Pancreatic cancer affects your pancreas, a gland in your abdomen that aids in digestion. Pancreatic cancer symptoms include nausea, bloating, fatigue, jaundice and lack of appetite. Treatments include surgery, chemotherapy and radiation therapy. Pancreatic cancer survival rates are low because the disease is difficult to detect in the early stages.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
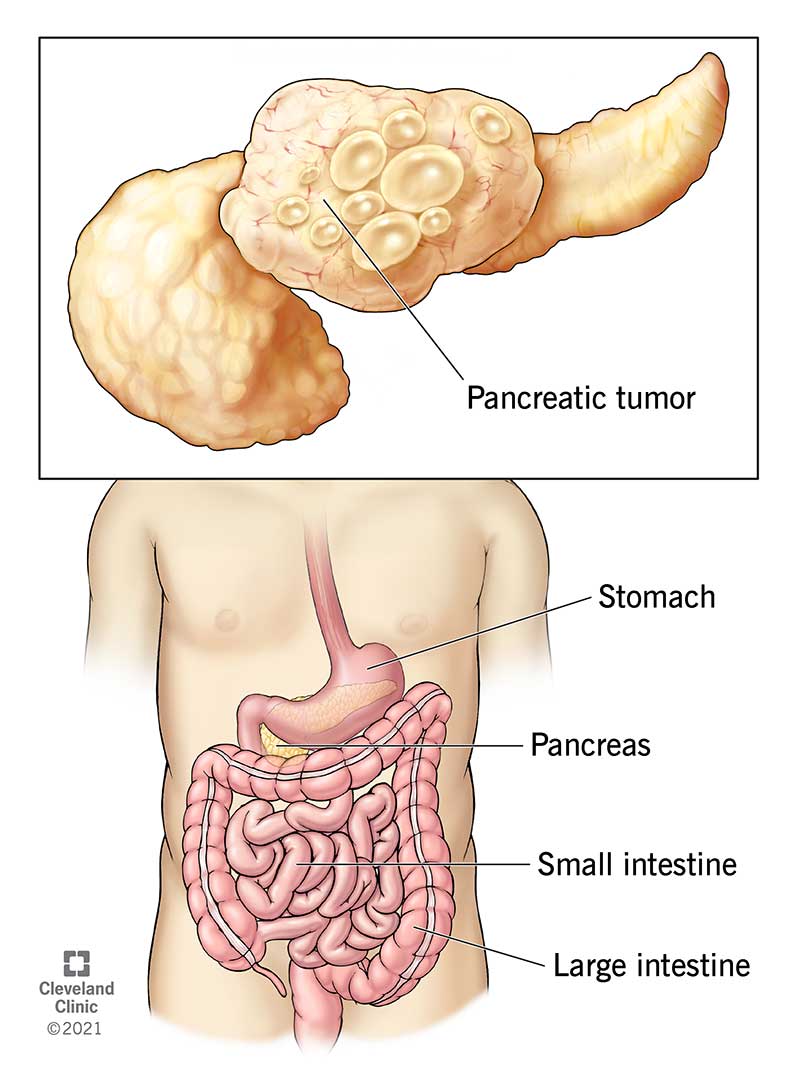
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21786-pancreatic-cancer-illustration)
Pancreatic cancer occurs when cells in your pancreas mutate (change) and multiply out of control, forming a tumor. Your pancreas is a gland in your abdomen (belly), between your spine and stomach. It makes hormones that control blood-sugar levels and enzymes that aid in digestion.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Most pancreatic cancers start in the ducts of your pancreas. The main pancreatic duct (the duct of Wirsung) connects your pancreas to your common bile duct.
Early-stage pancreatic tumors don’t show up on imaging tests. For this reason, many people don’t receive a diagnosis until the cancer has spread (metastasis). Pancreatic cancer is also resistant to many common cancer drugs, making it notoriously difficult to treat.
Ongoing research focuses on early detection through genetic testing and new imaging methods. Still, there’s much to learn.
There are two main types of pancreatic tumors:
Pancreatic cancer is responsible for approximately 3% of all cancers in the United States. It’s the 10th most common cancer in men and the 8th most common cancer in women.
Cases of pancreatic cancer are on the rise. Trends indicate that pancreatic cancer will be the second leading cause of cancer death in the United States by 2030.
Advertisement
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_hk0ofhgx/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Warning signs of pancreatic cancer and how to spot them.
Unfortunately, there aren’t any early signs of pancreatic cancer. Symptoms typically emerge once the tumor starts impacting other organs in your digestive system.
Pancreatic cancer symptoms may include:
Your healthcare provider might suspect pancreatic cancer if you’ve recently developed diabetes or pancreatitis — a painful condition due to inflammation in your pancreas.
Symptoms of pancreatic neuroendocrine cancer may be different from traditional pancreatic cancer symptoms, such as jaundice or weight loss. Symptoms can vary, but may include diarrhea and anemia.
There are no tell-tale early signs of pancreatic cancer. Some people develop vague symptoms up to one year before they receive a diagnosis.
Many people report that their first pancreatic cancer symptoms were back pain or stomach pain. These symptoms can come and go at first, but may get worse after meals or when you lie down.
There isn’t a clear answer. We don’t know exactly what causes pancreatic cancer. But experts have identified some risk factors.
A risk factor is something that increases your chances of getting a certain disease. Common pancreatic cancer risk factors include:
Pancreatic cancer tends to spread (metastasize) to nearby blood vessels, lymph nodes, and then to your liver, peritoneum (the lining of your abdominal cavity) and lungs.
The majority of pancreatic cancers have already spread beyond the pancreas at the time of diagnosis.
It’s difficult to detect pancreatic cancer in the early stages. This is because healthcare providers can’t feel your pancreas during routine exams and it’s difficult to see these tumors on routine imaging tests.
Advertisement
If your provider suspects pancreatic cancer, they’ll recommend a combination of pancreas function tests, which may include:
Your healthcare provider may need to take one or more of the following imaging tests:
A pancreas blood test can detect tumor markers. A tumor marker is a substance that may indicate the presence of cancer.
For pancreatic cancer, high levels of carbohydrate antigen (CA) 19-9 — a type of protein released by pancreatic cancer cells — might indicate a tumor.
Sometimes, providers use laparoscopy to determine the extent of pancreatic cancer and whether removal is possible.
During this procedure, a surgeon creates a few small incisions (cuts) in your abdomen and inserts a long tube with a camera on the end. This allows them to see inside your abdomen and look for abnormalities. Often, they’ll take a biopsy during the same procedure.
If you receive a pancreatic cancer diagnosis, you should consider genetic testing. This can tell you if there’s a hereditary reason you developed pancreatic cancer. It can also help your healthcare provider determine which type of treatment will be most effective for you.
Advertisement
Some people with pancreatic cancer have mutations in genes BRCA1 and BRCA2. Though you may recognize these genes as the “breast cancer genes,” mutations in BRCA1 and BRCA2 may also indicate other types of cancer, including prostate, ovarian and pancreatic.
If you’re a first-degree relative (a parent, child or sibling) of someone who has pancreatic cancer, you should consider genetic testing. Your results can tell you if you have a BRCA1 or BRCA2 gene mutation. Keep in mind, even if you have the mutation, it doesn’t mean you’ll get cancer. But knowing your risk is important.
Healthcare providers rank pancreatic tumors into four different categories:
Advertisement
If you have specific questions about pancreatic cancer staging, talk to your healthcare provider. Understanding your pancreatic cancer diagnosis can help you make an informed decision about your treatment.
Even though pancreatic cancer has a poor survival rate, complete remission is possible with early detection and treatment. The only way to realistically cure pancreatic cancer is total surgical removal of the cancer.
Specific treatment depends on certain factors, including:
Pancreatic cancer treatments include:
Surgery is the only realistic way to cure pancreatic cancer. But surgeons only recommend it when they think they can remove all of the cancer. Otherwise, there’s little to no benefit.
For surgery to be successful, the cancer must be completely confined to the pancreas. Even then, total cancer removal may not be possible.
There are a few different surgical techniques, depending on the location and size of the tumor:
If the tumor is in the head of your pancreas (the widest part of your pancreas, near your small intestine), your provider may recommend the Whipple procedure. This surgical approach removes the head of your pancreas, your duodenum (the first portion of your small intestine), your gallbladder, a portion of your bile duct and nearby lymph nodes.
Your surgeon will then attach your remaining bile duct and pancreas to your small intestine. This reestablishes your digestive tract.
If the tumor is in the tail of your pancreas, a surgeon can perform a distal pancreatectomy. During this procedure, a surgeon removes the tail of your pancreas and some of the pancreas body. In most cases, they’ll also remove your spleen.
As your spleen helps fight infections, your healthcare provider may recommend getting certain vaccinations before having a distal pancreatectomy.
If cancer has spread throughout your entire pancreas, but resection (removal) is still possible, your healthcare provider may consider a total pancreatectomy. This surgery removes your entire pancreas, gallbladder, spleen and part of your stomach and small intestine.
It’s possible to live without a pancreas, but it can cause major side effects. Your pancreas makes insulin and other hormones that keep blood sugar at a safe level. Without a pancreas, you’ll develop diabetes and need insulin shots to survive. Additionally, you’ll need to take pancreatic enzyme pills to help with digestion.
Chemotherapy uses drugs that kill cancer cells. Healthcare providers give these drugs in pill form or through an IV in your arm.
Providers use chemotherapy as a stand-alone treatment — especially for people with advanced pancreatic cancer. They may also recommend chemotherapy before surgery to shrink the tumor or after surgery to kill any remaining cancer cells.
Radiation therapy uses high-energy X-rays to kill cancer cells. Healthcare providers commonly use this approach to treat pancreatic cancer.
Most often, providers combine radiation therapy with chemotherapy (chemoradiation). They may recommend it before surgery, after surgery or as part of your main cancer treatment. Radiation therapy can also help ease pancreatic cancer symptoms in people who don’t qualify for surgery (in cases of advanced cancer).
This treatment uses drugs that “target” certain proteins. These proteins control how cancer cells grow and spread. Providers may combine targeted therapy with other treatments like radiation therapy.
Common targeted therapy drugs for pancreatic cancer include:
Pancreatic cancer could be very painful as it may involve nearby nerves. Your healthcare provider can help you manage pain with oral medications, anesthesia or steroid injections.
If you have pancreatic cancer and start to develop severe and persistent pain, tell your healthcare provider. They can find a treatment that will ease your symptoms.
A pancreatic cancer diagnosis can feel overwhelming. Because everyone is unique, no two cases are the same. Your healthcare provider will assemble a team of experts to determine the best treatment plan for your situation. Your medical team may include:
Generally, it takes about 10 to 20 years for a single cancer cell in your pancreas to turn into a tumor. The goal of ongoing research is to determine how healthcare providers can detect pancreatic cancer in its earliest stages, when it’s more treatable.
In the United States, the five-year survival rate for people with pancreatic cancer is 11%. This means that 11 out of 100 people are still alive five years after their diagnosis.
Survival rates are only estimates. They can’t tell you how long you’ll live or how well you’ll respond to treatment. If you have specific questions about survival rates and what they mean for you, talk to your healthcare provider.
You can’t prevent pancreatic cancer. But there are things you can do to lower your risk:
Healthcare providers don’t usually perform routine screenings for pancreatic cancer. But in people with a high risk of pancreatic cancer due to genetic predisposition, providers recommend monitoring with imaging tests and endoscopic ultrasounds.
If you have a first-degree family member (parents or siblings) with pancreatic cancer, you should talk to a healthcare provider about your risk of developing pancreatic cancer and proper screening and genetic tests.
There are no clear-cut symptoms for early-stage pancreatic cancer. However, you should see a healthcare provider right away if you develop:
Develop an open and cooperative relationship with your healthcare provider. If you or a loved one received a pancreatic cancer diagnosis, here are some questions you may want to ask:
As pancreatic cancer progresses, you may develop new symptoms. Advanced pancreatic cancer symptoms may include:
A pancreatic cancer diagnosis can be shocking and life-changing. Your healthcare provider is here to help you navigate this difficult time. You might consider joining a local or online support group for people with pancreatic cancer. Spending time with others who are going through the same things can be empowering and beneficial for your mental and emotional health. You can also talk with a counselor, therapist or social worker about how you’re feeling. Knowledge is power, and there are several helpful resources available for you and your family.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A pancreatic cancer diagnosis can make your world tilt. Cleveland Clinic experts are here to start personalized treatment for the best possible outcome.
