Ovarian cancer starts in your ovaries — small organs in the female reproductive system where eggs form. Ovarian cancer is sometimes difficult to detect because symptoms often don’t develop until later stages. Healthcare providers treat ovarian cancer with surgery, chemotherapy and other cancer treatments.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
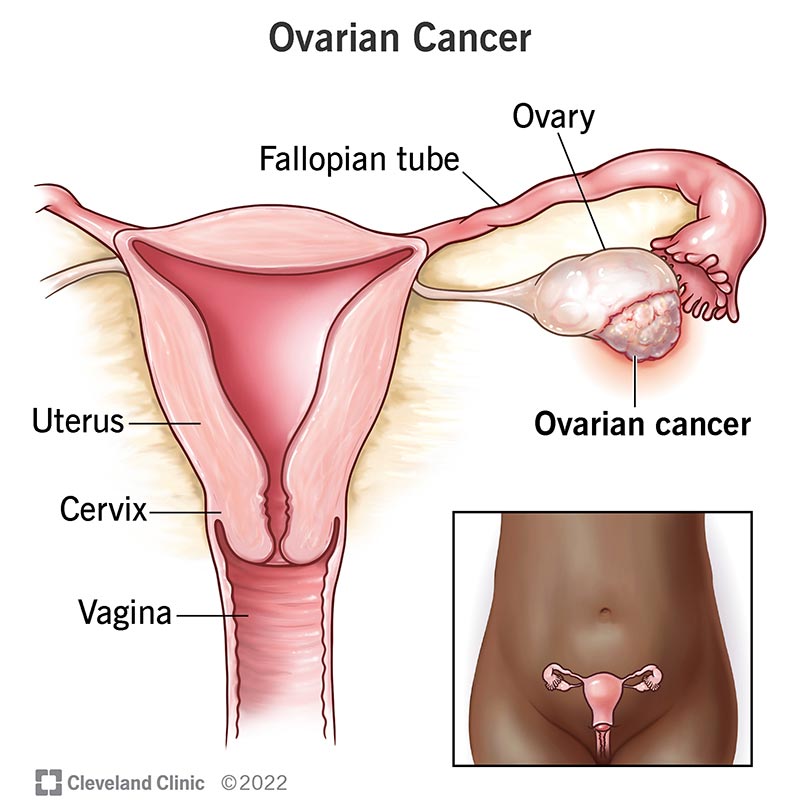
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/4447-ovarian-cancer)
Ovarian cancer occurs when abnormal cells in your ovaries or fallopian tubes grow and multiply out of control.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ovaries are part of the female reproductive system. These two round, walnut-sized organs make eggs during your reproductive years.
Ovarian cancer affects women. It’s slightly more common in Native American and white populations than in people who are Black, Hispanic or Asian.
In addition, people of Ashkenazi Jewish descent are much more likely to have a BRCA gene mutation, placing them at a higher risk for breast and ovarian cancer.
Ovarian cancer accounts for 1% of all new cancer cases in the U.S. The lifetime risk of developing ovarian cancer is approximately 1 in 78.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_ww89qmtv/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Warning signs and risk factors of ovarian cancer.
Ovarian cancer can develop and spread throughout your abdomen before it causes any symptoms. This can make early detection difficult. Ovarian cancer symptoms may include:
If you develop any of the symptoms listed above, schedule a visit with a healthcare provider.
Advertisement
The exact cause of ovarian cancer isn’t yet known. But some people have a slightly higher risk of developing the condition. Ovarian cancer risk factors include:
There’s also an increased risk of developing ovarian cancer as you grow older.
If ovarian cancer spreads, it usually does so from your pelvis to your lymph nodes, abdomen, intestines, stomach, chest or liver.
Despite years of research, experts haven’t yet developed a successful ovarian cancer screening test. For this reason, the condition is often difficult to diagnose in the early stages.
If your healthcare provider suspects ovarian cancer, they’ll ask about your symptoms and perform a pelvic exam. During the exam, they’ll check for any abnormal growths or enlarged organs.
They may recommend additional tests, including:
Providers may use several imaging tests, including:
Blood tests look for a substance called CA-125. High levels of CA-125 in your blood can be a sign of cancer. However, CA-125 levels can be normal, even when cancer is present, and higher in many conditions that aren’t cancer. Because of this, providers use blood tests in combination with other tests to diagnose ovarian cancer.
Providers can diagnose ovarian cancer during surgery. Typically, if they find abnormal growths, they’ll remove them during the same procedure.
During laparoscopic surgery, a surgeon places a thin camera (laparoscope) through a small cut (incision) made in your abdomen. Using the scope as a guide, along with additional ports to hold instruments, the surgeon can assess the cancer, perform staging biopsies and, in some circumstances, remove ovarian tumors.
There are four stages of ovarian cancer. In this cancer staging system, the least severe is the lowest number. The more serious the condition, the higher the number.
Advertisement
Staging is important because it helps your healthcare provider design a tailored treatment plan for you. Your healthcare provider will talk with you about your treatment options.
The goal in treating cancer is to remove as much, if not all, cancer from your body as possible. Common ovarian cancer treatments include:
After you’ve completed ovarian cancer treatment, your healthcare provider will want to see you regularly for observation. You may have routine appointments to check and make sure the cancer hasn’t returned over time. During these appointments, your provider may go through any possible symptoms and do an exam. Be mindful of any symptoms you may be having and tell your provider about them. Sometimes, your provider may order imaging tests, typically a CT scan.
Advertisement
After you’ve received ovarian cancer treatment, your healthcare provider will still see you for regular appointments. During these visits, they’ll check on any symptoms you may have and discuss any concerns. It’s important to pay close attention to your body and let your provider know if anything unusual is happening. Observation is key after ovarian cancer treatment.
The overall five-year survival rate for ovarian cancer is 49%. That means that approximately 49% of people diagnosed with ovarian cancer are alive five years from diagnosis.
It’s important to understand that survival rates are just estimates. They can’t tell you how long you’ll survive or predict the success of your treatment. If you have specific questions about ovarian cancer survival rates, talk with your healthcare provider.
There’s no way to prevent ovarian cancer completely. But knowing your biological family history can help you prepare for any heightened risk of developing ovarian cancer.
If you have a genetic mutation such as BRCA mutation, your healthcare provider may recommend risk-reducing surgery to remove your ovaries and tubes before they become cancerous. If you’re not sure if you have a BRCA or another mutation, ask your healthcare provider about genetic testing.
Advertisement
If you develop signs of ovarian cancer, such as unusual lumps, pain or bloating in your abdomen, schedule a visit with a healthcare provider.
If you’ve received an ovarian cancer diagnosis, you may want to ask your healthcare provider questions such as:
A cancer diagnosis is scary, no matter the type. If you or a loved one has ovarian cancer, you may also feel sad, frustrated or hopeless. Your healthcare provider can help you during this trying time. Ask about resources or support groups (local or online). Getting in touch with others who are going through the same thing can help you process the difficult emotions that often come with a cancer diagnosis.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
An ovarian cancer diagnosis can be shocking and life-changing. Cleveland Clinic cancer experts will help you get the treatment you need.
