Cholecystitis is inflammation in your gallbladder, an organ in your upper right abdomen. Your gallbladder stores and distributes bile through your bile ducts. When a gallstone gets stuck in your bile duct, it can cause bile to back up into your gallbladder. This can cause swelling, pain and other complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
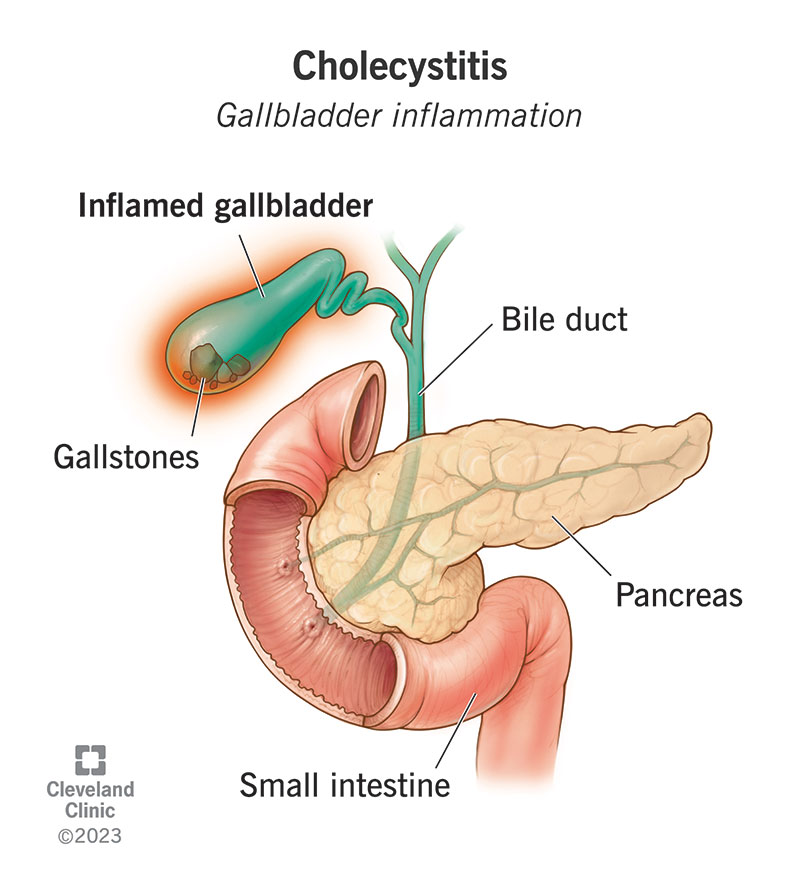
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/15265-cholecystitis-gallbladder-inflammation)
Cholecystitis (KO-leh-sis-TY-tiss) is inflammation in your gallbladder, the small, pear-shaped organ that lives under your liver and stores the bile your liver makes. Your gallbladder sends bile to your small intestine after you eat to help digest fats. It sends and receives bile through tiny pipelines called bile ducts. An infection or obstruction in your gallbladder or the bile ducts connected to it can cause inflammation, pain and swelling inside it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Gallbladder inflammation can be:
An inflamed gallbladder can be an immediate response to an urgent problem, or a slow response to a long-term problem. This is the difference between acute cholecystitis and chronic cholecystitis.
Gallstones are usually the cause of both chronic and acute cholecystitis. So, most cases are “calculous”. Healthcare providers use “acalculous” to distinguish cholecystitis that’s not related to gallstones.
About 15% of the world’s population has gallstones, and about 20% of these will have complications from gallstones, which include cholecystitis. Gallstones cause 95% of all cholecystitis cases.
Common symptoms of acute cholecystitis include:
Advertisement
Additional symptoms may include:
Chronic cholecystitis symptoms tend to be less severe, and they come and go. You might have an episode of biliary colic — abdominal pain with nausea — after a rich or heavy meal. Fatty foods require more bile to digest. Your digestive system signals to your gallbladder to send more bile, which causes it to squeeze harder, increasing the pressure inside it. You might feel this for a few hours afterward.
Gallstones blocking your bile ducts are the most common cause of cholecystitis, both chronic and acute. Gallstones are pieces of hardened bile residue. They usually form at the bottom of your gallbladder, but they can also travel. Sometimes, they can get stuck in a bile duct or in the opening to your gallbladder. This causes bile to back up into your gallbladder. It also can encourage infections inside it.
A gallstone that obstructs the flow of bile from your gallbladder will cause acute cholecystitis. This type gets steadily worse as your gallbladder swells more and more. A drifting gallstone may partly obstruct your gallbladder in an on-and-off way. For example, you may feel it only occasionally, when your gallbladder squeezes out bile to help digest a heavy meal. This can cause chronic cholecystitis.
While a gallstone causing an obstruction is the most common reason why bile flow may slow and back up into your gallbladder, there are other ways this might happen. For example:
These conditions develop slowly, so they’re more likely to cause chronic cholecystitis. But they can get steadily worse, and chronic acalculous cholecystitis can progress to acute acalculous cholecystitis.
Other possible causes include:
Advertisement
You’re more likely to get cholecystitis if you have gallstones. You’re more likely to have gallstones if you:
Acute cholecystitis is usually caused by something blocking the flow of bile. This can affect more than just your gallbladder. A blockage in your biliary system — the system of organs that exchange bile through your bile ducts — can cause inflammation and possibly infection throughout. Backed-up bile can overflow into your bloodstream, making you sick. Your digestive system also won’t get the bile it needs.
Severe inflammation and swelling in your organs can cause tissue death (gangrene), which can cause the organ to split or tear (gangrenous cholecystitis). Chronic cholecystitis tends to be less severe, but long-term inflammation can still do serious damage. Your gallbladder may develop scar tissue inside, which may make it unable to contract effectively. This can also cause your bile flow to stall.
Advertisement
A healthcare provider will start by asking you about your symptoms. If they suspect cholecystitis, they might check for it by asking you to take a deep breath while they gently press on your upper right abdomen. If this is painful, it’s a classic sign of cholecystitis (Murphy’s sign). They’ll follow up with tests, including imaging of your gallbladder and bile ducts and blood tests to look for additional clues.
Tests to diagnose cholecystitis may include:
All of the causes of cholecystitis require treatment. It’s possible that a gallstone blocking your gallbladder or bile duct could become unstuck on its own, causing your symptoms to go away. But it’s not worth waiting for this to happen — the pain and the risk are too great. If it did happen, it probably wouldn’t be the end of your troubles. The same gallstone or another gallstone could get stuck again.
Cholecystitis is treated immediately in the hospital. Treatment begins with supportive care, including:
Advertisement
The definitive treatment for cholecystitis is surgery to remove your gallbladder. Most causes of cholecystitis, including gallstones, originate in your gallbladder itself. In rare cases, surgery might not be necessary if your cholecystitis was caused by something that’s separately treatable, like an infection unrelated to gallstones. You may also need to delay or forego surgery based on other health conditions.
If you’re delaying or foregoing surgery, you might have:
Even if your present episode of cholecystitis is over — the gallstone that was stuck is no longer stuck, or the symptoms that brought you to the hospital have passed — both chronic and acute cholecystitis are bound to recur. Gallstones that have caused acute cholecystitis once are likely to do so again. Repeat episodes of acute cholecystitis can lead to chronic cholecystitis, and both can do cumulative damage.
To prevent the effects of repeat episodes of gallbladder inflammation, healthcare providers recommend surgery to remove your gallbladder (cholecystectomy). This is a common, minor procedure with minimal side effects. Most people can have it done by minimally invasive laparoscopic surgery. A laparoscopic cholecystectomy requires only a few small incisions. More complicated cases may require open surgery.
Your biliary and digestive systems can function well without your gallbladder. Your gallbladder is mainly a storage place for the bile your liver makes. When a surgeon removes your gallbladder, they redirect your bile ducts to send bile directly from your liver to your small intestine. Your body will take a few weeks to months to adapt to this change. You might have temporary symptoms during this time, like:
You’ll need treatment in the hospital for cholecystitis, regardless of the type or cause. The hospital can provide immediate pain relief while they look for the cause. It’s usually gallstones, though not always. In most cases, healthcare providers recommend definitive treatment with surgery. Most people have excellent outcomes. Cholecystitis that goes untreated may lead to dangerous complications.
Severe abdominal pain always deserves medical attention. If it has the hallmarks of gallbladder pain — located in the upper right side of your abdomen, sudden and severe, and accompanied by nausea — you might want to head straight to the ER.
Your gallbladder is small, but when it’s stressed, your whole biliary system might be endangered. Cholecystitis symptoms may pass, but its causes will remain. Symptoms are likely to return, and cholecystitis will continue to harm your gallbladder until you get the treatment you need.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
