Functional dyspepsia is a kind of chronic indigestion. It involves frequent stomachaches and a feeling of fullness or bloating after eating. A healthcare provider may diagnose you with functional dyspepsia if they can’t find any direct cause for your symptoms. There are many treatment options, but there’s no one solution that works for everyone.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
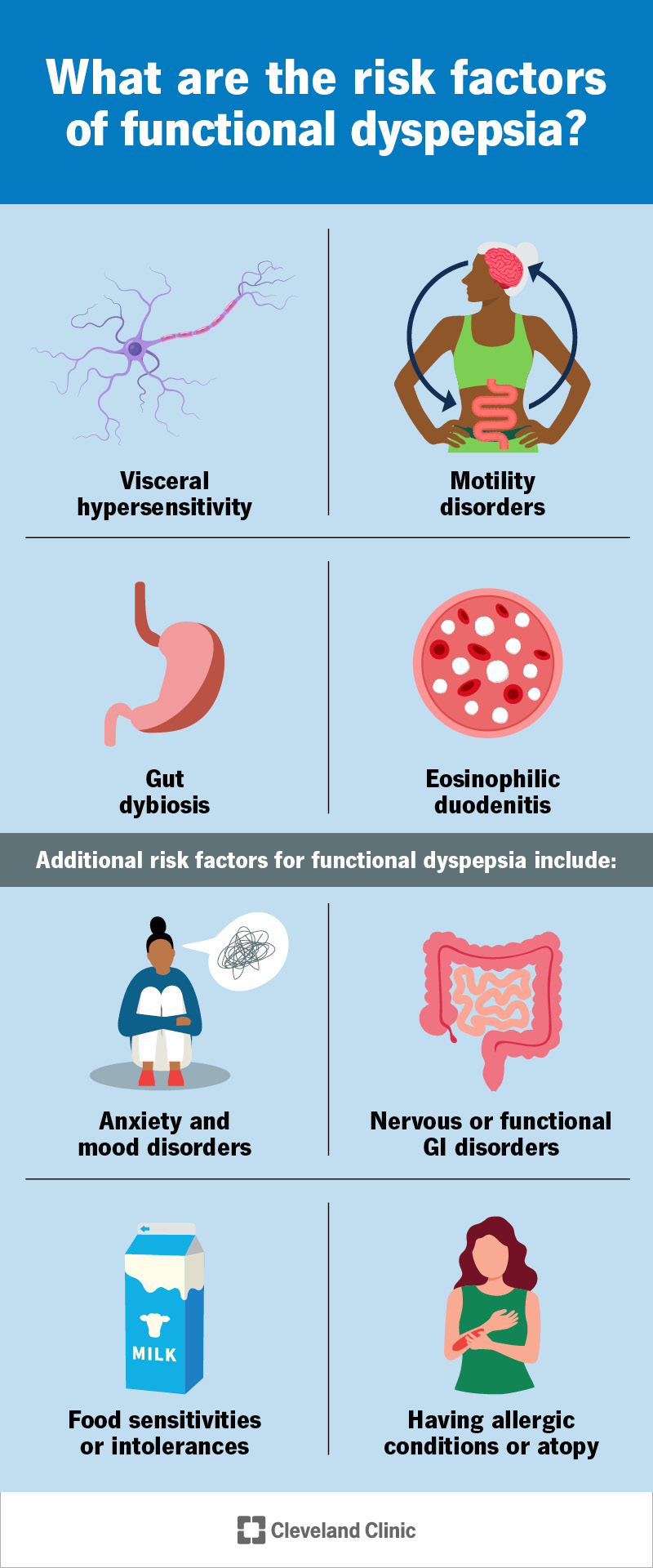
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22248-functional-dyspepsia.jpg)
Functional dyspepsia is chronic indigestion with no identifiable cause. “Dyspepsia” is another word for indigestion — a pattern of symptoms that occur together after eating and while you’re digesting. “Functional” means that your dyspepsia symptoms can’t be explained by the usual physical causes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Typical symptoms of dyspepsia include burning stomach pain, over-fullness and bloating. These symptoms resemble peptic ulcer disease or GERD. But after testing, only a fraction of people with dyspepsia are diagnosed with these conditions. The rest are diagnosed with functional dyspepsia.
Dyspepsia is more of a syndrome than a condition — it’s a pattern of symptoms that occur together. But different people can have different combinations of symptoms with it. Healthcare providers have identified two distinct ways that people can experience functional dyspepsia. They classify these as:
Not everyone fits these into profiles. Some people experience both types or a mix.
Functional dyspepsia symptoms typically include:
Advertisement
Additional or related symptoms may include:
Healthcare providers diagnose “functional” gastrointestinal disorders when they can’t find a direct cause for your symptoms. This might happen because of the close connection between your gut and brain. Functional disorders seem to involve your nervous system and how you perceive pain or discomfort.
While there’s no single cause of functional dyspepsia, several factors might be involved. These include:
Additional risk factors for functional dyspepsia include:
Healthcare providers diagnose functional dyspepsia by confirming your symptoms and ruling out other causes. These include chronic acid reflux (GERD) and peptic ulcer disease. In some cases, you may already have one of these diagnoses. But treating the condition hasn’t relieved your symptoms.
Functional dyspepsia symptoms can be sporadic. Providers only diagnose it if they:
Once they’ve confirmed you have dyspepsia, they’ll look to rule out structural causes.
Tests might include:
Advertisement
If tests reveal any underlying factors, like bacterial overgrowth or a motility disorder, your provider will treat those first. But usually, treating these isn’t enough to relieve functional dyspepsia. Your provider will suggest other treatment options to relieve your symptoms. It usually takes a combination of these.
Medications for functional dyspepsia might include:
Complementary medicine for functional dyspepsia might include:
For most people, functional dyspepsia is a chronic condition that comes and goes throughout their lives. It may take some trial and error to figure out which therapies and habits improve your symptoms. While you may find some relief, it may never go away completely. But it doesn’t cause serious harm.
Advertisement
See your provider if:
With no definitive cause or cure, functional dyspepsia can be a frustrating diagnosis for people looking for answers. Functional GI disorders are complex. They involve your brain and nervous system, diet and lifestyle, and possibly hidden causes in your body. That’s what makes them so tricky to manage.
Medical testing can help by identifying or ruling out certain contributing factors. But in the end, you’re the one in the best position to notice what makes your symptoms better or worse. As you try out different therapies and isolate your triggers, you’ll find your own way to live with functional dyspepsia.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Chronic indigestion can affect your daily routine or make you feel worried and anxious about eating. We can help with treatments to bring relief.
