Diverticulosis is a common condition that can develop in your colon, especially as you get older. It means that little pouches form in the inside lining of your colon. They usually don’t cause any problems. But rarely, they may bleed or develop an infection (diverticulitis).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
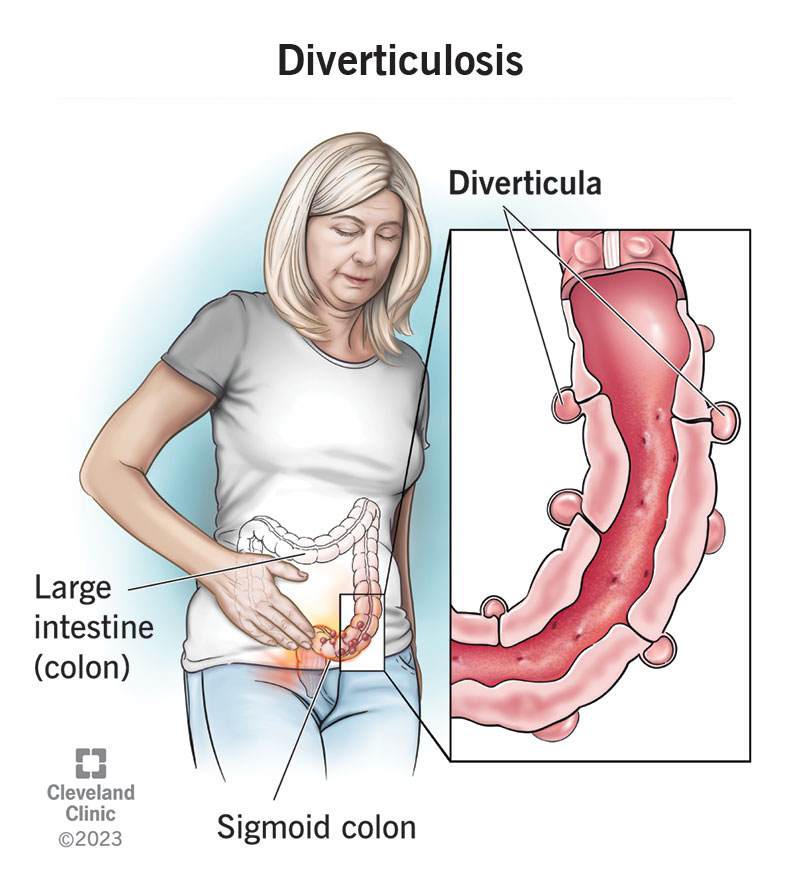
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/24883-diverticulosis)
Diverticulosis is the condition of having small pouches or pockets in the inside walls of your intestines. They develop when the inside lining of your intestines pushes into weak spots in the outer wall. This usually happens gradually over time. As you’re digesting food and food waste makes its way through your intestines each day, it pushes against the weak spots until they eventually begin to cave in.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The term, “diverticulosis,” comes from the word “divert,” indicating that the path through your intestines is diverging into these side pockets. Several pouches are called “diverticula,” and one pouch is called a “diverticulum”. They most commonly occur in your large intestine (colon), which is more likely to have denser food waste pushing against the weak spots, especially towards the end (your sigmoid colon).
Diverticulosis is the condition of having diverticula. Diverticulitis means that there’s inflammation in at least one of your diverticula. This usually means there’s a bacterial infection inside it. Diverticula by themselves may not cause you any trouble, but they can make great breeding grounds for bacteria to hide out and multiply. If you get diverticulitis, it can cause you pain and other symptoms of illness.
Having diverticulosis alone isn’t necessarily a problem. Most people never experience any symptoms or complications from it. It can become serious under rare circumstances. For example, if you develop an infection and it goes untreated for too long, it can lead to complications like sepsis. If you’re one of a small number of people who have frequent bleeding from their diverticula, you could risk serious blood loss.
Advertisement
It’s common in the Western world, especially as you get older. In the U.S., 30% of people over 50, 50% of people over 60 and 75% of people over 80 have diverticulosis. Almost all of them have it in the last part of their colon (sigmoid colon). Diverticulosis is uncommon before the age of 40. It’s also uncommon in parts of the world where the standard diet is less processed than in the West, such as Africa and Asia.
Most people don’t have symptoms from diverticulosis alone. You’re likely to never notice it. If you have symptoms of illness, such as lower abdominal pain or fever, you might have an infection (diverticulitis).
It’s also possible to have symptoms as a side effect of another disease in your intestines that makes your diverticula more sensitive to pressure. For example, if you have irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), food waste passing through your diverticula may cause tenderness or bloating. If you’re prone to constipation, impacted stool may get stuck in the pockets, making it worse.
About 10% of people with diverticulosis may have some diverticular bleeding. This can happen if hard stool passing through a diverticulum erodes or stretches a blood vessel until it breaks. It’s usually temporary and painless, but if it happens, you might see fresh blood in your poop. If you have bleeding, persistent symptoms or complications from diverticulosis, it’s called “diverticular disease.”
Researchers suspect that the leading cause of diverticulosis is the standard Western diet, which is low in plant fiber and high in processed starches. This diet contributes to dense food waste that moves sluggishly through our bowels and fails to sweep them clean on the way. The waste becomes more solid as it travels, which is why it’s most likely to cause diverticulosis in the sigmoid colon (the end part).
It’s possible that genetics are partly involved. Western diet aside, diverticulosis is more common in white Americans, Europeans and Australians than in Black people or other groups. Researchers have also noticed that when people in Asian countries get diverticulosis, they tend to get it in a different part of the colon — the first part, rather than the last. This is also true of the Japanese population in Hawaii.
A healthcare provider may notice the pouches during a routine colonoscopy or GI X-ray exam. This is the most common way of discovering diverticulosis since it usually doesn’t cause symptoms on its own. If you do have symptoms, your healthcare provider will seek to discover the cause in steps. They’ll ask you about your medical history, medications, diet and bowel patterns before examining you.
Advertisement
Exams might include:
Most people won’t need treatment for diverticulosis itself. But your provider might recommend that you begin incorporating more fiber into your diet. This is to address the likely cause of your diverticulosis and to prevent further complications related to constipation, bloating or other symptoms. More fiber will help poop pass more smoothly through your colon and help sweep it clean as it goes.
About 3% of people may need treatment to help stop persistent diverticular bleeding. This usually happens during a colonoscopy. When a gastroenterologist finds bleeding during a colonoscopy, they can pass tools through the colonoscope to seal the broken blood vessel. Alternatively, a provider might use an angiogram to find the bleeding, then treat it by injecting medications into the blood vessel.
Advertisement
If you haven’t had any symptoms or complications from diverticulosis, chances are you never will. If you have another condition that makes diverticulosis more complicated, such as constipation, IBS or IBD, you may be more at risk of chronic symptoms. A small number of people have recurrent bleeding episodes. These people might need repeat treatments to stop the bleeding or manage blood loss.
Once you have diverticula, there’s no known way to make them go away. They won’t cause problems for most people, but if they cause problems for you, you’ll have to adjust your lifestyle to account for them.
Eating more plants and whole foods, getting regular exercise and drinking enough water each day will help keep your bowel movements healthy and regular. This may prevent diverticulosis. If you already have diverticulosis, it may prevent further diverticula from occurring. While it’s not guaranteed, these healthy lifestyle factors help to prevent most types of lower bowel disease.
Whether or not you have any symptoms from diverticulosis, having it means that you could probably benefit from more fiber in your diet. The best way to achieve this is to eat more whole grains, fruits and vegetables. Some people also use fiber supplements, such as psyllium. Make sure to drink enough water with your fiber to help it pass through your colon. Otherwise, it could make constipation worse.
Advertisement
If you have diverticular disease, you’ll need to pay attention to your symptoms to help keep it in check. For example, notice if particular foods cause more discomfort, or if particular medicines you might be taking affect your symptoms. If you notice rectal bleeding, make sure to let your healthcare provider know, even if it stops by itself. They’ll want to make sure you’re not losing too much blood.
You can get diverticula anywhere in your GI tract, including in your small intestine, in your stomach and in your esophagus (esophageal diverticulum). But all of these occurrences are rare. Usually, they’re complications of another disease, such as a motility disorder that makes it difficult for food to pass through the organ normally. Meckel’s diverticulum is a birth defect that occurs in the small intestine.
For most people, diverticulosis is nothing to worry about. A healthcare provider might find it by accident on a routine exam. If you’re over 40, this isn’t remarkable. And if it doesn’t cause symptoms, you can go about your business. If you do have symptoms, be sure to discuss them with a healthcare provider. They might be related to another condition, or you might have developed an infection.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
