Metabolic dysfunction-associated steatotic liver disease (MASLD) is when fat builds up in your liver. It once was called nonalcoholic fatty liver disease (NAFLD). MASLD may not cause symptoms. Having obesity or Type 2 diabetes increases the risk of developing it. Losing weight and becoming more active may slow down or reverse liver damage from MASLD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
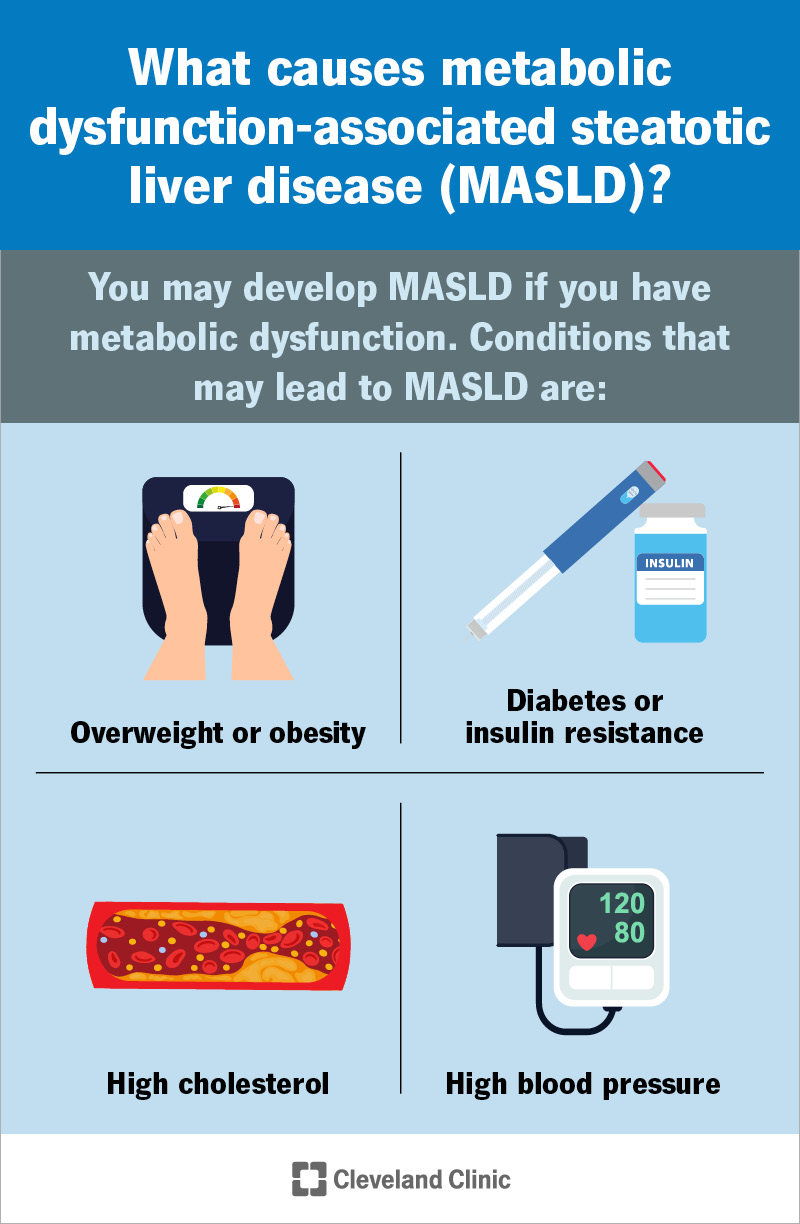
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22437-non-alcoholic-fatty-liver-disease-masld.jpg)
Metabolic dysfunction-associated steatotic liver disease (MASLD) is a group of liver diseases that happen when your body stores lots of fat in your liver (steatotic (fatty) liver disease (SLD). Over time, this fat in your liver can cause inflammation in your liver (hepatitis). Until recently, MASLD was known as nonalcoholic fatty liver disease (NAFLD.)
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
MASLD is one of the most common forms of chronic liver disease. Having obesity or Type 2 diabetes are common causes of MASLD. Given the rising rates of obesity and Type 2 diabetes, experts estimate more than 30% of people worldwide have this condition. Without treatment, MASLD can cause more serious liver diseases. Early diagnosis and treatment can keep MASLD from getting worse.
MASLD develops over several years. You can have it without having symptoms. You may not notice changes in your body unless you develop MASH (metabolic dysfunction-associated steatohepatitis).
MASH causes cirrhosis or severe liver fibrosis. Liver fibrosis is bands of scar tissue in your liver. Some people with MASH have symptoms like:
You may develop MASLD if you have metabolic dysfunction. This is a group of conditions that affect your metabolism. Your metabolism changes food into energy. Conditions that may lead to MASLD are:
Advertisement
Researchers have also found several genetic variations that increase MASLD risk.
Some people with MASLD may develop MASH. The condition can lead to more serious forms of MASH, including:
MASLD may also increase your risk of developing serious conditions like:
Healthcare providers will do certain blood tests and imaging tests (or a liver biopsy).
Your healthcare provider may do imaging tests to look for signs of MASLD in your liver. Tests include:
Occasionally, your provider may perform a liver biopsy. They may do this if they think something other than MASLD causes your symptoms. They may also do a liver biopsy as a follow-up to imaging tests like FibroScan.
Treatment for MASLD usually starts with weight loss. Your healthcare provider will also treat conditions like diabetes, high cholesterol and high blood pressure, which cause MASLD.
Losing weight makes a difference in your liver health. Reducing excess fat in your liver helps with inflammation that leads to cirrhosis. Your provider may recommend meal plans like the Mediterranean diet or the DASH diet.
Doing moderate activity 30 minutes a day for three days a week supports weight loss. Your provider may recommend you lose 10% or more of your body weight. But even losing 3% to 5% of your weight can make a difference.
Your healthcare provider may recommend weight loss medications like GLP-1 agonists if you have diabetes and/or obesity. These medications help lower your blood sugar and help you lose weight. Weight loss medications may include:
Advertisement
Your provider may discuss bariatric surgery with you. Bariatric surgery to support weight loss may reverse MASLD that’s diagnosed before you develop cirrhosis.
Yes, but that depends on your situation. In general, treatment can reverse MASLD unless you have MASH-related cirrhosis.
Receiving a diagnosis early on can help keep MASLD from doing a lot of damage to your liver. Taking steps, like losing weight, may reverse the impact MASLD has on your liver. But your situation depends on your overall health. Ask your healthcare provider whether losing weight can reverse this condition.
Research shows having MASLD can affect how long you’ll live compared with people who don’t have it. For example, one study found the life expectancy for people with MASLD was about 2.8 years lower than the life expectancy for people who didn’t have the disease.
Many things affect how long you’ll live with MASLD. Your situation may be different from others. Your healthcare provider is your best source of information about what you can expect.
This condition often affects people who have obesity or Type 2 diabetes. You may not be able to prevent those conditions from happening. But it’s possible that early diagnosis and lifestyle changes may prevent MASLD.
Advertisement
If you have obesity or Type 2 diabetes, your healthcare provider may recommend blood and imaging tests to screen for signs of this condition. Caught early on, lifestyle changes could reduce your risk.
You can take care of yourself by working with healthcare providers to manage the conditions that lead to MASLD, like having overweight, having obesity and Type 2 diabetes. Losing weight and being active can help slow and possibly reverse liver damage. Here are some other suggestions:
Contact your provider if you notice changes in your body like being more tired than usual or pain in your upper right abdomen. These changes could mean you’re developing MASH, a serious form of fatty liver disease that can lead to cirrhosis and hepatocellular cancer.
Advertisement
No, it doesn’t. Until recently, MASLD was called nonalcoholic fatty liver disease (NAFLD) because you could develop this condition even though you don’t drink a lot of beverages containing alcohol.
That said, people with MASLD who drink beverages that contain alcohol are likely to develop cirrhosis much faster than usual. That’s why healthcare providers typically tell people who have MASLD to avoid beverages that contain alcohol.
A blood test as part of your annual physical shows something is going on with your liver. More tests show you have metabolic dysfunction-associated steatotic liver disease (MASLD). This liver disease can lead to more serious issues.
Lifestyle changes like losing weight and being more active can help keep MASLD from getting worse. Those changes may even reverse the damage done to your liver. But it takes time to lose weight safely. And becoming more active means making a commitment to your health. There may be days when you feel like giving up. Your healthcare team understands the challenge of making changes that don’t show immediate results. Don’t hesitate to ask for help and support.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic providers compassionately diagnose and treat all liver diseases using advanced therapies backed by the latest research.
