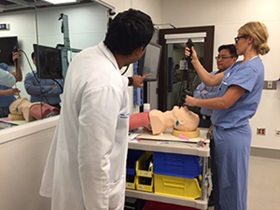
Surgery simulation
The Cleveland Clinic Simulation and Advanced Skills Center is an American College of Surgeons Accredited Education Institute equipped with laparoscopy, flexible endoscopy, robotic surgery, and endovascular surgery simulators. The center is a Fundamentals of Laparoscopic Surgery (FLS) and Fundamentals of Endoscopic Surgery (FES) training and testing site. Residents have 24-hour access to the sim-lab where they can practice skills. A robust skills curriculum using simulation is integrated into the teaching program with sessions occurring around once per month.
A DaVinci XI training robot is available for practice with 24/7 access to augment our robust simulation and on-console robotics training program.
Night float/call format
The main campus has a night float system, consisting of a team of PGY-1, PGY-2, and PGY-4 residents. This format allows all team members to operate in level-appropriate cases, provide longitudinal care of patients, and dedicate time to research projects, leadership positions, and knowledge development. When not on the night float rotation, junior residents typically take call two weekends per month and senior residents take call about once a month. We adhere to all ACGME work hour regulations, including the 80-hour work week and an average of one day off per week averaged over the month. Regional hospitals have a rotating call schedule with residents taking in house call around 1-2 times per week.
Morbidity and mortality conference
M&M conference is held weekly and is designed to foster inter-disciplinary learning and collegial discussions between trainees and faculty.
Grand rounds
Quarterly Grand Rounds by both local experts and internationally recognized Visiting Professors promote surgical learning for faculty and residents. In addition to lecture style seminars, residents have the unique opportunity to interact with these leaders over case presentations and informal lunch discussions. Residents also benefit by meeting with these surgeons in an informal setting to ask questions about research, career trajectory, and general life advice. Topics cover a broad range including modern advances, historical perspectives, world health, and the environmental impact of healthcare to name a few.
Cleveland Clinic conferences
Our residents may attend high-level, multidisciplinary conferences taught by our world-renowned faculty aimed at practicing digestive, vascular, oncologic and endocrine disease specialists. These combine clinical management updates by thought leaders, hands-on skills development, and quality and patient safety developments.
Who makes up the PGY-1 surgery class?
Our PGY-1 class is made up of 11 categorical and 13non-designated preliminary General Surgery residents. Additionally, designated interns from multiple specialties rotate on our general surgery services facilitating exposure to relevant general surgery cases for our subspecialty colleagues, and creating rapport between residents across departments. Interns from our Integrated Vascular, Cardiovascular, Thoracic, Plastics, Urology, Orthopedic, and Otolaryngology work closely with our general surgery residents.
PGY-1 Fundamentals of Surgery Seminar Series
Residents arrive as PGY-1’s with a range of knowledge and clinical experience. Orientation to the program includes a two week skills training course designed to help all new residents get accustomed to common technical skills, clinical scenarios and our electronic health record. During the first month of training, all new residents participate in a didactic and simulation curriculum to ease the transition to residency.
Weekly learning sessions
Protected educational conferences occur every Wednesday morning from 7-11 am. All residents are excused from their clinical responsibilities during this time. The format varies week-to-week, ranging from lecture based content from leading Cleveland Clinic faculty, research work-shops, simulation activities, and game-based ABSITE review. The curriculum for this conference follows a two-year revolving schedule based on the SCORE curriculum, and is supplemented by access to Scientific American’s Decker online question bank and content.
Service specific conferences
Each service holds its own conference (weekly) and journal clubs (monthly). Journal clubs are usually held at restaurants.
Advising and mentorship programs
Each trainee, upon entrance to our program, is assigned a faculty and resident advisor. The staff-member helps facilitate the trainee’s integration into Cleveland Clinic and assist them throughout their time here. Trainees meet with their faculty advisors at least twice a year to go over their milestones, evaluations, progress and accomplishments.
New trainees are also aligned with a senior resident to help them navigate issues with which residents would be more familiar than staff.
Our program believes that mentorship is an organic relationship that cannot be assigned. All of our faculty participate as mentors to our trainees. Throughout their time here, most residents identify several mentors in a variety of areas such as career, family, work-life integration, research and leadership.
Administrative experience
Residents have the opportunity to participate in administrative roles very early on their path through the program. Two administrative Chiefs Residents are selected by the residents and program administration to assist in the day-to-day oversight, including rotation schedules, call schedules, education improvements and new initiatives. In addition, residents have the opportunity to hold membership in the department’s education committee, residency recruitment committee, research committee, intern orientation and quality improvement committees, serve as the medical student liaison and help organize social events. Faculty also serve as champions to assist trainees in attaining membership and leadership roles in national organizations.
Opportunities for electives both inside and outside Cleveland Clinic
All PGY-3s, 4s and 5s have a designated block of elective time each year. This time may be used for additional exposure to one of the core rotations at the main campus or regional hospitals. Alternatively, this time may be used to pursue other interests including rotation at other institutions if desired.
Global health
Opportunities for international rotations are available to those who are interested with funding available. In the past, residents have rotated at St. Vincent’s Hospital in Dublin, Ireland where they learned how surgical training is provided in a nationally centralized system in addition to working on a busy trauma and oncology service. Residents have also rotated at the Rwanda Military Hospital in Kigali, Rwanda, learning about surgical care and training in an under-resourced setting.
Rotations & Teams
PGY-1 (4 weeks per rotation)
Acute Care
Acute Care Surgery Night Float
Colorectal
Bariatrics/Endoscopy
Endocrine
HPB/Oncology
Liver Transplant
MIS/hernia/General Surgery
Pediatric
Plastic Surgery
Thoracic
Vascular
Fairview Orange (Peds/Breast/MIS/HPB)
Fairview Colorectal
Fairview General Surgery/Trauma
Fairview ICU
Fairview Vascular Surgery
Hillcrest General Surgery
PGY-2 (4 weeks per rotation)
Acute Care Night Float
Bariatric
Breast
Intestinal Transplant
MIS/Hernia/General Surgery
Plastic
Fairview Peds/Breast/MIS/HP
Fairview ICU
Fairview General Surgery/Trauma
Fairview Vascular
Hillcrest General Surgery
Hillcrest HPB/Colorectal
MetroHealth Trauma / ICU
MetroHealth Burns / ICU
PGY-3 (5 weeks per rotation)
Acute Care
Breast*
Pediatric*
Liver Transplant*
Minimally Invasive/Bariatric Surgery/Surgical Endoscopy*
Fairview General Surgery/Trauma
Fairview Colorectal
Fairview Vascular
Hillcrest General Surgery
Elective
PGY-4 (5 weeks per rotation)
Acute Care Night Float*
Endocrine*
HPB/Surgical Oncology
MIS/Hernia/General Surgery*
Minimally Invasive/Bariatric Surgery/Surgical Endoscopy
Thoracic
Fairview Colorectal*
Fairview General Surgery/Trauma
Metro Health Trauma*
Elective
PGY-5 (5-12 weeks per rotation)
Acute Care*
Colorectal - Acting Fellow*
Fairview Peds/Breast/MIS/HPB*
Fairview Vascular*
Hillcrest General Surgery*
Hillcrest HPB/Colorectal*
HPB/Surgical Oncology*
MIS/Hernia/General Surgery*
Elective
*Chief
Surgical teams
Main Campus
| Rotation | Team |
|---|---|
|
HPB/Surgical Oncology |
PGY5, PGY4, PGY2, PGY1 |
|
Endocrine |
PGY4, PGY1 |
|
MIS/Hernia (Steiger) |
PGY4, PGY3, PGY1 |
|
MIS/Hernia (Grundfest) |
PGY5, PGY2, PGY1 |
|
MIS/Bariatrics/Surgical Endoscopy |
PGY4, PGY1 |
|
Bariatric |
PGY2 |
|
Acute Care Surgery-Days |
PGY5, PGY3, PGY12x |
|
Acute Care Surgery Nights |
PGY4, PGY2, PGY12x |
|
Pediatric Surgery |
PGY3, 2x-PGY1 |
|
Breast |
PGY3, PGY2 |
|
Liver Transplant |
PGY3, PGY1 |
|
Multivisceral Transplant |
PGY2 |
Regional hospital teams
| Rotation | Team |
|---|---|
|
Hillcrest General Surgery |
PGY5, PGY3, PGY1 |
|
Hillcrest HPB and Colorectal |
PGY5, PGY2, PGY1 |
|
Fairview Vascular |
PGY5, PGY3, PGY2, PGY1 |
|
Fairview Colorectal |
PGY4, PGY3, PGY2 |
|
Fairview General Surgery/Trauma |
PGY4, PGY3, PGY2, PGY1 (2x) |
| Fairview Peds/Breasts/MIS/HPB | PGY5, PGY2, PGY1 |
|
Fairview SICU |
PGY2 |
| MetroHealth Level 1 Trauma / ICU | PGY4, PGY2 |
| MetroHealth Burn / ICU | PGY2 |
Research
Resident research
A successful career in surgery, both in an academic and a community setting, requires an understanding of research and the ability to critically appraise medical literature. All residents in our program participate in a comprehensive academic curriculum with year-round lectures, individualized mentorship and extensive resources to encourage resident participation in research.
Those who are interested may arrange for additional years of professional development time during residency, typically after the second clinical year. Departmental and other funding sources are available. This time can be used to obtain an advanced degree, participate in basic science research, or become involved in one of many prospective clinical studies conducted at Cleveland Clinic.
We offer a 2-year Surgical Education Research Fellowship that is accredited by the American College of Surgeons. A Master of Health Professions Education is also possible through this position.
Residents routinely present their work at local, regional, national and international meetings. Release from clinical duties and travel support is provided.
Resident Research Day
Our annual resident research day showcases the impressive academic endeavors completed by General Surgery residents in both the clinical and basic sciences.
Research opportunities
Research is one of the main pillars of Cleveland Clinic, as is reflected by the vast resources offered by the institution to continuously innovate and improve patient care. Fueled by the unique case volume and complexity, the surgical divisions and departments are pioneers in clinical and basic science research with multiple ongoing prospective trials and large historical databases readily available. Unique opportunities exist across all surgical specialties for residents interested in academics to work within established groups and excel. In addition, those interested in laboratory research benefit from access to the more than 200 principal investigators at the Cleveland Clinic’s Lerner Research Institute.
Clinical research opportunities for general surgery residents
All clinical research groups continuously conducting research projects, and reaching out to any can be a great way for current residents to get involved in research during their clinical surgery time. Some also offer fully-funded research positions for 2 years that allow research fellows to take time off between clinical years 2 and 3 for an immersive experience in clinical research.
Additionally, some general surgery residents choose to pursue a PhD and engage in more translational/bench research in a lab with separate funding. Those opportunities are not included in this list.
If any current general surgery residents are interested in participating in research with the groups below, they should reach out directly to the Principal Investigator via email.
- Bariatric and Metabolic Surgery
- Breast Surgery
- Colorectal Surgery
- Endocrine Surgery
- Differences in Health Outcomes in General Surgery
- Hepatobiliary Surgery
- Hernia Surgery
- Liver Cancer
- Liver Transplant Surgery
- Pediatric Surgery
- Quality Improvement
- Surgical Education
- Minimally Invasive Surgery
PhD in molecular medicine
Residents have the option to attain a PhD in Molecular Medicine through the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University. Residents receive academic credit for their medical degree making it possible to complete the program during these years.
Current Residents in Professional Development
Justin Bauzon, MD
Justin is completing his research studies under the endocrine surgery department. His primary focus is on the genetic and biochemical basis of thyroid/parathyroid malignancy as well as clinical outcomes research. Current projects include an analysis of diagnostic molecular markers in thyroid cancer, role of hyperparathyroidism on orthopedic outcomes, relationship of parathyroidectomy with calcific coronary disease, and predictive neural network modeling for thyroid cancer. Justin is also interested in research quality and safety initiatives.
Mentors: Allan Siperstein, MD, Judy Jin, MD, Gustavo Romero-Velez, MD
Fadlullah Ba’th, MD, MA
Fadlullah is conducting outcomes research in the fields of bariatric, metabolic, and general surgery. His primary focus encompasses both prospective and retrospective studies investigating the impact of various factors, both modifiable and non-modifiable, on the overall outcomes of obese populations. As an URiM, he holds a specific interest in the interplay between modifiable risk factors and the mitigation of differences in bariatric outcomes.
Mentors: Ali Aminian, MD, Xiaoxi Feng, MD, Rickesha Wilson, MD, Ricard Corcelles Codina, MD
William Bennett, MD
Will is the first-year Hernia Surgery and Abdominal Core Health Research Fellow. His primary research interests regard randomized controlled trials and prospective trial design considerations for surgical outcomes research. Surgical topics of interest include clinical and radiographic correlates of abdominal wall tensiometry, parastomal hernia management, postoperative chronic pain in mesh-based repairs, and component separation techniques. He is currently coordinating randomized controlled trials evaluating absorbable synthetic mesh vs pledget repair for large hiatal hernias, inguinal mesh explantation vs observation for chronic groin pain, and a contemporary comparison of suture vs mesh repair of small incisional hernias. He also contributes to research aimed at reducing resource use and waste in surgical practices while maintaining high standards of patient care, and supports initiatives that promote health career exposure to middle school students in the Cleveland area.
Mentors: Michael Rosen, MD, Ajita Prabhu, MD, Clayton Petro, MD, Benjamin Miller, MD, David Krpata, MD, and Lucas Beffa, MD
Andrew Conner, MD, PhD
Andrew is a general thoracic surgery clinical research fellow. His research interests include benign foregut, esophageal cancer, and lung cancer surgery. Current projects include initiating a randomized clinical trial comparing outcomes of intrapyloric Botox injection to pyloromyotomy during esophagectomy. In addition to using outcomes data to answer questions related to the management of achalasia, Andrew is planning to build a outcomes-based database on lung cancer patients treated at the Cleveland Clinic to answer questions in an effort to guide optimal surgical management of lung cancer.
Elissa Dabaghi
Elissa is currently completing the James Church, MD-Sheetz Family Endowed Clinical Fellowship in Hereditary Colorectal Cancer Syndromes at Cleveland Clinic. Her clinical focus includes management of patients with FAP, Lynch Syndrome, and other hereditary colorectal cancer syndromes, and her research is primarily outcomes focused. Current projects include comparing quality of life, cancer worry, and regret of Lynch Syndrome patients after segmental versus extended colectomy, infertility outcomes of FAP patients that undergo colectomy, as well as outcomes and the natural history of rectal polyposis in FAP patients that undergo IRA versus IPAA.
Mentors: Joshua Sommovilla, MD, David Liska, MD
Divya Deverakonda
Divya is a research fellow in the Hepato-Pancreato-Biliary (HPB) Surgery, Liver Cancer, and Liver Transplant Surgery Research Groups. Her work is primarily outcomes-based and includes clinical trials as well as retrospective studies. Her current research focus includes surgical and endoscopic management of duodenal polyposis in patients with FAP, colonic fistula formation in patients with necrotizing pancreatitis, long term outcomes in the surveillance and management of pancreatic cystic neoplasms, and surgical outcomes following liver resection or liver transplantation for MASH cirrhosis and MASH-associated malignancies.
Mentors: R Matthew Walsh, MD; Robert Simon, MD; Robert Naples, DO; Toms Augustin, MD MPH; Samer Naffouje, MD; Daniel Joyce MBBCh; Andrea Schlegel, MD MBA; Federico Aucejo, MD
Amanda Graveson, MD
Amanda is completing her research studies at the University of California, San Francisco in the Pediatric Surgery Department. The lab focuses on developing innovative prenatal therapies to treat congenital disorders before birth, with a particular emphasis on in utero stem cell transplantation and gene therapy.
Mentor: Tippi MacKenzie, MD
Janell Holloway, MD
Janell is conducting basic science research under the Physicians Researchers Innovating in Science and Medicine (PRISM) program under Feng Lin, PhD. At the conclusion of this program, she will have a PhD in molecular medicine. She is currently studying the potential role of CDCP1 (a surface protein highly expressed in colon cancer) in regulating gut homeostasis.
Diana Jimenez, MD
Diana is a clinical research fellow with the department of colorectal surgery. Her types of research include Meta-analysis, clinical trials, and outcomes-focused research. Areas of interest include irritable bowel disease, and rectal cancer. She is currently working on defining textbook outcomes for surgeries in patients with IBD. Additionally, she is working on investigating cost and healthcare resource utilization as a consequence of venous thromboembolism complications postoperatively. Diana is also working on a clinical trial with a novel drug which aims to shorten the course of postoperative ileus.
Mentor: Stefan Holubar, MD
Sangeeta Satish, MD
Sangeeta is conducting research with the Liver Transplantation department. Her research interests include viability assessment, machine perfusion and HCC recurrence following liver transplant.
Mentor(s): Andrea Schlegel, MD (Liver Transplant)
Erika Schmidt, MD
Erika is conducting research regarding surgical outcomes in general surgery and abdominal wall reconstruction. Within the Center for Abdominal Core Health, she coordinates both retrospective and prospective data collection, including several randomized controlled trials. Her current areas of research include preoperative weight loss before abdominal wall reconstruction, long-term outcomes following minimally-invasive ventral hernia repair, postoperative opioid utilization, and outcomes following robotic versus open ventral hernia repair. She additionally is interested in surgical education at both the undergraduate and graduate level.
Mentors: Lucas Beffa, MD, David Krpata, MD, Benjamin Miller, MD, Clayton Petro, MD, Ajita Prabhu, MD
Noah Tocci, MD
Noah is conducting research regarding surgical outcomes in general surgery, abdominal wall reconstruction, and hepatopancreatobiliary. Within the Center for Abdominal Core Health, and HPB he coordinates both retrospective and prospective data collection, including several randomized controlled trials. His current areas of research include post operative management following inguinal hernia repair, utilization of wound matrices for necrotizing soft tissue infections, postoperative opioid utilization, outcomes and management for patients with complex necrotizing pancreatitis, pancreatic cysts and the utility of EUS in pancreatic masses. Additionally, he is interested in surgical education at both the undergraduate and graduate level.
Mentors: Clayton Petro, MD, R. Matthew Walsh, MD, David Krpata, MD, Benjamin Miller, Lucas Beffa, MD, Ajita Prabhu, MD, Robert Simon, MD, Robert Naples, MD, Daniel Joyce, MD, Toms Augustin, MD, Samer Naffouje MD
Ece Unal, MD
Ece is a clinical research fellow with the department of colorectal surgery. Her types of research include clinical trials, outcomes-focused research and qualitative research. Areas of interest include inflammatory bowel disease and surgical education in colorectal surgery. Current projects include rescue therapy for postoperative ileus after colorectal surgery, impact of GLP1 agonist therapy on functional outcomes after pelvic pouch creation and safety of perianal elective operative intervention in Crohn's disease.
Mentors: Stefan Holubar, MD MS; Arielle Kanters, MD
Pooja Varman, MD
Pooja is the current surgical education research fellow who is applying qualitative and quantitative research methods to study medical student transitions to surgical residency, teaching in the operating room, and simulation- and video-based education for minimally invasive surgery. She is involved in curriculum design for the general surgery program and surgery clerkship, creating content for the surgery podcast Behind the Knife, and obtaining a master’s in education. She has additional interests in socially responsible surgery, surgical palliative care, and breast surgery.
Mentors: Jeremy Lipman, MD, MHPE, Judith French, PhD, Anna Chichura, MD, Stephanie Valente, DO, and Zahraa AlHilli, MD, MBA
Melissa Wills, MD
Mélissa works in the minimally invasive, foregut surgery, and surgical endoscopy research lab. Her scholarly output encompasses a range of publications, including randomized controlled trials, retrospective analyses, and academic book chapters. Current projects comprise a comparison in outcomes of PEG and PEG-J tubes, an investigation in endoscopic management strategies of gastroparesis, a study of the effects of standardized limb length in roux-en-y gastric bypass, and a textbook chapter on esophageal emergencies. When she's not working in the lab, she can be found spending time outdoors, in the gym, or at Edgewater Beach with her friends.
Mentors: Matthew Kroh, MD; Salvador Navarrete, MD; Andrew Strong, MD; Jerry Dang, MD, PhD
Clinical Research Groups
Bariatric and Metabolic Surgery Research Group
Principal Investigator: Ali Aminian, MD
Co-Investigators: Rickesha Wilson, MD, Chelsea Feng, MD, Ricard Corcelles, MD, Matthew Kroh, MD, Kalman Bencsath, MD, Walter Cha, MD, Jesse Gutnick, MD, Toms Augustin, MD, MPH, Salvador Navarrete, MD, Andrew Strong, MD
Funded Opportunities: Potential opportunities may be available upon request
Research Focus:
- Effects of bariatric surgery on health consequences of obesity such as diabetes, cardiovascular disease, fatty liver disease, cancer, COVID-19, etc.
- Individualized approach in bariatric procedure selection.
- Role of changes in microbiome in health benefits of bariatric surgery.
- Bariatric surgery in patients with specific underlying medical conditions such as heart failure, pulmonary hypertension, cirrhosis, organ transplant candidates, etc.
- Differences in outcomes after bariatric surgery based on factors that influence health outcomes.
Recent/Noteworthy Publications:
- Aminian A, Al-Kurd A, Wilson R, Bena J, Fayazzadeh H, Singh T, Albaugh VL, Shariff FU, Rodriguez NA, Jin J, Brethauer SA, Dasarathy S, Alkhouri N, Schauer PR, McCullough AJ, Nissen SE. Association of Bariatric Surgery With Major Adverse Liver and Cardiovascular Outcomes in Patients With Biopsy-Proven Nonalcoholic Steatohepatitis. JAMA. 2021 Nov 23;326(20):2031-2042. doi: 10.1001/jama.2021.19569. PMID: 34762106; PMCID: PMC8587225.
- Aminian A, Wilson R, Al-Kurd A, Tu C, Milinovich A, Kroh M, Rosenthal RJ, Brethauer SA, Schauer PR, Kattan MW, Brown JC, Berger NA, Abraham J, Nissen SE. Association of Bariatric Surgery With Cancer Risk and Mortality in Adults With Obesity. JAMA. 2022 Jun 28;327(24):2423-2433. doi: 10.1001/jama.2022.9009. PMID: 35657620; PMCID: PMC9166218.
- Landreneau JP, Strong AT, Rodriguez JH, Aleassa EM, Aminian A, Brethauer S, Schauer PR, Kroh MD. Conversion of Sleeve Gastrectomy to Roux-en-Y Gastric Bypass. Obes Surg. 2018 Dec;28(12):3843-3850. doi: 10.1007/s11695-018-3435-1. PMID: 30094577.
Breast Surgery Research Group
Principal Investigator: Zahraa AlHilli, MD
Co-Investigators: Debra Pratt, MD, Stephanie Valente, DO, Erica Peters, MD, Julie Lang, MD
Funded Opportunities: Potential opportunities may be arranged upon request
Research Focus:
- Exploring healthcare delivery of breast cancer from initial entry point into system to flow between specialties (surgery, radiation oncology, medical oncology, etc) and ultimate treatment.
- Pain control after breast surgery and opioid-reducing options.
- Cost and value of breast oncological care from different perspectives (patient, healthcare system).
- Enhanced recovery after surgery (ERAS) pathway for post-breast surgery.
Recent/Noteworthy Publications:
- ElSherif A, Armanyous S, Gentle CK, Al-Hilli Z, Valente SA. Trends of Contralateral prophylactic mastectomy at the time of ipsilateral breast tumor recurrence. Am J Surg. 2022 Mar;223(3):533-537. doi: 10.1016/j.amjsurg.2021.12.009. Epub 2021 Dec 11. PMID: 34924172.
- Al-Hilli Z, Wilkerson A. Breast Surgery: Management of Postoperative Complications Following Operations for Breast Cancer. Surg Clin North Am. 2021 Oct;101(5):845-863. doi: 10.1016/j.suc.2021.06.014. Epub 2021 Aug 7. PMID: 34537147.
- ElSherif A, Shah C, Downs-Kelly E, Alhareb A, Valente SA, Tu C, Al-Hilli Z. Outcomes of ipsilateral breast tumor recurrence after breast conserving surgery: Repeat lumpectomy as an alternative to salvage mastectomy. Surgery. 2022 Mar;171(3):673-681. doi: 10.1016/j.surg.2021.10.069. Epub 2021 Dec 12. PMID: 34911644.
- ElSherif A, Armanyous S, Al-Hilli Z, Valente SA. Mastectomy options for the treatment of ipsilateral breast cancer recurrence after lumpectomy. Am J Surg. 2022 Mar;223(3):447-451. doi: 10.1016/j.amjsurg.2021.11.028. Epub 2021 Dec 15. PMID: 34955166.
Colorectal Surgery – Note Several Groups
Principal Investigator: The staff in the colorectal surgery department at main campus are actively engaged in research, and often collaborate with each other. Some of the staff and their specific interests are listed below. The department offers a wind range of research options to include outcomes, prospective trials and quality. Residents are supported to go to regional and national meetings to present their work. In addition, support for statistical analysis and educational conferences is standard with the group.
Co-Investigators: Scott Steele, MD, MBA, Tracy Hull, MD, Stefan Holubar, MD, David Liska, MD, Emre Gorgun, MD, Hermann Kessler, MD, Michael Valente, DO, Anuradha Bhama, MD, Jeremy Lipman, MD, Joshua Sommovilla, MD, Arielle Kanters, MD
Funded Opportunities: Funding for research positions is available for 1-2 years. The source of funding will vary based on the fellow and what projects they will undertake. In general, funding is available from DDSI, the Colorectal Surgery Department, or a specific PI related to a specific project.
Research Focus: The colorectal surgery department has several staff who are actively engaged in research in all aspects of colorectal surgery, including colorectal cancer, IBD, hereditary cancers, and endoscopic colorectal surgery techniques. There are a large number of internal or national/international database studies, clinical research trials, and basic science research in various areas of colorectal surgery. Specific interests of different PIs are listed below.
Principal Investigator: Scott Steele, MD, MBA
Specific Research Interests:
- Rectal cancer.
- Retrospective studies in all areas of colorectal surgery.
Recent/Noteworthy Publications:
- Short- and Long-term Outcomes of Ileal Pouch Anal Anastomosis Construction in Obese Patients With Ulcerative Colitis. Leeds IL, Holubar SD, Hull TL, Lipman JM, Lightner AL, Sklow B, Steele SR. Dis Colon Rectum. 2022 Aug 1;65(8):e782-e789.
- Advanced age alone should not preclude surveillance colonoscopy in the octogenarian and older population. Sapci I, Guyton K, Church J, Liska D, Gorgun E, Steele SR, Valente MA. Am J Surg. 2022 Mar;223(3):510-512. doi: 10.1016/j.amjsurg.2021.11.033. Epub 2021 Dec 2. PMID: 34916038
Principal Investigator: Tracy Hull, MD
Specific Research Interests:
- Ileal Pouch-Anal Anastomosis (IPAA) related research.
Recent/Noteworthy Publications:
- Pouch volvulus-why adhesions are not always the enemy. Dionigi B, Prien C, Lavryk O, Lightner AL, Holubar SD, Hull T. Colorectal Dis. 2022 May 18. doi: 10.1111/codi.16195. Online ahead of print. PMID: 35585780
- Turnbull-Cutait abdominoperineal pull-through operation: The Cleveland Clinic experience in the 21st century. Lavryk OA, Bandi B, Shawki SF, Floruta C, Xue J, Valente MA, Steele SR, Hull TL. Colorectal Dis. 2022 May 1. doi: 10.1111/codi.16163. Online ahead of print. PMID: 35490348
Principal Investigator: Stefan Holubar, MD
Specific Research Interests:
- Inflammatory bowel disease.
- NSQIP and other database-related research.
Recent/Noteworthy Publications:
- What About Patient Cost? Defining Copay and Out-of-Pocket Costs of Extended Venous Thromboembolism Chemoprophylaxis After Colorectal Surgery. Prien C, Ribakow D, Steele SR, Liska D, Kessler H, Hull TL, Holubar SD. J Gastrointest Surg. 2022 Jul 26. doi: 10.1007/s11605-022-05416-8. Online ahead of print. PMID: 35882761
- Use of Intraoperative Calibration Spheres for Endoluminal Stricture Assessment to Facilitate Heineke-Mikulicz Strictureplasty in Diffuse Stricturing Crohn's Jejunoileitis. Duraes LC, Lee CHA, Holubar SD. Dis Colon Rectum. 2022 Jul 1;65(7):e741-e742. doi: 10.1097/DCR.0000000000002360. Epub 2022 Mar 23. PMID: 35333805
Principal Investigator: David Liska, MD
Specific Research Interests:
- Hereditary cancer and polyposis syndromes.
- Early onset colorectal cancer.
- Differences in health outcomes.
Recent/Noteworthy Publications:
- Effect of Incisional Negative Pressure Wound Therapy on Surgical Site Infections in High-Risk Reoperative Colorectal Surgery: A Randomized Controlled Trial. Sapci I, Camargo M, Duraes L, Jia X, Hull TL, Ashburn J, Valente MA, Holubar SD, Delaney CP, Gorgun E, Steele SR, Liska D. Dis Colon Rectum. 2022 Apr 1. doi: 10.1097/DCR.0000000000002415. Online ahead of print. PMID: 35358097
- Enhanced Recovery Pathway Benefits Patients Undergoing Nonelective Colorectal Surgery. Liska D, Novello M, Cengiz BT, Holubar SD, Aiello A, Gorgun E, Steele SR, Delaney CP.
Ann Surg. 2021 Apr 1;273(4):772-777. doi: 10.1097/SLA.0000000000003438. PMID: 32697898
Principal Investigator: Emre Gorgun, MD
Specific Research Interests:
- Advanced endoscopic techniques in colorectal surgery, including endoscopic submucosal dissection (ESD).
- Colonoscopy and colorectal cancer screening.
Recent/Noteworthy Publications:
- Outcomes and Cost Analysis of Robotic Versus Laparoscopic Abdominoperineal Resection for Rectal Cancer: A Case-Matched Study. Gorgun IE, Cengiz TB, Ozgur I, Dionigi B, Kalady MF, Steele SR. Dis Colon Rectum. 2022 Feb 21. doi: 10.1097/DCR.0000000000002394. Online ahead of print. PMID: 35195554
- A technical note on the treatment of large perianal condylomata acuminata. Ozgur I, Kanters A, Isakov R, Gorgun E. Colorectal Dis. 2022 Aug 8. doi: 10.1111/codi.16295. Online ahead of print. PMID: 35938233
- Restorative proctocolectomy with ileal pouch-anal anastomosis in elderly patients - is advanced age a contraindication? Duraes LC, Liang J, Steele SR, Cengiz B, Delaney CP, Holubar SD, Gorgun E.
- ANZ J Surg. 2022 Apr 18. doi: 10.1111/ans.17728. Online ahead of print. PMID: 35434821
Endocrine Surgery Research Group
Principal Investigator: Eren Berber, MD (Can also reach out to other Co-investigators individually)
Co-Investigators:Allan Siperstein, MD, Joyce Shin, MD, Vikram Krishnamurthy, MD, Judy Jin, MD, Katherine Heiden, MD
Funded Opportunities: Potential opportunities may be arranged upon request
Research Focus:
- Fluorescence in endocrine surgical procedures.
- Adrenalectomy procedures comparing different techniques such as laparoscopic and robotic.
- Liver tumor ablation, laparoscopic liver resection.
- Clinical studies based on existing databases.
- Patient-reported outcomes in thyroid and parathyroid surgery.
- Creating video abstracts of specific surgical techniques.
Recent/Noteworthy Publications:
- Broome DT, Naples R, Bailey R, Tekin Z, Hamidi M, Bena JF, Morrison SL, Berber E, Siperstein AE, Scharpf J, Skugor M. Use of Preoperative Imaging in Primary Hyperparathyroidism. J Clin Endocrinol Metab. 2021 Jan 1;106(1):e328-e337. doi: 10.1210/clinem/dgaa779. PMID: 33119066.
- Zolin SJ, Crawford K, Rudin AV, Harsono H, Krishnamurthy VD, Jin J, Berber E, Siperstein A, Shin JJ. Selective parathyroid venous sampling in reoperative parathyroid surgery: A key localization tool when noninvasive tests are unrevealing. Surgery. 2021 Jan;169(1):126-132. doi: 10.1016/j.surg.2020.05.014. Epub 2020 Jul 8. PMID: 32651054.
- Zolin SJ, Crawford K, Rudin AV, Harsono H, Krishnamurthy VD, Jin J, Berber E, Siperstein A, Shin JJ. Selective parathyroid venous sampling in reoperative parathyroid surgery: A key localization tool when noninvasive tests are unrevealing. Surgery. 2021 Jan;169(1):126-132. doi: 10.1016/j.surg.2020.05.014. Epub 2020 Jul 8. PMID: 32651054.
- Isiktas G, Nazli Avci S, Ergun O, Krishnamurthy V, Jin J, Siperstein A, Berber E. Laparoscopic versus robotic adrenalectomy in pheochromocytoma patients. J Surg Oncol. 2022 Sep;126(3):460-464. doi: 10.1002/jso.26918. Epub 2022 May 14. PMID: 35567781.
Healthcare Disparities in General Surgery Research Group
Principal Investigator: Sofya Asfaw, MD
Co-Investigators: Rickesha Wilson, MD, David Liska, MD, Claire Konys, PA-C
Funded Opportunities: None currently, however, funded Quality Improvement Research Fellow works closely with this group
Research Focus:
- Identifying barriers to care in healthcare outcomes based on patient demographics and other social drivers of health.
- Evidence-based interventions to mitigate gaps in surgery access and quality.
- Topics span across general surgery – from trauma to breast surgery to colorectal surgery.
- Educating the healthcare community on causes of disparate care in general surgery.
- Advocacy for collection of SDOH factors for use in research.
Recent/Noteworthy Publications:
Multiple projects in various stages of development, including under review for publication.
Hepatobiliary Surgery Research Group
Principal Investigator: Matthew Walsh, MD
Co-Investigators: Robert Simon, MD, Toms Augustin, MD MPH, Daniel Joyce, MBBCh
Funded Opportunities: 1-2 fully-funded positions annually for a 2-year research fellowship
Research Focus:
- Clinical research.
- Pancreatic cancer, liquid biopsy.
- Pancreatic cystic lesions such as IPMN and serous cystadenoma.
- Pancreatic neuroendocrine tumors.
- Pancreatic surgery prehabilitation and outcomes.
Recent/Noteworthy Publications:
- Perlmutter BC, Ali J, Cengiz TB, Said SA, Tang A, Augustin T, Joyce D, Simon R, Walsh RM. Correlation between physical status measures and frailty score in patients undergoing pancreatic resection. Surgery. 2022 Mar 1;171(3):711-7. https://doi.org/10.1016/j.surg.2021.10.030
- Naples R, Walsh RM, Thomas JD, Perlmutter B, McMichael J, Augustin T, Simon R. Short-and long-term surgical outcomes of total pancreatectomy with islet autotransplantation: A comparative analysis of surgical technique and intraoperative heparin dosing to optimize outcomes. Pancreatology. 2021 Jan 1;21(1):291-8. https://doi.org/10.1016/j.pan.2020.11.013
- Perlmutter BC, Naples R, Hitawala A, McMichael J, Chadalavada P, Padbidri V, Haddad A, Simon R, Walsh RM, Augustin T. Factors that Minimize Curative Resection for Gallbladder Adenocarcinoma: an Analysis of Clinical Decision-Making and Survival. Journal of Gastrointestinal Surgery. 2021 Sep;25(9):2344-52. https://doi.org/10.1007/s11605-021-04942-1
Hernia Surgery Research Group
Principal Investigator: Michael Rosen, MD
Co-Investigators: Ajita Prabhu, MD, Clayton Petro, MD, Benjamin Miller, MD, David Krpata, MD, Lucas Beffa, MD, Adele Costanzo, RN
Funded Opportunities: 2-5 fully-funded positions annually for a 2-year research fellowship
Research Focus:
- Clinical research, trial design, multiple ongoing randomized control trials.
- Abdominal core health.
- Minimally invasive hernia repair.
- Abdominal wall biomechanics.
- Mesh and biomaterials.
- Benign foregut and anti-reflux surgery.
Recent/Noteworthy Publications:
- Rosen MJ, Krpata DM, Petro CC, Carbonell A, Warren J, Poulose BK, Costanzo A, Tu C, Blatnik J, Prabhu AS. Biologic vs synthetic mesh for single-stage repair of contaminated ventral hernias: a randomized clinical trial. JAMA surgery. 2022 Apr 1;157(4):293-301. doi:10.1001/jamasurg.2021.6902
- Petro CC, Zolin S, Krpata D, Alkhatib H, Tu C, Rosen MJ, Prabhu AS. Patient-reported outcomes of robotic vs laparoscopic ventral hernia repair with intraperitoneal mesh: the PROVE-IT randomized clinical trial. JAMA surgery. 2021 Jan 1;156(1):22-9. doi:10.1001/jamasurg.2020.4569
- Prabhu AS, Carbonell A, Hope W, Warren J, Higgins R, Jacob B, Blatnik J, Haskins I, Alkhatib H, Tastaldi L, Fafaj A. Robotic inguinal vs transabdominal laparoscopic inguinal hernia repair: the RIVAL randomized clinical trial. JAMA surgery. 2020 May 1;155(5):380-7. doi:10.1001/jamasurg.2020.0034
Liver Cancer Research Group
Principal Investigator: Federico Aucejo, MD
Co-Investigators: Koji Hashimoto, MD PhD, Bijan Eghtesad, MD, Masato Fujiki, MD, Choon Hyuck Kwon, MD, PhD, Charles Miller, MD, Rotating research fellows
Funded Opportunities: None present
Research Focus:
- Translational and clinical research.
- Liver malignancy digital histopathology: Predictive signatures via artificial intelligence.
- Role of liquid biopsy in liver malignancy.
- Salivary metabolomics as biomarkers of liver malignancy.
- Perioperative adjunct therapies for primary and secondary liver cancer.
- Role of liver transplantation in the management of primary and secondary liver malignancy
Recent/Noteworthy Publications:
- Sasaki K, Nair A, Moro A, Augustin T, Quintini C, Berber E, Aucejo FN, Kwon CH. A chronological review of 500 minimally invasive liver resections in a North American institution: overcoming stagnation and toward consolidation. Surgical Endoscopy. 2022 Mar 11:1-9. https://doi.org/10.1007/s00464-022-09182-1
- Barron JO, Orabi D, Moro A, Quintini C, Berber E, Aucejo FN, Sasaki K, Kwon CH. Validation of the IWATE criteria as a laparoscopic liver resection difficulty score in a single North American cohort. Surgical Endoscopy. 2022 May;36(5):3601-9. https://doi.org/10.1007/s00464-021-08561-4
- Hershberger CE, Rodarte AI, Siddiqi S, Moro A, Acevedo‐Moreno LA, Brown JM, Allende DS, Aucejo F, Rotroff DM. Salivary metabolites are promising non‐invasive biomarkers of hepatocellular carcinoma and chronic liver disease. Liver Cancer International. 2021 Aug;2(2):33-44. https://doi.org/10.1002/lci2.25
Liver Transplant Surgery Research Group
Principal Investigator: Koji Hashimoto, MD PhD
Co-Investigators: Federico Aucejo, MD, Bijan Eghtesad, MD, Masato Fujiki, MD, Choon Hyuck Kwon, MD, PhD, Charles Miller, MD, Rotating research fellows
Funded Opportunities: Potential opportunities can be arranged
Research Focus:
- Bariatric Surgery, with specific focus on revisional bariatric surgery
- GERD
- Motility disorders
- MALS
- Surgical innovation and technology
- Research fellow is a part of the DDSI Innovations and Technology program, including device development, tech-based endoscopy and surgery labs associated with the program, and the DDSI Innovation Council
Recent/Noteworthy Publications:
- Aminian A, Wilson R, Al-Kurd A, Tu C, Milinovich A, Kroh M, Rosenthal RJ, Brethauer SA, Schauer PR, Kattan MW, Brown JC, Berger NA, Abraham J, Nissen SE. Association of Bariatric Surgery With Cancer Risk and Mortality in Adults With Obesity. JAMA. 2022 Jun 28;327(24):2423-2433. doi: 10.1001/jama.2022.9009. PMID: 35657620
- Schwalbe K, Finelli C, Moon S, Niehaus H, Kondajji A, Tu C, Fathalizadeh A, Kroh M, Allemang M. Endoscopic findings do not predict per-oral pyloromyotomy (POP) response. Surg Endosc. 2022 May 24. doi: 10.1007/s00464-022-09321-8. PMID: 35608698.
- Qudah Y, Abdallah M, Barajas-Gamboa JS, Del Gobbo GD, Pablo Pantoja J, Corcelles R, Rodriguez J, Balci N, Kroh M. Personalized Health Care Technology in Managing Postoperative Gastrointestinal Surgery Complications: Proof of Concept Study. J Laparoendosc Adv Surg Tech A. 2022 Apr 28. doi: 10.1089/lap.2022.0114. PMID: 35483077.
- Majid SF, Husain FA, Choi Y, Gill S, Schirmer B, Kroh M, Kurian M. The SAGES MASTERS program presents the 10 seminal articles for Roux-en-Y gastric bypass. Surg Endosc. 2022 Jan;36(1):6-15. doi: 10.1007/s00464-021-08861-9. PMID: 34855007
Pediatric Surgery Research Group
Principal Investigator: Jason Robertson, MD
Co-Investigators: Darrell Cass, MD, Anthony DeRoss, MD, John DiFiore, MD, David Magnuson, MD
Funded Opportunities: Potential opportunities can be arranged upon request
Research Focus:
- Endothelial progenitor cell dysfunction relative to development of pulmonary hypoplasia and hypertension in congenital diaphragmatic hernia
- Pectus excavatum
- Bracing for pectus carinatum
- Pediatric VV ECMO cannula choice
- Appendectomy for RLQ pain
- Non-standard indications for cholecystitis
- Pediatric Surgery workforce issues
- Role for pediatric and adult combined colorectal surgery clinic
Recent/Noteworthy Publications:
- DiFiore JW, Robertson JO, Chhabada S, DeRoss AL, Hossain MS, Rincon-Cruz L, Sung W. Next day discharge after the Nuss procedure using intercostal nerve cryoablation, intercostal nerve blocks, and a perioperative ERAS pain protocol. Journal of Pediatric Surgery. 2022 Feb 1;57(2):213-8. PMID: 34823843. DOI: 10.1016/j.jpedsurg.2021.10.034
- Robertson JO, Criss CN, Hsieh LB, Matsuko N, Gish JS, Mon RA, Johnson KN, Hirschl RB, Mychaliska GB, Gadepalli SK. Comparison of early versus delayed strategies for repair of congenital diaphragmatic hernia on extracorporeal membrane oxygenation. J Pediatr Surg. 2018 Apr;53(4):629-634. doi: 10.1016/j.jpedsurg.2017.10.056. Epub 2017 Nov 22. PMID: 29173775
- Sajankila N, DeRoss A, Lipman JM. Approach to the Adult Colorectal Patient with a History of Pediatric Abdominal Surgery. Clin Colon Rectal Surg. 2022 Aug 12;35(3):177-186. doi: 10.1055/s-0042-1742412. PMID: 35966376; PMCID: PMC9374533.
Quality Improvement Research Group
Principal Investigator: Toms Augustin, MD MPH
Co-Investigators: Kelly Nimylowycz, Kelly Walker
Funded Opportunities: One fully-funded position for a 2-year research fellow (cycles every 2 years with only 1 fellow at any given time)
Research Focus:
- Sepsis care and prevention of sepsis-related mortality
- Optimal transfers of acute surgical patients between hospitals with different surgical capabilities
- Prevention of serious safety events
- Predicting and preventing hospital re-admission in general surgical patients
- Management and monitoring of data to assess the quality and safety of healthcare
- Harnessing the electronic health record to prevent specific patient-harm events
- Monitoring quality and patient safety using American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) data
Recent/Noteworthy Publications:
- Nimeri AA, Gamaleldin MM, McKenna KL, Turrin NP, Mustafa BO. Reduction of Venous Thromboembolism in Surgical Patients Using a Mandatory Risk-Scoring System: 5-Year Follow-Up of an American College of Surgeons National Surgical Quality Improvement Program. Clin Appl Thromb Hemost. 2017 May;23(4):392-396. doi: 10.1177/1076029615614396. Epub 2015 Nov 25. PMID: 26607437.
- Gentle CK, Alkhatib H, Valente SA, Tu C, Pratt DA. Stage IV Non-breast Cancer Patients and Screening Mammography: It is Time to Stop. Ann Surg Oncol. 2022 Jul 18. doi: 10.1245/s10434-022-12132-9. Epub ahead of print. PMID: 35849289.
Surgical Education Research Group
Principal Investigator: Jeremy Lipman, MD, MHPE
Co-Investigators: Judith French, PhD, Ajita Prabhu, MD
Funded Opportunities: One fully-funded position for a 2-year research fellowship (cycles every 2 years with only 1 fellow at any given time), as well as full funding for the pursuit of Masters of Education degree (typically MHPE or MEHP degree).
Research Focus:
- Operative teaching and assessment
- Operative autonomy
- Simulation teaching and assessment
- Curriculum design
- Residency recruitment
- Medical student education in surgery
- Professionalism in surgery
- Any aspect of surgical education
- Translational and clinical research
- Improving transplant outcomes
- Machine perfusion pump to improve ex-vivo viability of borderline donor livers
- Novel therapeutics for improvement of allograft function
- Immunotherapies in the prevention of transplantation rejection
- Impact of metabolomics on peri-transplant patient outcomes
- Model development with realistic perfusate for laparoscopic and robotic ex vivo hepatectomy and transplant training
- Minimally invasive liver surgery
Recent/Noteworthy Publications:
- Quintini C, Del Prete L, Simioni A, Del Angel L, Uso TD, D’Amico G, Hashimoto K, Aucejo F, Fujiki M, Eghtesad B, Sasaki K. Transplantation of declined livers after normothermic perfusion. Surgery. 2022 Mar 1;171(3):747-56. PMID: 35065791 DOI: 10.1016/j.surg.2021.10.05
- Matsushima H, Fujiki M, Sasaki K, Cywinski JB, D’Amico G, Uso TD, Aucejo F, Kwon CH, Eghtesad B, Miller C, Quintini C. Can pretransplant TIPS be harmful in liver transplantation? A propensity score matching analysis. Surgery. 2020 Jul 1;168(1):33-9. PMID: 32268937 DOI: 10.1016/j.surg.2020.02.01
Minimally Invasive Surgery Research Group
Principal Investigator: Matthew Kroh, MD
Co-Investigators:Salvador Navarrete, MD, Jeffrey Ponsky, MD, Matthew Allemang, MD, Andrew Strong, MD, John Rodriguez, MD (Cleveland Clinic Abu Dhabi)
Funded Opportunities: Funding is available and provided either by the Department of General Surgery or the DDSI Innovations Program, depending on areas of interest of the research fellow
Research Focus:
- Foregut surgery
- Surgical endoscopy, including POEM, POP, and enteral access
- Currently in enrollment phase of randomized placebo-intervention trial for POP under a NIH RO1 Grant
Recent/Noteworthy Publications:
- Han AY, Naples R, French JC, Dragomirescu C, Tu C, Lipman JM. Operative teaching takes "GUTS": Impact of Educational Time Out on trainee's cognitive load. Am J Surg. 2022 Apr 4:S0002-9610(22)00215-X. doi: 10.1016/j.amjsurg.2022.03.037. PMID: 35414429.
- Naples R, French JC, Han AY, Lipman JM, Awad MM. The Impact of Simulation Training on Operative Performance in General Surgery: Lessons Learned from a Prospective Randomized Trial. J Surg Res. 2022 Feb;270:513-521. doi: 10.1016/j.jss.2021.10.003. PMID: 34801802.
- Han AY, Obiri-Yeboah D, French JC, Lipman JM. The Virtual Recruitment Onion: Peeling Back the Layers of the Interview Season During the COVID-era. J Surg Educ. 2022 Jan-Feb;79(1):77-85. doi: 10.1016/j.jsurg.2021.08.003. PMID: 34446384.
- Naples R, French JC, Thomas JD, Lipman JM. A New Era in Graduate Medical Education: A Novel Role for Surgical Subinternships in the Interview Selection Process. Ann Surg. 2021 Jan 1;273(1):e16-e18. doi: 10.1097/SLA.0000000000004042. PMID: 32773620.
Pipeline Program
The Middle School Healthcare Careers Program (MSHCP) was created in 2022 by our general surgery residents to expand the healthcare pipeline. The mission is to inspire middle school students in our Cleveland community to pursue careers in healthcare by hosting multiple events each academic year. To date, MSHCP has reached several hundreds of students, offering them hands-on experiences and all areas of medicine.
Program Highlights
Each event features specialty stations with engaging, hands-on activities that provide students with a glimpse into various healthcare careers. For example,
- Surgery: Laparoscopic skills, suturing, knot tying
- Critical Care: Central lines, arterial lines, ultrasound
- Dental: Cavity filling, dental hygiene
- Nutrition: Calorie counting, nutritional counseling
- Physical Therapy: Strengthening exercises
- Pharmacy: Compounding, pill counting
- Podiatry: Saw bones demonstrations
- Nursing: Vitals, IV placement, blood draws
- Operating Room Prep: Donning and doffing, scrubbing, table prep
- Obstetrics/Gynecology: C-section simulations, infant delivery techniques
Our Partners
We collaborate with local area schools and programs that serve socioeconomically under-resourced youth, including
- Boys Hope Girls Hope
- Breakthrough Schools
- Almira Public Schools
Our professional partners include
- Cleveland Clinic’s Center for Youth and College Education (CYCE)
- Cleveland Surgical Society
- Cuyahoga Community College (Tri-C)
- Baldwin Wallace University
Funding & Support
Our program is made possible through generous grant funding from
- Catalyst Grant
- Martha Holden Jennings Foundation
We are thankful for the abundance of support and hopeful that programs like this might help to shape the future of healthcare.
Current Residents
PGY-1 Categorical

Victoria Ajayi, MD
- Medical School: Tufts University School of Medicine
- Career Interest: Cardiothoracic surgery, trauma and critical care, hernia surgery, surgical education, global surgery, pediatric surgery

Yara Alfawares, MD
- Medical School: University of Cincinnati College of Medicine
- Career Interest: Cardiothoracic, transplant/HPB, vascular

Faris Almadi, MD
- Medical School: Royal College of Surgeons in Ireland - Medical University of Bahrain
- Career Interest: Cardiothoracic surgery, vascular surgery

Grace Patrice Anyetei-Anum, MD
- Medical School: Mayo Medical School
- Career Interest: Cardiothoracic surgery

Lovette Azap, MD
- Medical School: Ohio State University College of Medicine
- Career Interest: Minimally invasive surgery, cardiothoracic surgery

Mohanad Baroudi, MD
- Medical School: Alfaisal University College of Medicine
- Career Interest: Undecided

Pooja Dave, MD
- Medical School: University Of Miami LM Miller School Of Medicine
- Career Interest: Minimally invasive surgery, HPB surgery

Karl Hage, MD
- Medical School: Universite Saint-Joseph Faculte de Medecine
- Career Interest: Colon and rectal surgery, MIS, endocrine surgery

Vidur Kailash, DO
- Medical School: Touro Un College Of Osteopathic Medicine, Vallejo
- Career Interest: Cardiothoracic, vascular surgery, and colorectal surgery

Heekyung Jenny Kim, MD
- Medical School: Case Western Reserve University
- Career Interest: Abdominal wall reconstruction, MIS, global surgery

Renita Wilson, MD
- Medical School: Mayo Medical School
- Career Interest: Surgical education
PGY-1 Preliminary

Abdalla Abuzubida, MD
- Medical School: Alfaisal University College of Medicine
- Career Interest: General surgery, colorectal surgery, HPB surgery

Maria Alqamish, MD
- Medical School: Royal College of Surgeons in Ireland School of Medicine
- Career Interest: Surgical oncology, colorectal and breast surgery

Ayman Alrazim, MD
- Medical School: American University of Beirut Faculty of Medicine
- Career Interest: Colorectal surgery or surgical oncology

Jasmine Chaij, MD
- Medical School: University of Texas Medical Branch At Galveston/li>
- Career Interest: Plastic and reconstructive surgery and abdominal wall reconstruction

Fachreza Aryo Damara, MD
- Medical School: Universitas Padjadjaran Fakultas Kedokteran
- Career Interest: Vascular Surgery, cardiothoracic surgery

Addison Gepfert, DO
- Medical School: Marian University College of Osteopathic Medicine
- Career Interest: Orthopaedic surgery, hand surgery

Bikona Ghosh, MD
- Medical School: Dhaka Medical College and Hospital
- Career Interest: Breast surgery, plastic surgery, surgical oncology

Abdullah Khan, MD
- Medical School: Shifa College of Medicine
- Career Interest: Vascular Surgery, cardiothoracic surgery

Muhammad Taimour Khan, MD
- Medical School: Lahore Medical and Dental College
- Career Interest: Trauma surgery, critical care

Sophia Pressman, DO
- Medical School: Des Moines Un, Col Of Osteopathic Med & Surgery
- Career Interest: Reconstructive surgery and critical care

Richard Ramsingh, MD
- Medical School: University of the West Indies Faculty of Medicine
- Career Interest: Cardiothoracic surgery, imaging-guided innovation

Gabriela Restrepo Rodas, MD
- Medical School: Universidad Internacional del Ecuador Facultad de Ciencias Medicas y de la Salud
- Career Interest: Minimally invasive general surgery, abdominal wall reconstruction, global surgery
PGY-2

Riley Bohan, MD
- Medical School: University of Florida College of Medicine.
- Career Interest: Surgical Oncology, Critical Care.
 .
.
Anagha Deshpande, MD
- Medical School: Mayo Clinic Alix School of Medicine, Arizona.
- Career Interest: Surgical Oncology, Breast, Endocrine.
Nadia Khan, MD
- Medical School: University of Washington School of Medicine.
- Career Interest: Trauma & Critical Care.
Karen Kong, MD
- Medical School: Rutgers NJMS.
- Career Interest: Colorectal, Breast.

Natalia Ochman, MD
- Medical School: University of Maryland Medical School.
- Career Interest: Trauma Surgery, Critical Care.

Hafsa Omer Sulaiman, MBBS
- Medical School: St George's University of London.
- Career Interest: Plastic surgery, transplant.

Vishal Rajesh, MD
- Medical School: Long School of Medicine at UT Health San Antonio.
- Career Interest: Liver transplant, HPB, Colorectal.

Rachel Schneider, MD
- Medical school: UMass Chan School of Medicine.
- Career Interest: Trauma surgery, General Surgery, Acute Care Surgery.

Henry Stitzel, MD
- Medical School: Case Western Reserve University School of Medicine.
- Career Interest: Undecided.

Riley Wilkinson, MD, MPH
- Medical School: University of Louisville.
- Career Interest: Undecided.
PGY-3

Abby Gross, MD
- Medical School: Case Western Reserve University School of Medicine.
- Career Interest: Critical Care, Pediatric Surgery, Colorectal Surgery.

Jared Hendren, MD
- Medical School: Southern Illinois University School of Medicine.
- Career Interest: Colorectal surgery.

Anibal La Riva Rincon, MD
- Medical School: Universidad Central de Venezuela Escuela de Medicina José María Vargas.
- Career Interest: Cardiothoracic Surgery, Trauma & Critical Care, Surgical Education.

Michael Littau, MD
- Medical School: Loyola University of Chicago, Stritch School of Medicine.
- Career Interest: Trauma, Critical Care.

April Martinez, MD
- Medical School: University of Texas Medical Branch, Galveston TX
- Career Interest: Colorectal surgery.

Fathi Moustafa, MD
- Medical School: Royal College of Surgeons – Bahrain
- Career Interests: Acute care surgery, critical care, and abdominal wall reconstruction

Ion Profirii, MD
- Medical School: Charles University, Czech Republic.
- Career interest: HPB, Transplant, Surgical Oncology.

Daphne Remulla, MD
- Medical School: Keck School of Medicine of USC.
- Career Interest: Surgical Education, Undecided.
Sarah Wang, MD, MPH
- Medical School: Virginia Commonwealth University.
- Career Interest: Surgical Oncology, Endocrine, MIS.

Chase Wehrle, MD
- Medical School: Medical College of Georgia.
- Career Interest: HPB Surgery, Surgical Oncology.

Kimberly Woo, MD
- Medical School: Case Western Reserve University School of Medicine.
- Career Interest: Surgical Oncology.
PGY-4

Juan Aulestia Herrera, MD
- Medical School: Universidad Central del Ecuador.
- Career Interest: Minimally Invasive and Robotic General Surgery, Minimally invasive HPB surgery.

Nicole Brooks, MD
- Medical School: Case Western Reserve University School of Medicine.
- Career Interest: Colorectal Surgery, Surgical Education, Global Surgery.

Jenny Chang, MD
- Medical school: Loma Linda University School of Medicine.
- Career Interest: Surgical oncology, Breast surgery, Surgical outcomes and public health.

Ryan Ellis, MD
- Medical School: McGovern Medical School.
- Career Interest: Undecided.

Yasser Fouda, MD
- Medical School: Faculty of Medicine, Mansoura University, Egypt.
- Career Interest: Liver, Pancreas, Kidney and Multivisceral Transplant, Gut Rehabilitation and HPB surgery.

Oscar Hernandez Dominguez, MD
- Medical School: University of California, Irvine School of Medicine.
- Career/Research Interest: Colorectal Surgery.

Benjamin Kramer, DO, MS
- Medical School: New York Institute of Technology College of Medicine.
- Career Interest: Cardiothoracic Surgery, Surgical Education.

Sara Maskal, MD
- Medical School: Case Western Reserve University School of Medicine.
- Career/Research Interest: Minimally Invasive Surgery, Abdominal Wall Reconstruction.

Megan Obi, MD
- Medical School: Case Western Reserve School of Medicine.
- Career Interest: Colorectal Surgery, Surgical Education, Global Surgery.
Research Interest and Institution: Colorectal Cancer, Benign Abdominal Disease, Inflammatory Bowel Disease - Cleveland Clinic.

Sadia Tasnim, MD
- Medical School: University of Texas Medical Branch.
- Career/Research Interests: thoracic, genetics, barriers to care, surgical education. Sadia is currently in clinical research studying both benign and malignant non-cardiac thoracic diseases.
PGY-5

Jordan Apfeld, MD
- Medical School: Stanford University School of Medicine.
- Career Interest: Thoracic Surgery.
- Research Interest: Surgical Outcomes Research Fellow, specializing in large database analysis.

Doua Elamin, MD
- Medical School: University of Medical Sciences and Technology, Khartoum (Sudan).
- Career Interest: MIS, Colorectal.

Corey Gentle, MD
- Medical School: UT Southwest Medical School.
- Career Interest: Endocrine Surgery, Breast Surgery, Pediatric Surgery, Global Health.

Mir Shanaz Hossain, MD
- Medical School: University of Pittsburgh School of Medicine.

Pavel Lenkov, MD
- Medical School: University of Oklahoma.
- Career Interest: General Surgery, Thoracic Surgery.

Gilman Plitt, MD
- Medical School: Creighton University School of Medicine.
- Career Interests: Endocrine Surgery, Surgical Oncology, Cancer Genetics.

Lorena Rincon-Cruz, MD
- Medical school: University of Colorado School of Medicine.
- Career Interest: Pediatric Surgery.

Nitin Sajankila, MD
- Medical School: Case Western Reserve University School of Medicine.
- Career Interest: Pediatric Surgery and Surgeon Scientist.

Brian Tang, MD
- Medical School: McGovern Medical School at UTHealth.

Noah Weingarten, MD, MA
- Medical School: Northwestern University.
- Career Interest: Pediatric and Cardiothoracic Surgery; Device Innovation and Global Surgery

Avia Wilkerson, MD
- Medical School: Case Western Reserve University School of Medicine.
- Career Interest: Surgical oncology, immunotherapies for solid cancers
Research

Fadlullah Ba’th, MD
- Medical School: University of Minnesota Medical School.
- Career Interests: Pediatric Surgery, Colorectal Surgery, MIS.
Justin Bauzon, MD
- Medical School: Kirk Kerkorian School of Medicine at UNLV.
- Career Interest: Colorectal, MIS, or Pediatric Surgery.

William Bennett, MD
- Medical School: University of North Carolina.
- Career Interests: Critical Care, MIS, Surgical Education.

Andrew Conner, MD
- Medical School: Frank H. Netter MD School of Medicine at Quinnipiac University.
- Career Interest: Thoracic surgery, HPB surgery.

Elissa Dabaghi, MD
- Medical School: University of Texas Medical Branch.
- Career Interest: Colorectal surgery.

Divya Deverakonda, MD
- Medical School: Case Western Reserve University School of Medicine.
- Career Interest: General Surgery, Critical Care, HP.

Amanda Graveson, MD
- Medical School: Oregon Health and Science University.
- Career Interest: General Surgery, Critical Care.

Jannell Holloway, MD
- Medical School: University of California, Los Angeles.
- Career Interest: Trauma, Colorectal, MIS.

Diana Jimenez, MD
- Medical School: Sidney Kimmel Medical College at Thomas Jefferson University.
- Career Interest: General Surgery, Colon and Rectal Surgery.

Sangeeta Satish, MD
- Medical School: Saint Louis University School of Medicine.
- Career Interest: Abdominal transplant surgery.

Erika Schmidt, MD
- Medical School: Saint Louis University School of Medicine, St. Louis, MO.
- Career Interests: Colorectal Surgery, Surgical Education.

Noah Tocci, MD
- Medical School: Geisel School of Medicine at Dartmouth.
- Career Interest: Undecided.

Ece Unal, MD
- Medical School: Sidney Kimmel Medical College at Jefferson, Philadelphia, PA.
- Career Interest: Surgical Education, undecided.

Pooja Varman, MD
- Medical School: Creighton University School of Medicine.
- Career Interest: Pediatric Surgery, Colorectal Surgery, Surgical Palliative Care, Surgical Education.

Melissa Wills, MD
- Medical School: Wayne State University School of Medicine.
- Career Interest: Surgical Education, Critical Care, and undecided!
Alumni
2025 |
|
|---|---|
| Raha Almarzooqi, MD | Colorectal Surgery Fellowship, Vanderbilt |
| Amy Han, MD | Endocrine Surgery Fellowship, Cleveland Clinic |
| Matthew Johnson, MD | Cardiac Surgery Fellowship, Washington University |
| George Kereselidze, MD | General Surgery Staff, Cleveland Clinic |
| Katie Montelione, MD | General Surgery, Private Practice |
| Moustafa Moussally, MD | Colorectal Surgery Fellowship, Cleveland Clinic |
| Andres Narvaez, MD | Colorectal Surgery Fellowship, Cleveland Clinic |
| Caleb Seavey, MD, PhD | Surgical Oncology Fellowship, Roswell Park |
| Shahed Tish, MD | MIS & Abdominal Wall Reconstruction Fellowship, Mayo Clinic |
| Emily Verbus, MD | Surgical Oncology Fellowship, University of Toronto |
2024 |
|
|---|---|
| Reece DeHann, MD | Colorectal Surgery Fellowship, Cleveland Clinic |
| Maysoon Gamaleldin, MD | Colorectal Surgery Fellowship, Cleveland Clinic |
| Alexis Harvey, MD | General Surgery, Trinity Health - North Dakota |
| Vyacheslav Lenkov, MD | Cardiothoracic Fellowship, Univ. of Wisconsin - Madison |
| Mujtaba Mubashir, MD | Cardiothoracic Fellowship, Beth Israel |
| Danny Orabi, MD | Liver Transplant Fellowship, Univ. of California - San Francisco |
| Camila Ortega Estrella, MD | Breast Surgery Fellowship, Cleveland Clinic Akron |
| Breanna Perlmutter, MD | Hepatopancreatobiliary Fellowship, Cleveland Clinic |
| Jesse Rappaport, MD | Minimally Invasive Surgery Fellowship, Allegheny Health |
2023 |
|
|---|---|
| Alicia Adams, MD | Colorectal Surgery Fellowship, University Hospitals |
| Tim Beck, MD | Endocrine Surgery Fellowship, Cleveland Clinic |
| Aldo Fafaj, MD | Abdominal Wall Reconstruction Fellowship, Cleveland Clinic |
| Alexandra Ferre, MD | Surgical Critical Care/Trauma/ACS Fellowship, Denver Health |
| Alexander Gibbons, MD | Fetal Surgery, Cincinnati Children’s Hospital |
| Paul Karam, MD | Bariatrics Fellowship, St. Luke’s Hospital, Allentown |
| Michael Klingler, MD | Colorectal Surgery Fellowship, Cleveland Clinic |
| Robert Naples, DO | Hepatopancreatobiliary Surgery Fellowship, Cleveland Clinic |
| Thomas Shin, MD | MIS/Bariatrics Fellowship, Brigham and Women’s Hospital |
| Sam Zolin, MD | Abdominal Wall Reconstruction Fellowship, Penn State Hershey |
2022 |
|
|---|---|
| Kevin Brown, MD | Bariatric & Minimally Invasive Surgery – Yale |
| Sarah Choi, MD, MS | Colorectal Surgery – University of Southern California |
| Bess Connors, MD | Breast Surgical Oncology – University of Michigan |
| Amanjit Gill, MD | Surgical Oncology – Allegheny General Hospital |
| Nadeem Haddad, MD | Burn & Reconstructive – Johns Hopkins University |
| Joshua Landreneau, MD | Minimally Invasive Surgery – Massachusetts General |
| Shashank Sharma, MD | Vascular Surgery – Houston Methodist |
| Kathryn Stackhouse, MD | Hepatopancreatobiliary Surgery – Cleveland Clinic |
| Andrew Tang, MD | Cardiothoracic Surgery – Cleveland Clinic |
| Yaning Zhang, MD | Hepatopancreatobiliary Surgery – Ascension Providence Hospital |
2021 |
||
|---|---|---|
| Dominykas Burneikis | Colorectal Surgery Fellowship | The Ohio State University |
| Talia Burneikis | Endocrine Surgery Fellowship | Cleveland Clinic |
| Mohammed Elshamy | Endocrine Surgery Fellowship | Cleveland Clinic |
| Monica Isabella | Surgical Critical Care Fellowship | Michigan State University |
| Sami Judeeba | Colorectal Surgery Fellowship | Cleveland Clinic |
| Olga Lavryk | Colorectal Surgery | Cleveland Clinic |
| Salvador Navarrete | MIS/Bariatric Surgery Staff | Cleveland Clinic |
| Justin Philip | MIS/Bariatric Surgery Fellowship | Dartmouth-Hitchcock Medical Center |
| Andrew Strong | MIS/Bariatric Surgery Fellowship | Duke University |
| Valery Vilchez | Colorectal Surgery Fellowship | UC-Irvine Medical Center |
2020 |
||
|---|---|---|
| Paul Adenuga | Plastic Surgery Fellowship | NYU Langone |
| Matthew Burstein | Minimally Invasive Surgery Fellowship | SUNY Buffalo |
| Maryna Chumakova-Orin | Minimally Invasive Surgery Fellowship | Duke University |
| Jennifer Colvin | Minimally Invasive Surgery Fellowship | Ohio State University |
| Jennifer Colvin | Minimally Invasive Surgery Fellowship | Ohio State University |
| Xiaoxi (Chelsea) Feng | Minimally Invasive Surgery Fellowship | Cedars-Sinai Medical Center |
| Ian Glenn | Thoracic Surgery Fellowship | Cleveland Clinic |
| Julia Muntean | Critical Care Fellowship | Cleveland Clinic |
| Lisa Park | Colorectal Surgery Fellowship | Cedars-Sinai Medical Center |
| Kaitlin Ritter | Trauma and Critical Care Fellowship | University of Colorado |
2019 |
|
|---|---|
| Nicholas Bruns | Pediatric Surgery Fellowship - Children’s Mercy Hospital |
| Jessica Ardila Gatas | Minimally Invasive and Bariatric Surgery Fellowship - Stony Brook University |
| Colin Gause | Pediatric Surgery Fellowship - Oregon Health and Science University |
| Charlotte Horne | Abdominal Wall Reconstruction and MIS Fellowship - Cleveland Clinic |
| George Karagkounis | Surgical Oncology Fellowship - Memorial Sloan Kettering Cancer Center |
| Marijan Koprivanac | Cardiothoracic Surgery Fellowship - University of Pennsylvania |
| Maitham Moslim | Surgical Oncology Fellowship - Fox Chase Cancer Center |
| Ahmed Nassar | Abdominal Transplant Fellowship - Emory University |
| Antonios Sideris | Thoracic Surgery Fellowship - Memorial Sloan Kettering Cancer Center |
| Vorranadha Vacharathit | Minimally Invasive and Bariatric Surgery Fellowship - Geisinger Medical Center |
2018 |
|
|---|---|
| Mohammad Abbass | Colorectal Surgery Fellowship - Cleveland Clinic Foundation |
| Amelia Dorsey | Minimally Invasive and Bariatric Surgery Fellowship - Stanford University |
| Emil Fernando | Breast Surgical Oncology Fellowship- Northwestern University |
| Ramona Ilie | Minimally Invasive Surgery Fellowship - Emory University |
| Daniel Joyce | Surgical Oncology Fellowship - Roswell Park Comprehensive Cancer Center |
| Hari Keshava | Thoracic Surgery Fellowship - Memorial Sloan Kettering Cancer Center |
| Yitian Liu | Breast Surgical Oncology Fellowship - Vanderbilt University Medical Center |
| S. Julie-Ann Lloyd | Minimally Invasive and Metabolic Surgery Fellowship - University of Pittsburgh |
| Hideo Takahashi | Surgical Oncology Fellowship - Roswell Park Comprehensive Cancer Center |
| JingLiang Yan | Minimally Invasive Surgery Fellowship - Vanderbilt University Medical Center |
2017 |
|
|---|---|
| Anas Abdelazim | Vascular Surgery Fellowship - University Hospitals Case Medical Center |
| Djurabek Babadjanov | Vascular Surgery Fellowship - Eastern Virginia Medical Center |
| Julietta Chang | Minimally Invasive Surgery Fellowship - Massachusetts General Hospital |
| Matthew Davis | Minimally Invasive Surgery Fellowship - Duke University |
| Kathryn Fong | Vascular Surgery Fellowship - University of Pittsburgh Medical Center |
| Adam Mace | Thoracic Surgery Fellowship - Cleveland Clinic |
| Trang Nguyen | Surgical Oncology Fellowship - John Wayne Cancer Institute |
| June Peng | Surgical Oncology Fellowship - Roswell Park Cancer Institute |
| Jacob Petrosky | Minimally Invasive Surgery Fellowship - Geisinger Health System |
| David Reznick | Endocrine Surgery Fellowship - Cleveland Clinic |
2016 |
|
|---|---|
| Avery Capone | Plastic and Reconstructive Surgery – Harvard Plastic Surgery |
| Matthew Dong | Minimally Invasive Surgery – Mount Sinai Medical Center, New York |
| Priya Jadeja | Breast Surgery – Columbia University Medical Center |
| Kelsey Larson | Breast Surgical Oncology - Cleveland Clinic |
| Michael Liu | Colorectal Surgery – Cleveland Clinic |
| Jay Mittal | Surgical Critical Care – Cleveland Clinic |
| Jeffrey Mino | Colorectal Surgery – Cleveland Clinic |
| Rosebel Monteiro | Endocrine Surgery – Cleveland Clinic |
| Naftali Presser | Abdominal Organ Transplant – University of California, Los Angeles |
| Jeh Yung | Private Practice – Redlands, CA |
2015 |
|
|---|---|
| Naveen Balasundaram | Vascular Surgery – Cleveland Clinic |
| Osama Essa | General Surgery Staff – Private Practice |
| Alfredo Daniel Guerron | Minimally Invasive Surgery – Duke University |
| Jesse Gutnik | Endocrine Surgery – Cleveland Clinic (2015-2016) Minimally Invasive Surgery - Duke University (2016-2017) |
| Billy Lan | Colorectal Surgery – Cleveland Clinic |
| Jose Lozada | Trauma and Critical Care – Jackson Health System University of Miami |
| Neal Moores | Plastic Surgery – University of Utah |
| Mihir Shah | Minimally Invasive Surgery – Emory University |
| Sherief Shawki | Colorectal Surgery – Cleveland Clinic |
| Subash Reddy | Minimally Invasive Surgery – University of California, San Francisco Fresno |
2014 |
|
|---|---|
| Gavin Falk | Pediatric Surgery – Miami Children's Health System |
| Ronald Charles | Colorectal Surgery – Cleveland Clinic |
| Shohrat Annaberdyev | Colorectal Surgery – Florida Hospital |
| Samir Shah | Vascular Surgery – Brigham and Women's Hospital |
| Sofya Asfaw | Trauma and Critical Care – University of Pennsylvania |
| Robert Cornateanu | Trauma and Critical Care – Johns Hopkins School of Medicine |
| Joshua Nash | Trauma and Critical Care – Cook County Health and Hospital System |
| Amy Hiuser | Plastic Surgery – SUMMA Health System |
| Samilia Obeng-Gyasi | Master in Public Health – Harvard T.H. Chan School of Public Health (2014-2015) | Breast Surgery – Duke University (2015-2016) |
| Nishant Raj | General Surgery Staff – Private Practice |
2013 |
|
|---|---|
| John Rodriguez | Flexible Surgical Endoscopy – Cleveland Clinic |
| Neil Kundu | Plastic Surgery – Cleveland Clinic |
| Omer Nasir | Colorectal Surgery – University of Medicine and Dentistry New Jersey |
| Hue Thai | Vascular Surgery – University of Medicine and Dentistry New Jersey |
| Jean Pierre Martucci Melo | Minimally Invasive Surgery – University of Illinois Chicago |
| Isaac Motamarry | Minimally Invasive Surgery – University of Florida |
| Viet Phuong | Minimally Invasive Surgery – Carolinas Healthcare Sysem |
| Christian Cruz | General Surgery Staff – Private Practice |
| Samuel Ibrahim | General Surgery Staff – Cleveland Clinic |
2012 |
|
|---|---|
| Vikram Attaluri | Colorectal Surgery – Cleveland Clinic |
| Jessica Titus | Vascular Surgery – Cleveland Clinic |
| Louisa Chiu | Surgical Oncology – City of Hope Cancer Center |
| Sam Bae | Bariatric and Laparoscopic Surgery – University of Southern California |
| Kevin Shah | Hepato-Pancreato-Biliary Surgery – Duke University |
| Nicole Sydow | Cardiothoracic Surgery – University of Arizona |
| Amit Sharma | Colorectal Surgery – University of Medicine and Dentistry, New Jersey |
| Jose Roberto Ramirez | Plastic Surgery – Vanderbilt Center of Plastic Surgery |
| Angel Farinas | General Surgery Staff – Private Practice |
2011 |
|
|---|---|
| Kalman Bencsath | Bariatric & Laparoscopic Surgery – Cleveland Clinic |
| Nakul Vakil | Cardiothoracic Surgery – Cleveland Clinic |
| Michael Tsinberg | Endocrine Surgery – University of California, San Francisco |
| George Cristescu | General Surgery Staff – Private Practice |
| Richy Lee | Pediatric Surgery – University of Calgary |
| Aaron Moore | Surgical Critical Care – University of Pittsburgh |
| John Bach | Surgical Critical Care – Ohio State University |
| Kevin El-Hayek | Surgical Endoscopy & Laparoscopy – Cleveland Clinic |
| Alexander Chang | Vascular Surgery – University Hospitals Case Medical Center |
2010 |
|
|---|---|
| Suzanne Brooks | Breast Surgery – Massachusetts General Hospital |
| William Abouhassan | Craniofacial Surgery & Plastic Surgery – Cleveland Clinic & University of Cincinnati |
| Christian Massier | General Surgery Staff – Cleveland Clinic |
| Justin Burdick | General Surgery Staff – United States Navy |
| Sheetal Nijhawan | Laparoscopy & Bariatric Surgery – University of California, San Diego |
| David Lee | Laparoscopy & Bariatric Surgery – Cleveland Clinic |
| George Rofaiel | Multi-Organ Transplant Surgery – University of Washington |
| Angelina Postoev | Surgical Critical Care – Ohio State University |
| Max Liebl | Vascular Surgery – Southern Illinois University |
2009 |
|
|---|---|
| Amara Malik | Breast Surgery – University of California, San Francisco |
| Werner Andrade Ortiz | Bariatric & Laparoscopic Surgery – University of South Florida |
| Travis Mason | General Surgery Staff – United States Army |
| Kara Schultz | General Surgery Staff – United States Air Force |
| Mohammed Alghoul | Plastic Surgery – Cleveland Clinic |
2008 |
|
|---|---|
| Michael Johnson | Hepato-Pancreato-Biliary Surgery – Cleveland Clinic |
| Jason Klovning | Multi-Organ Transplant Surgery – Emory University |
| Poornima Rao | Surgical Oncology – Fox Chase Cancer Center |
| Sherif Abdel Misih | Surgical Oncology – Ohio State University |
2007 |
|
|---|---|
| Kevin Rothchild | Bariatric & Laparoscopic Surgery – University of Colorado |
| Lewis Diulus | General Surgery Staff – United States Navy |
| Matthew Kroh | Surgical Endoscopy & Laparoscopy – Cleveland Clinic |
| Ravi Rajani | Vascular Surgery & Surgical Critical Care – Cleveland Clinic & Emory University |
2006 |
|
|---|---|
| Ikemma Okereke | Cardiothoracic Surgery – Beth Israel Deaconess Medical Center |
| Carolyn Garner | Endocrine Surgery – Cleveland Clinic |
| Rich Mackey | Hepato-Pancreato-Biliary Surgery – Cleveland Clinic |
| Peter Kreymerman | Plastic Surgery – Cleveland Clinic |
Staff Surgeons
Abdominal Wall Reconstruction and General Surgery
Breast Surgery
Main Campus
Hillcrest Hospital
Fairview Hospital
Colorectal Surgery
Main Campus
- Anuradha Bhama, MD
- Leonardo Duraes, MD, PhD
- I. Emre Gorgun, MD, MBA
- Stefan Holubar, MD
- Arielle Kanters, MD, MS
- Hermann Kessler, MD, PhD
- Olga Lavryk, MD, PhD
- David Liska, MD
- Jeremy Lipman, MD
- Johnathan Mitchem, MD
- Joshua Sommovilla, MD
- Anna Spivak, DO
- Scott Steele, MD, MBA
- Michael A. Valente, DO
Fairview Hospital
Hillcrest Hospital
Endocrine Surgery
- Allan Siperstein, MD, Chair, Department of Endocrine Surgery
- Eren Berber, MD
- Judy Jin, MD
- Vikram Krishnamurthy, MD
- Joyce Shin, MD
- Katherine Heiden, MD
Hepato-Pancreato-Biliary Surgery and Surgical Oncology
Main Campus
- R. Matthew Walsh, MD, Chair, Department of General Surgery
- Daniel Joyce, MBBCh
- Robert Naples, DO
- Robert Simon, MD
Fairview Hospital
Hillcrest Hospital
Liver and Multivisceral Transplant Surgery
- Masato Fujiki, MD, Director, Intestinal Transplant Program
- Koji Hashimoto, MD, PhD, Director, Liver Transplant Program
- Kareem Abu-Elmagd, MD, PhD
- Federico Aucejo, MD
- Mazhar Khalil, MD
- Jaekeun Kim, MD
- Choon Hyuck David Kwon, MD, PhD
- Charles Miller, MD
- Mohammed Osman, MD
- Alejandro Pita, MD
- Andrea Schlegel, MD
Metabolic and Minimally Invasive Surgery
Main Campus
Fairview Hospital
Hillcrest Hospital
Minimally Invasive and General Surgery
Main Campus
Fairview Hospital
- Diya Alaedeen, MD, Division Chief, General Surgery
- Toms Augustin, MD
- Kevin Baier, MD
- Cathleen Khandelwal, MD
- David Rosen, MD
- Andrew Smith, MD
Hillcrest Hospital
Surgical Critical Care
- Sofya Asfaw, MD
- Megan Beems, MD
- Tony Capizzani, MD
- Brett Elo, MD
- James Harrington, MD
- Jia Liu, MD
- John Medrick, DO
Surgical Endoscopy
Main Campus
Fairview Hospital
- Diya Alaedeen, MD, Division Chief, General Surgery
Pediatric Surgery
- Darrell Cass, MD, Director, Fetal Surgery
- Miguel Guelfand, MD, Director, Pediatric General Surgery
- Anthony DeRoss, MD
- John DiFiore, MD
- David Magnuson, MD
- Jason Robertson, MD
Thoracic Surgery
Main Campus
- Sudish Murthy, MD, PhD, Section Head, General Thoracic Surgery
- Siva Raja, MD, PhD, Associate Program Director, Thoracic Fellowship
- Daniel Raymond, MD
- Monisha Sudarshan, MD
Vascular Surgery
Main Campus
- Sean Lyden, MD, Chair, Department of Vascular Surgery
- Francis Caputo, MD, Program Director
- Jon Quatromoni, MD, Associate Program Director, Vascular Surgery Integrated
- Ravi Ambani, MD
- Courtney Hanak, MD
- Ali Khalifeh, MD
- Lee Kirksey, MD
Fairview Hospital
Hillcrest Hospital
Locations
Physicians at all locations are part of the Cleveland Clinic General Surgery, Vascular Surgery, or Colorectal Surgery Departments except for the MetroHealth Medical Center where the Level I trauma rotations are done.
Cleveland Clinic Main Campus
- Founded in 1921 by George Crile Sr., a general and endocrine surgeon; Frank Bunts, a neurosurgeon; William Lower, an urologist; and John Phillips, an internist.
- 44 buildings, over 85 operating rooms, more than 1,400 beds.
- Quaternary care center with an international referral base.
- Over 200,000 surgery cases each year.
- Program site director: Ajita Prabhu, MD.
Fairview Hospital
- Fairview Hospital is a busy community hospital and Level 2 Trauma Center on Cleveland’s west side. General Surgery Residents operate on all General, Colorectal, Breast, Endovascular, and Vascular Surgery cases and run the SICU and Trauma team.
- 488 beds.
- $83 million dollar expansion of emergency department and ICU in 2013.
- Site director: Joseph Trunzo, MD.
Hillcrest Hospital
- Hillcrest Hospital is a busy community hospital and Level 2 Trauma Center on Cleveland’s east side.
- 496 beds.
- $163 million dollar expansion and renovation in 2010.
- Site director: Kalman Bencsath, MD.
Lutheran Hospital
- Founded 1896; Joined CCHS 1997
- Beds: 203 licensed; 196 immediate availability
- Centers of Excellence: Spine, Orthopaedics, Behavioral Health, Wound Healing Center, Center for Spine Health
- Branded CC Services: Spine Health, Spine Research Lab, Behavioral Health (Alcohol and Drug Recovery Center, Adult Program and Mood Disorders Program)
- Renovations: Emergency Department, Operating Room and Cafeteria renovations
- Awards: Pathway to Excellence® Designation, ranked No. 34 in the nation for Patient Engagement by Becker’s Hospital Review, ranked No. 3 in the nation for Patient Safety by Consumer Reports, Press Ganey Commitment to Excellence Award
- The patient population is at a lower level of medical acuity than those often encountered at Main campus.
Metro Health Medical Center
- MetroHealth Medical Center is an academic health system, the regional Level 1 Trauma and Burn Center, and the regional safety net hospital on Cleveland’s south side.
- MetroHealth Medical Center’s staff surgeons are all professors at Case Western Reserve University Medical School.
- The Trauma Service has two teams, one run by a Cleveland Clinic General Surgery PGY-4 resident and the other run by a University Hospitals Case Medical Center General Surgery PGY-4 resident. The Trauma ICU is run by one PGY-2 resident from the Cleveland Clinic and one PGY-2 from University Hospitals Case Medical Center.
Beachwood, Strongsville, Twinsburg Family Health and Surgery Centers
- Beachwood, Strongsville, Twinsburg Family Health and Surgery Centers are ambulatory surgery centers staffed by Cleveland Clinic main campus, Hillcrest and Fairview surgeons. Residents perform endoscopy and operate on General and Breast Surgery cases in a fast track surgery environment.
Applications & FAQs
Categorical Program
The General Surgery residency program at Cleveland Clinic is approved for 11 categorical residents per year for five clinical years. A varying number of our categorical residents take advantage of optional research and professional development years, typically after PGY-2.
We seek trainees interested in a program with high clinical volume, scientifically-advanced care and robust opportunities for innovation. Our graduates become leaders as clinicians, researchers and educators. We recruit those whose backgrounds will further enhance the incredible culture of collaboration and camaraderie that exists in our program.
How to apply
Application deadline is Oct 3, 2025.
NRMP program code Categorical General Surgery 1968440C0
Applications are only accepted through ERAS. Our application requirements are the same as the standard ERAS application.
- Three letters of recommendation.
- Must not have failed any portion of the USMLE and/or COMLEX exam.
- Must report USMLE Step 2 or COMLEX 2 score.
- Institutionally, Cleveland Clinic has minimum requirements for all residents.
- Our program sponsors J1 visas for international medical graduates.
Preliminary program
The General Surgery residency at Cleveland Clinic is approved for 13 undesignated preliminary PGY 1 residents per year.
We seek trainees from around the world looking to gain additional experience prior to transitioning to a categorical residency. We also welcome those who have matched into an advanced training program and are looking for a robust General Surgery experience before beginning their specialty training.
Residents in the Preliminary program are fully integrated with residents in the Categorical program. They complete the same rotations, participate in all learning and social activities and function in the same role as Categorical residents.
A designated Associate Program Director for Preliminary Residents works to assure the best possible chance of attaining a Categorical position. However, all Categorical positions in our program are filled through the Match with no reserved spots for our Preliminary residents.
How to apply
Application deadline is Oct 3, 2025.
NRMP program code: Non-Designated Preliminary Surgery 1968440P0
Applications are only accepted through ERAS. Our application requirements are the same as the standard ERAS application.
- Three letters of recommendation.
- Must not have failed any portion of the USMLE and/or COMLEX exams.
- Must report USMLE Step 2 or COMLEX 2 score.
- U.S. clinical experience is preferred.
- Institutionally, Cleveland Clinic has minimum requirements for all residents.
- Our program sponsors J1 visas for international medical graduates.
Interviews
Invitations for interviews will be sent on or before Friday, November 14, 2025. Those not selected for interviews will be notified if they qualify for our waitlist or not. We do not invite more candidates than we have interview spots available. The program will hold virtual interviews using the Thalamus platform.
Categorical program interviews will be held on the following dates:
- December 3, 2025
- December 5, 2025
- December 10. 2025
- December 17, 2025
- December 19, 2025
Preliminary program interviews will be held on the following dates:
- January 7, 2026
- January 9, 2026
- January 14, 2026
The program will certify the rank list by the first week in February.
Cleveland Clinic site visit dates for categorical applicants will be listed at a later time.
FAQs
Where do the residents live?
Fortunately, Cleveland is very affordable on a resident’s salary. About half of the residents own a house or condo. Most live on the East side, in nearby neighborhoods such as Cleveland Heights, University Heights, Shaker Heights, or Beachwood. The downtown area is also popular for apartment living. There are also beautiful and affordable neighborhoods on the West side, such as Westlake, Ohio City and Tremont. Please visit the GME website for more information about living in Cleveland.
How is life outside of work in Cleveland?
Cleveland has wonderful food, sports, arts and culture. Learn more about the city. If you’re looking for something to do during a visit, check out ThisIsCleveland for some ideas. The program and institution also sponsor a number of social activities throughout the year. These include our welcome picnic, holiday party and graduation. The House Staff Association and House Staff Spouse Association organize several events throughout the year to promote well-being and camaraderie among residents of different specialties.
What is the operative volume for residents?
By the end of their first year, most residents have logged around 100 operations. Our Chiefs graduate with an average of 1,000-1,200 cases and around 120 upper and lower endoscopies. There are no areas of clinical deficiency.
Are residents able to do elective rotations?
Yes. All residents have 1 elective block in the PGY 3, 4 and 5 years to do a rotation that interests them. Additionally, PGY 1 residents have a 1 week elective that can either be used for a supplementary operative experience, or to work in another discipline such as radiology, pathology or with the emergency response team.
Visiting Residents & Students
Visiting resident application
For residents interested in rotating with the Department of General Surgery at Cleveland Clinic, all applications must be submitted by April 15 to be considered for the upcoming academic year.
The GME office requires applications to be submitted no less than 10 weeks prior to the start date of the requested rotation for NEW visiting residents and 4 weeks prior for RETURNING residents.
Please direct any questions to Rebecca Loew (loewr@ccf.org).
For additional GME information, please visit our Graduate Medical Information website.
Visiting students
We welcome students from other institutions to do an elective on one of our clinical teams.
Contact
General Surgery Residency
Lisa Paciorek
Program Manager
216.444.1754
paciorl@ccf.org
Rebecca Loew
Program Manager
216.444.8362
loewr@ccf.org
Graduate Medical Education
Main Office
216.444.5690
1.800.323.9259
Fax: 216.444.6112
Cleveland Clinic Main Line
216.444.2200




