Abdominal pain has many causes, some more serious than others. What feels like a stomachache may be coming from another organ in your abdomen. Or it may be coming from outside your digestive system. Always seek medical care if your abdominal pain is unexplained, severe or doesn’t stop.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Abdominal pain is discomfort anywhere in your belly region — the area between your ribs and pelvis. We often think of abdominal pain as “stomach pain” or a “stomachache.” But pain in your abdomen could be coming from organs other than your stomach.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your abdomen is home to many important organs, including:
These are all organs in your digestive system and urinary system. But pain can also be in your abdominal wall. This is the skin and muscles that make up the outer shell of your abdomen. Sometimes, the pain that you feel in your belly may be coming from somewhere else, like your chest, pelvis or back.
Abdominal pain can take many forms and mean many things. It may be constant, or come and go. You may feel it in one spot or all over. It may feel:
Your abdominal pain is a symptom that only you can describe. Since your healthcare provider can’t measure it, it’s what you say it is. Whether your abdominal pain is serious or mild, your provider will help you find the cause and provide treatment.
There are many different organs in your abdomen. So, your healthcare provider may narrow down the pain you’re having by which area you’re feeling it in. Providers often group your abdomen into quadrants, or four parts. They may ask if your pain is in the:
Advertisement
Location is an important clue to your abdominal pain. But it’s not the only factor. It may tell your healthcare provider which organs are involved. For example, pain in the upper right quadrant may mean you have a problem in your liver or gallbladder.
But your provider will also want to know more about your pain, including:
The answers to these questions give them additional clues about the kind of condition you may have.
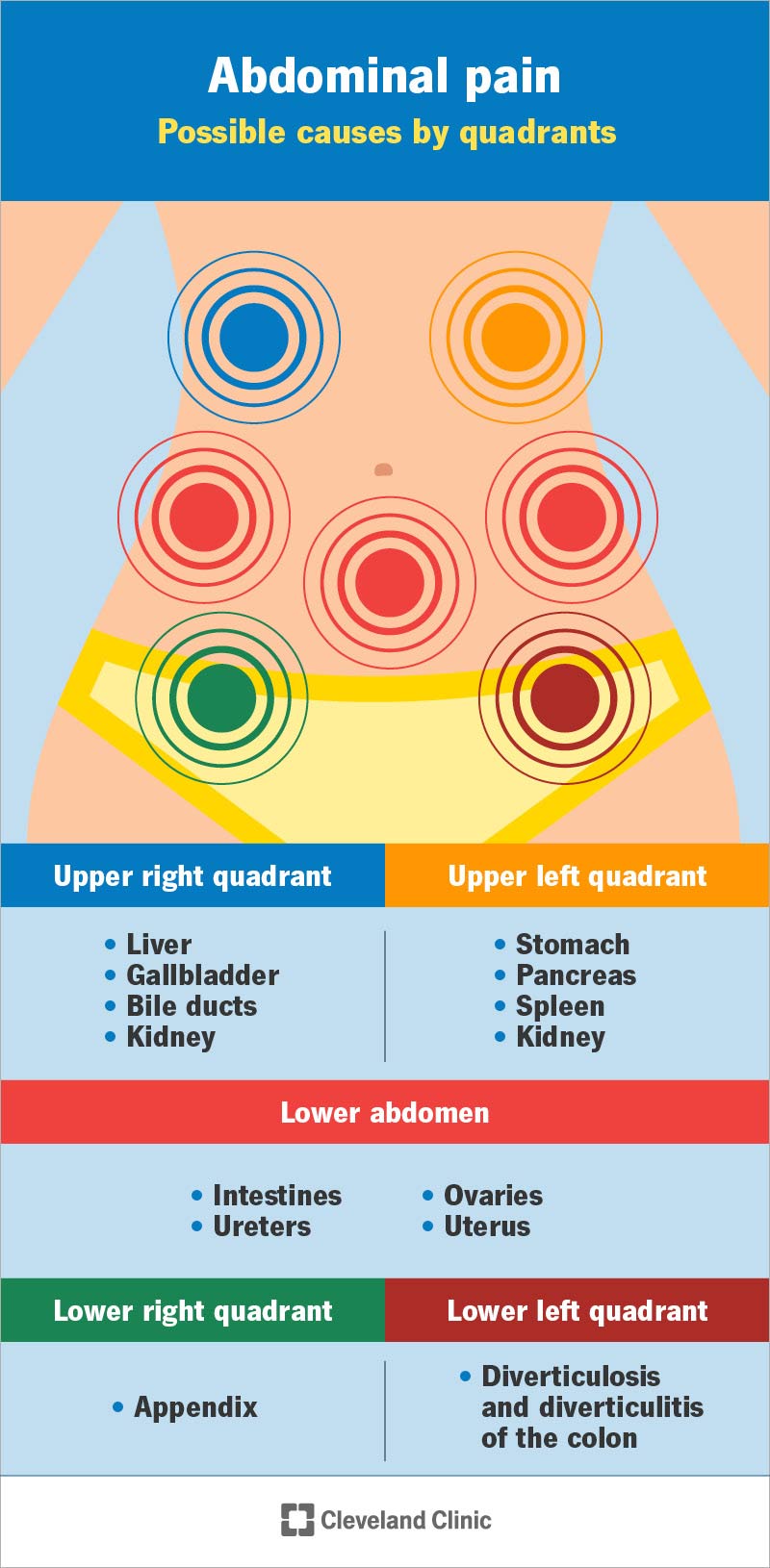
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4167-abdominal-pain)
There are many reasons you may have abdominal pain. It may be related to digestion, injury, infection or disease. It may come from an organ inside your abdominal wall, or from the muscles or skin within it. Or it may have spread from somewhere else nearby.
Your healthcare provider will ask you detailed questions about your pain to figure out the cause. Keep in mind that the level of pain you feel doesn’t always line up with how serious it is. Some common, temporary conditions can cause intense abdominal pain. And some life-threatening, serious conditions may feel mild.
Abdominal pain can feel much worse than others might expect. So, make sure your provider knows exactly what kind of pain you’re in.
Abdominal pain has many causes. Most are short-lived and not serious. They may have to do with digestion, inflammation or menstruation.
Abdominal pain after eating may be due to:
Irritation or infection in your organs can cause temporary inflammation, like:
Causes of female abdominal pain may include:
Sometimes, abdominal pain can mean a more serious medical condition. This can depend on where you’re experiencing the pain. Pain in different areas may mean certain organs are involved. You may have:
Causes of upper right abdominal pain include:
Causes of upper left abdominal pain include:
Causes of lower abdominal pain include:
Advertisement
Pain referred from your pelvic organs could be due to:
Causes of lower left abdominal pain include:
Causes of lower right abdominal pain include:
When you talk to your healthcare provider, let them know which region your pain is in.
Abdominal pain has a wide variety of causes and treatments. For some conditions, you’ll just need medicine to relieve your symptoms. For others, you may need surgery. And sometimes, you just have to get through a bout of stomach flu or a kidney stone until it passes.
If you don’t know what’s causing your abdominal pain, it’s important to find out. This is especially true if it doesn’t go away on its own. Remember that even mild cases can be serious.
Your healthcare provider may ask you to complete an imaging study so they can further evaluate your pain. Depending on the pain location and other factors, imaging tests may include:
If you have a good idea that your stomachache is related to digestion, you can begin by treating yourself with:
Advertisement
For more serious conditions, treatment may include:
You can’t always prevent abdominal pain. But you can take some steps to keep your abdominal organs healthy. You can:
If you have certain health conditions — like lactose intolerance or celiac disease — you may be able to prevent stomach pain. Your healthcare provider may recommend avoiding certain foods or drinks. Talk to your provider before starting any new eating plan.
Always see your doctor if your pain is unexplained, severe or doesn’t go away. Or if you’ve been injured or are pregnant.
Advertisement
Also, see your provider if you have abdominal pain along with:
So many things can cause abdominal pain. So, it’s certain that you’ll experience it from time to time. You may recognize common causes, like abdominal pain and diarrhea. Other causes may be more mysterious. And sometimes, abdominal pain is a sign of an unknown or serious medical condition.
Your healthcare provider can help you figure out what’s causing your pain. They can often treat common causes easily, helping you find relief. Even if your abdominal pain is mild, make sure you see your provider if it doesn’t go away, keeps coming back or gets worse.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
