Donor-funded COVID-19 Research Examines Impact of Supplements

In a study funded by philanthropic contributions to Cleveland Clinic’s COVID-19 Response fund, researchers have found that zinc and ascorbic acid (vitamin C), or a combination of the two, do not significantly decrease the severity or duration of symptoms in COVID-19-positive patients, when compared to standard care.
Since the start of the COVID-19 pandemic, there has been widespread speculation about the role of various vitamins and supplements to prevent or treat the disease, but with limited scientific evidence. Zinc,known to be important for immune function, also has a role in antibody and white blood cell production and can fight infections. Vitamin C, an antioxidant, can help reduce damage to cells, and has shown to be immune-boosting.
No Significant Difference Found
The COVID AtoZ clinical trial enrolled 214 adult patients with confirmed COVID-19 infections. Patients were randomized and received either 10 days of zinc gluconate (50 mg), vitamin C (8,000 mg), both agents, or standard care from April 2020 to October 2020. The study was stopped for futility, with no significant difference among the four groups. Specifically, the endpoint of a 50% reduction in symptoms showed no significant difference between the usual care, vitamin C, zinc gluconate or the group receiving both vitamin C and zinc gluconate.
“When we began this trial, there was no research to support supplemental therapy for the prevention or treatment of COVID-19,” says Milind Desai, MD, MBA, Director of Clinical Operations at the Sydell and Arnold Miller Family Heart Vascular & Thoracic Institute and co-principal investigator of the study. “As we watched the pandemic spread across the globe, infecting and killing millions, the medical community and consumers alike scrambled to try supplements that they believed could possibly prevent infection, or ease COVID-19 symptoms, but the research is just now catching up. While vitamin C and zinc proved ineffective as a treatment when clinically compared to standard care, the study of other therapeutics continues.”
The patients enrolled in this study were not hospitalized, but rather managed on an outpatient basis. “We know that not all patients with COVID-19 require hospital admission, and compared to those being treated in a hospital setting, they are more likely to be seeking out supplements that could help them, so it was an important population to study,” says Suma Thomas, MD, MBA, Vice-Chair of Strategic Operations at the Miller Family Heart Vascular & Thoracic Institute and co-principal investigator of the study.
The Impact of Donor Funding
“We are grateful for the generous response from donors to help support our research into treatments and prevention strategies to overcome the novel coronavirus,” says Serpil Erzurum, MD, Chief Research and Academic Officer at the Lerner Research Institute. “Our rapid pivot in response to the COVID-19 pandemic demonstrates our agile, nimble, multidisciplinary team approach that is dedicated to saving lives through pioneering new treatment and prevention methods.”
How You Can Help
Your gift to Cleveland Clinic’s COVID-19 Response fund helps support research saves lives. Please make a gift today.
Southern California Family Supports Lewy Body Dementia Research

“This condition came out of nowhere and just hit us really hard,” says Mark Herthel. “It was so sudden – we didn’t know what was going on; we were shell-shocked. One day he was fine, and the next day he wasn’t.”
Mark is speaking about his father, Doug Herthel, DVM, an internationally respected equine veterinarian. Dr. Herthel made pioneering contributions to colic surgery, fracture repair, stem cell therapy and therapeutic nutrition for horses. In 1972, he and his wife, Sue, founded Alamo Pintado Equine Medical Center just north of Los Angeles, in the Santa Ynez Valley where the family made their home. Dr. Herthel treated Kentucky Derby-winning racehorses and served as President Ronald Reagan’s personal veterinarian.
In early 2017, Dr. Herthel suddenly began hallucinating and experiencing paranoia. Visits to the emergency department and his primary care physician didn’t provide any answers. The family ended up at Ronald Reagan UCLA Medical Center, where Dr. Herthel stayed for 15 days while doctors examined him.
The family was stunned with the eventual diagnosis: Lewy body dementia (LBD).
Mark says his uncle, a veterinarian at the University of Georgia, was the first to mention LBD. “He’d read an editorial written by Robin Williams’ wife about what he had gone through in trying to obtain a diagnosis of LBD and thought the symptoms sounded similar.”Robin Williams ultimately was diagnosed with LBD, but not until a brain autopsy was done after his death, highlighting the challenges in making a diagnosis during life.
Lewy Body Dementia (LBD)
LBD is a broad term covering two separate neurological disorders: dementia with Lewy bodies and Parkinson’s disease dementia. The same biological changes to the brain cause both disorders.
A buildup of Lewy bodies (made up of a protein called alpha-synuclein) causes LBD. Lewy bodies accumulate in neurons located in certain areas of the brain that are responsible for behavior, movement and cognitive ability. It has been estimated that 1.4 million people in the United States are living with LBD, including both dementia with Lewy bodies or Parkinson's disease with dementia. LBD is notoriously difficult to diagnosis, as it shares symptoms with both Alzheimer’s disease (AD) and Parkinson’s disease (PD).
There are no medical tests that can diagnose LBD with 100% accuracy. Specialists, including neurologists, geriatric psychiatrists, neuropsychologists and geriatricians, make the diagnosis of “probable LBD” based on the combined results of tests and patient symptoms.
A Lack of Research
The Herthel family was devastated. Had they missed signs or symptoms of the disease? Could they have done anything to lessen its impact?
Lewy body dementia is less known thanAD, PD and other neurodegenerative disorders. It’s estimated that many cases go undiagnosed or misdiagnosed. While there is no cure for AD or PD, research has led to insights, medications and treatment paths.
After his father's diagnosis, Mark immediately began researching LBD, looking for leaders in the field who could help his father. He came across James Leverenz, MD, Director of Cleveland Clinic Lou Ruvo Center for Brain Health, Cleveland.
Sadly, Dr. Herthel’s disease progressed rapidly, and he passed away in July 2018.
Progress on the Horizon
Mark was impressed with Dr. Leverenz’s work with the Dementia with Lewy Bodies Consortium. Cleveland Clinic Lou Ruvo Center for Brain Health is the coordinating site for a ten-center national collaboration, which was funded by a five-year, $6 million grant from the National Institutes of Health in 2017.
"In neurodegenerative disease research, strength seems to lie in numbers,” says Dr. Leverenz. “Understanding of both AD and PD has benefited substantially from large consortia that have advanced research by harnessing the strengths of multiple academic centers to combine efforts, pool data and develop standardized approaches.We were funded to do the same thing in LBD with a particular focus on developing better ways to diagnose LBD using biomarkers.” Biomarkers are measurable indicators of the presence and severity of a disease and can be critical for developing and guiding new therapies.
In 2018, Cleveland Clinic was also selected by the Lewy Body Dementia Association to be one of 24 U.S. academic medical centers comprising its new Research Centers of Excellence (RCOE) partnership. The overarching goal of the RCOE is to promote research collaboration and guide patients and families to Centers with special expertise in treating LBD.
“After my dad passed away, we really focused on the fact that there isn’t a definitive way to diagnose LBD, measure somebody’s chance of developing it or somebody’s decline after diagnosis. Like many people impacted by LBD, we think it’s unacceptable,” says Mark. “Within days, we were in touch with Dr. Leverenz to see how we could support his biomarker research. We are very interested in supporting a specific cause that means the world to us.”
The Herthel family – Mark, his mother Sue, brother Troy and their families – established the Doug Herthel DVM Memorial Research Fund at Cleveland Clinic in support of Dr. Leverenz’s work into LBD. Their gift has funded the purchase of specialized laboratory instrument platforms for biomarker research, giving Dr. Leverenz, and his collaborator Lynn Bekris, PhD, of the Genomics Medicine Institute at Cleveland Clinic, more flexibility in measuring markers of LBD and other forms of brain neurodegeneration.
“At our veterinarian clinic, there’s a plaque on the wall that says, ‘People don’t care how much you know until they know how much you care,’” Mark says. “All around, we’re very impressed with the quality of care at Cleveland Clinic. Those doctors have just been fantastic, and Dr. Leverenz’s very personal approach is a big part of this.”
He’s also encouraged by the research progress. “We’re confident that breakthroughs will be made in the next several years and that there will be things you can do to slow this thing down. My goal is that with some of the biomarkers that people are working on, we can find intervention strategies.”
How You Can Help
Support from the Doug Herthel DVM Memorial Research Fund had an immediate impact on research into neurodegenerative disorders. As a nonprofit healthcare system, Cleveland Clinic depends on philanthropy to further the work of our researchers and scientists, which makes a difference to patients and families around the world. Your gift will help.
UFC Continues Support of Head Trauma Study with $1M Gift
Growing research shows that cumulative head trauma may result in long-term brain conditions such as chronic traumatic encephalopathy (CTE) and Alzheimer’s disease. This is a particular concern for football players and athletes in other contact sports who risk receiving repetitive blows to the head.
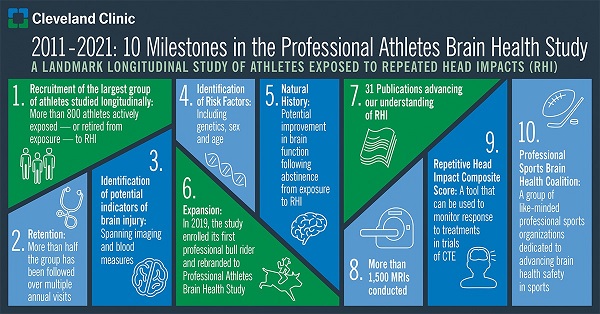
In January 2021, Ultimate Fighting Championship (UFC) announced its continued support of Cleveland Clinic’s Professional Athletes Brain Health Study with a $1 million gift to Cleveland Clinic Lou Ruvo Center for Brain Health.
The Professional Athletes Brain Health Study, led by Charles Bernick, MD, and Aaron Ritter, MD, researches the entire spectrum of repetitive head trauma in both active and retired athletes in sports exposed to repetitive head impacts, such as professional boxers, bull riders and NFL players.
UFC’s commitment to aid in the funding of the Professional Athletes Brain Health Study is provided in conjunction with other organizations in the combat sports industry. Their support facilitates ongoing progress in answering critical questions regarding the long-term effects of exposure to repetitive head injuries that affect athletes competing in sports as well as active-duty military personnel.
Studying Long-term Effects
Now in its 10th year, the study has enrolled more than 800 active and retired athletes. Participation is voluntary. Athletes in the study receive free, ongoing assessments of brain health and function, including MRI scans. Individual tests are repeated annually for a minimum of four years.
The longer an athlete is assessed, the more valuable information will be amassed. Researchers already have detected subtle effects of repetitive head injuries on brain structure and proteins released in the blood following impact. These changes can be measured over time and may be early indicators of brain injury, which could help athletes proactively make informed decisions about their careers based on personal brain health data. Additionally, as CTE researchers nationwide prepare to begin clinical trials, the Repetitive Head Impact Composite Score developed from data in the study will be critical in determining the effectiveness of new therapies.
The next decade of research will focus on social determinants to better understand how the environment impacts the onset of CTE pathology and the role of neuroinflammation in the brain immediately after trauma.
“The key for the next 10 years is to discover which factors are most crucial in each individual,” says Dr. Ritter. “The Professional Athletes Brain Health Study is the largest and longest-lasting study to look at this issue. Without the support of the UFC, a study like this would never happen.”
How You Can Help
Learn more here about the Professional Athletes Brain Health Study and how philanthropic support makes a difference.

