Pancreatitis is inflammation in your pancreas. It’s usually temporary (acute) but can also be a life-long (chronic) condition. The most common symptom is abdominal pain. The most common causes are alcohol use and gallstones.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
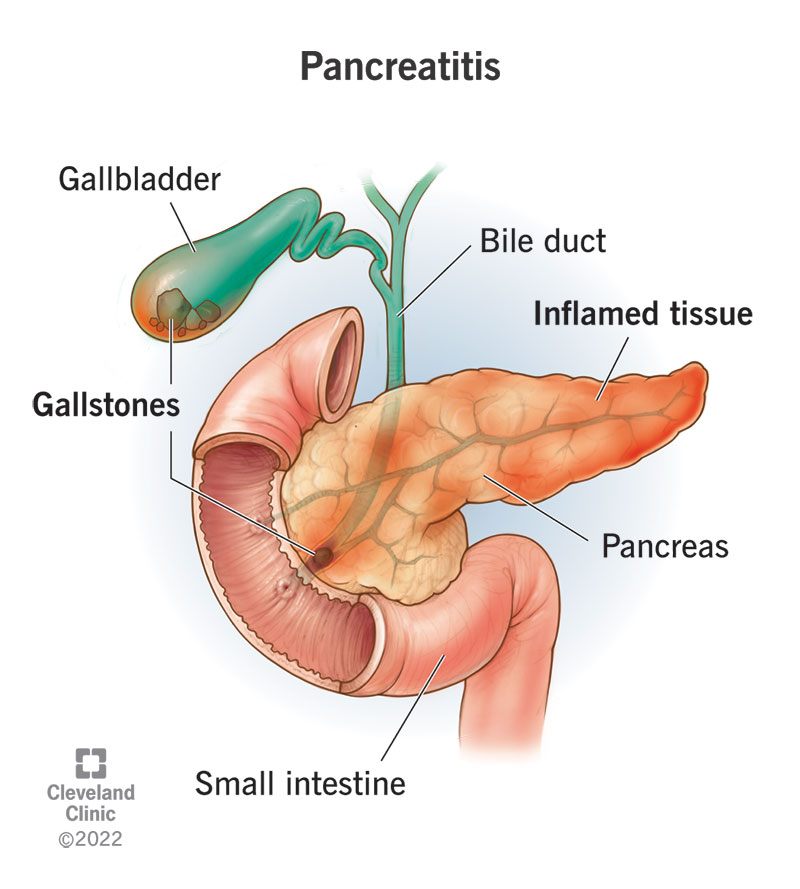
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/8103-pancreatitis-illustration)
Pancreatitis is inflammation in your pancreas. Inflammation causes swelling and pain. If you have pancreatitis, it might feel like stomach pain that spreads to your back.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your pancreas is an organ in your abdomen. It sits between your stomach and your spine. If you lay your right hand across your stomach, that's roughly the size and shape of your pancreas behind it.
Your pancreas is involved in digestion and regulating your blood sugar. It makes digestive enzymes (like amylase) and hormones (like insulin). It delivers digestive enzymes to your small intestine through the pancreatic duct.
Inflammation is your immune system’s response to injury. It’s supposed to help heal injured tissues. When your pancreas is injured, it’s most often from gallstones blocking the pancreatic duct, or from alcohol.
There are two types of pancreatitis: acute and chronic.
Acute pancreatitis is a temporary condition. It happens when your pancreas is attempting to recover from a minor, short-term injury. Most people with acute pancreatitis will recover completely in a few days with supportive care: rest, hydration and pain relief. However, a very severe case of acute pancreatitis can cause serious health complications, some of them life-threatening.
Chronic pancreatitis is a long-term, progressive condition. It doesn’t go away and gets worse over time. It happens when the injury or damage to your pancreas never stops. Chronic pancreatitis will eventually do lasting damage to your pancreas, although it may take many years. Constant inflammation causes scarring of your pancreas tissues (fibrosis), which stops them from making enzymes and hormones.
Advertisement
In the U.S., acute pancreatitis leads to 275,000 hospital stays per year. About 20% of these cases are considered severe. Chronic pancreatitis is less common and leads to 86,000 hospital stays per year.
The primary symptom of pancreatitis is abdominal pain.
Additional symptoms of acute pancreatitis may include:
Additional symptoms of chronic pancreatitis may include:
These are symptoms of your pancreatic functions beginning to break down.
Abdominal pain from pancreatitis may be moderate to severe and may radiate to your back. Acute pancreatitis tends to be more severe, with a penetrating quality. Your abdomen may feel tender to the touch. With chronic pancreatitis, the pain may vary in intensity. It may come and go, but it typically doesn’t go away completely. You may notice it more after eating. For some people, the pain is constant.
It may feel worse when you:
It may feel better when you:
When long-term, chronic pancreatitis begins to affect your pancreatic function, you’ll notice it in your digestive system first. When your pancreas can no longer make and deliver its digestive enzymes, your body won’t be able to break down and absorb all the nutrients from your food. You may feel discomfort after eating and may begin passing undigested fats in your poop. Over time, you may notice weight loss.
The top two causes of pancreatitis are:
These causes together represent about 80% of pancreatitis cases.
Your common bile duct empties bile from your gallbladder into your intestine through the same opening as your pancreatic duct. If a gallstone enters the common bile duct and gets stuck at that junction, it can temporarily block the drainage of pancreatic juice from the pancreatic duct. This traps the enzymes inside your pancreas. As pressure builds up behind the obstruction, it activates the enzymes inside your pancreas and they begin digesting the pancreas itself. This causes the inflammatory response of gallstone pancreatitis.
Heavy alcohol use is another clear cause of pancreatitis, though scientists aren’t sure why. It may be that the toxic byproducts of alcohol in your blood cause an inflammatory response in your pancreas, or they somehow chemically activate the digestive enzymes inside your pancreas. Scientists estimate that heavy alcohol use accounts for around half of both acute pancreatitis and chronic pancreatitis cases.
Advertisement
Less common causes of pancreatitis include:
These causes together represent about 20% of pancreatitis cases. Occasionally, no cause is found.
Most of the time, pancreatitis is acute and temporary. But causes that are chronic and don’t go away, such as inherited disorders, can cause chronic pancreatitis. Repeat episodes of acute pancreatitis can also lead to chronic pancreatitis. If your pancreas becomes inflamed too many times from repeated stress and injury, your body may learn to keep it constantly inflamed, even after the injury has stopped.
You can die from complications of acute pancreatitis if it’s very severe. In a small percentage of people, severe acute pancreatitis causes a systemic reaction that affects the whole body. This can lead to shock and multiple organ failure, which can be fatal if it isn’t treated quickly. You may not be able to tell how severe your pancreatitis is, so you should go to the emergency room if you have symptoms.
Advertisement
Most cases of acute pancreatitis don’t have complications, but 1 in 5 cases is more severe. It’s not clear why severe acute pancreatitis occurs in some cases and not others. A severe case can lead to serious complications, including death. Chronic pancreatitis also causes complications, but they develop more slowly and aren’t directly life-threatening. Most complications are manageable with treatment.
Complications of severe acute pancreatitis include:
Advertisement
Complications of chronic pancreatitis develop over time and can include:
If you have characteristic symptoms of pancreatitis, a healthcare provider will check your pancreas with blood tests and imaging tests. A pancreas blood test looks for elevated levels of pancreatic enzymes in your blood. If levels are at least three times higher than normal, your provider will suspect pancreatitis. They might confirm the diagnosis with a cross-sectional imaging test, such as a CT scan or MRI. These tests can show swelling and fluid deposits in your pancreas as well as other abnormalities.
If your provider suspects you have chronic pancreatitis, they may order additional tests, including:
Treatment depends on the cause, whether it’s acute or chronic and how severe it is. In general, you should always see a healthcare provider for symptoms of pancreatitis. Although some cases of acute pancreatitis may go away on their own, that depends on what caused the condition and how severe it is. In the meantime, most people with acute pancreatitis will need pain relief to get through it. Some people will need emergency treatment for certain causes. And some will need intensive care for complications.
Treatment for acute pancreatitis may include:
If the cause has been resolved and you don’t have severe or complicated pancreatitis, care will focus on supporting your body’s natural healing process. This usually includes:
If you have gallstone pancreatitis, your provider may need to remove an impacted gallstone from your bile ducts. They’ll also recommend gallbladder removal surgery to prevent gallstones from causing you future problems. Procedures may include:
If you have complications, you may also need:
If you have chronic pancreatitis, your general healthcare provider may refer you to a specialist (gastroenterologist). Treatment for chronic pancreatitis begins with pain management and lifestyle changes to slow down the progression of the disease. Eventually, you may need enzyme supplements and insulin injections to replace the enzymes and insulin your pancreas no longer produces.
If you have chronic pancreatitis, it’s paramount that you quit drinking alcohol and quit smoking. These factors both contribute greatly to pancreatitis and will speed up the progression of the disease. Your healthcare provider can connect you with resources to help you quit. It’s also important to maintain a low-fat diet with plenty of fruits and vegetables and to drink plenty of water each day.
Long-term pain management can be complex. You may need to experiment with a variety of different medications and procedures to find what works for you. Make sure to stay in touch with your healthcare provider about your pain, especially if what you’re doing isn’t working. They can refer you to a chronic pain specialist to help you manage your pain. In some cases, endoscopic procedures to remove scar tissue or pancreas stones may improve your symptoms. Injection of local anesthetic agents into the nerves of the pancreas (celiac plexus block) is another option for selected patients.
Over time, many people with chronic pancreatitis can develop exocrine pancreatic insufficiency (EPI). These people will need to take pancreatic enzymes in supplement form. You might also need to take nutritional supplements to get enough calories and micronutrients (vitamins and minerals). Some people will develop glucose intolerance and eventually diabetes, becoming insulin-dependent.
If severe inflammation is concentrated in a specific part of your pancreas and that part is causing unmanageable pain or complications, your provider might suggest surgery to remove that part of your pancreas (resection). In very advanced cases, when your pancreas has been severely damaged and still causes significant pain, they might recommend removing the whole pancreas (total pancreatectomy).
Most people recover completely from acute pancreatitis. If it’s not a severe case, you’ll feel better in five to 10 days. In severe or complicated cases, you may need to stay in the hospital for several weeks. If you’re able to avoid what caused your acute pancreatitis in the future, chances are good it won’t occur again. Among the small percentage of people who experience organ failure, the mortality rate is 20%.
Chronic pancreatitis is a slow-progressing disease. With regular care, you can keep track of its progression and stay ahead of its complications. Pain management can become a challenge for some people, and it can also affect your mental health and quality of life. When this is the case, surgery might be an option. You can live without your pancreas, although it may make you insulin-dependent.
Not all causes are preventable, but you can reduce your risk by moderating your alcohol consumption. You can reduce your risk of gallstones, the other leading cause, by reducing cholesterol. If you’ve had acute pancreatitis, you can help prevent it from happening again by quitting alcohol and smoking. If you’ve had gallstone pancreatitis, removing your gallbladder can prevent it from recurring.
You may not think much about your pancreas, until one day it starts hurting. This can be a frightening and stressful way for the organ to grab your attention. Hopefully, it’ll be a one-time event. When you experience symptoms, head to the hospital. Most cases of acute pancreatitis are over in days. If you know what caused it, and you can avoid it, you probably won’t need a second warning to do so.
Chronic pancreatitis may come on more gradually and may take longer to notice. While some causes, such as alcohol use, are predictable, others are unusual and unexpected. You may have never imagined you were at risk of developing a chronic disease. Regardless, learning to live with it can be challenging. You’ll need a healthcare provider you can trust to help you manage it over the course of your life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
