Diabetes is a common condition that affects people of all ages. There are several forms of diabetes. Type 2 is the most common. A combination of treatment strategies can help you manage the condition to live a healthy life and prevent complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video playlist content: This video playlist is available to watch online.
View video playlist online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_4ng8o4h9/flavorId/1_5f3sgelj/format/applehttp/protocol/https/a.mp4)
Learn about the early signs of diabetes.
Diabetes is a condition that happens when your blood sugar (glucose) is too high. It develops when your pancreas doesn’t make enough insulin or any at all, or when your body isn’t responding to the effects of insulin properly. Diabetes affects people of all ages. Most forms of diabetes are chronic (lifelong), and all forms are manageable with medications and/or lifestyle changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Glucose (sugar) mainly comes from carbohydrates in your food and drinks. It’s your body’s go-to source of energy. Your blood carries glucose to all your body’s cells to use for energy.
When glucose is in your bloodstream, it needs help — a “key” — to reach its final destination. This key is insulin (a hormone). If your pancreas isn’t making enough insulin or your body isn’t using it properly, glucose builds up in your bloodstream, causing high blood sugar (hyperglycemia).
Over time, having consistently high blood glucose can cause health problems, such as heart disease, nerve damage and eye issues.
The technical name for diabetes is diabetes mellitus. Another condition shares the term “diabetes” — diabetes insipidus — but they’re distinct. They share the name “diabetes” because they both cause increased thirst and frequent urination. Diabetes insipidus is much rarer than diabetes mellitus.
There are several types of diabetes. The most common forms include:
Advertisement
Other types of diabetes include:
Diabetes is common. Approximately 37.3 million people in the United States have diabetes, which is about 11% of the population. Type 2 diabetes is the most common form, representing 90% to 95% of all diabetes cases.
About 537 million adults across the world have diabetes. Experts predict this number will rise to 643 million by 2030 and 783 million by 2045.
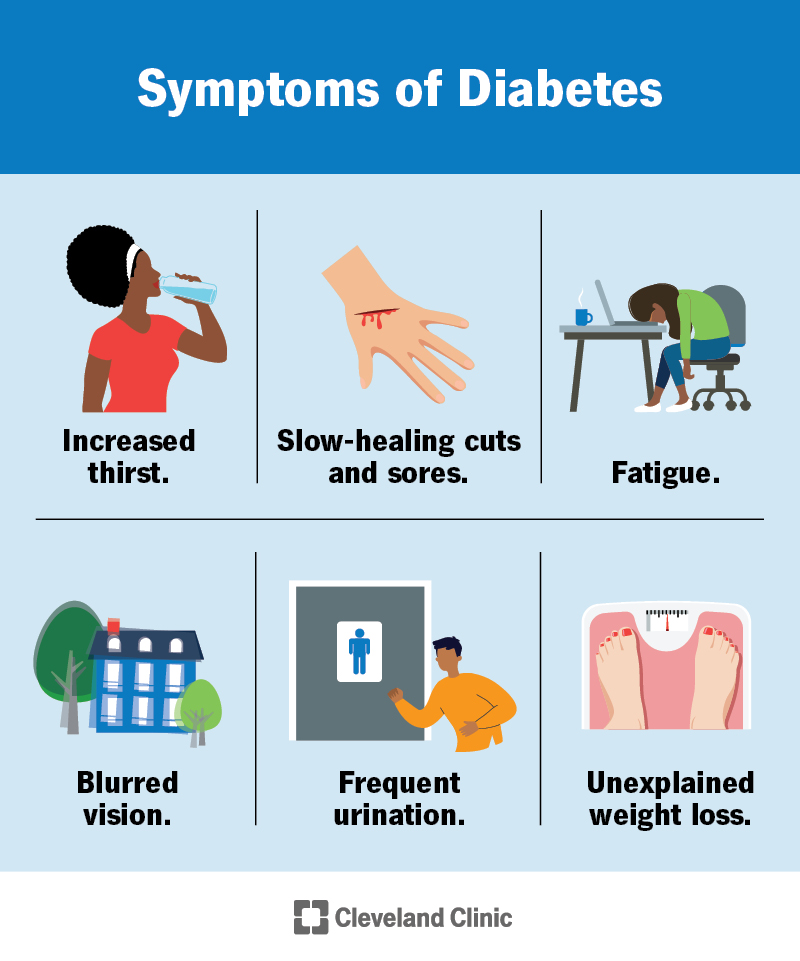
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/7104-diabetes-symptoms)
Symptoms of diabetes include:
It’s important to talk to your healthcare provider if you or your child has these symptoms.
Additional details about symptoms per type of diabetes include:
Advertisement
Too much glucose circulating in your bloodstream causes diabetes, regardless of the type. However, the reason why your blood glucose levels are high differs depending on the type of diabetes.
Causes of diabetes include:
Advertisement
Long-term use of certain medications can also lead to Type 2 diabetes, including HIV/AIDS medications and corticosteroids.
Diabetes can lead to acute (sudden and severe) and long-term complications — mainly due to extreme or prolonged high blood sugar levels.
Acute diabetes complications that can be life-threatening include:
Advertisement
Blood glucose levels that remain high for too long can damage your body’s tissues and organs. This is mainly due to damage to your blood vessels and nerves, which support your body’s tissues.
Cardiovascular (heart and blood vessel) issues are the most common type of long-term diabetes complication. They include:
Other diabetes complications include:
Living with diabetes can also affect your mental health. People with diabetes are two to three times more likely to have depression than people without diabetes.
Healthcare providers diagnose diabetes by checking your glucose level in a blood test. Three tests can measure your blood glucose level:
To screen for and diagnose gestational diabetes, providers order an oral glucose tolerance test.
The following test results typically indicate if you don’t have diabetes, have prediabetes or have diabetes. These values may vary slightly. In addition, healthcare providers rely on more than one test to diagnose diabetes.
| Type of test | In-range (mg/dL) | Prediabetes (mg/dL) | Diabetes (mg/L) |
|---|---|---|---|
| Fasting blood glucose test | Less than 100. | 100 to 125. | 126 or higher. |
| Random blood glucose test | N/A. | N/A. | 200 or higher (with classic symptoms of hyperglycemia or hyperglycemic crisis). |
| A1c | Less than 5.7%. | 5.7% to 6.4%. | 6.5% or higher. |
| Type of test | |||
| Fasting blood glucose test | |||
| In-range (mg/dL) | |||
| Less than 100. | |||
| Prediabetes (mg/dL) | |||
| 100 to 125. | |||
| Diabetes (mg/L) | |||
| 126 or higher. | |||
| Random blood glucose test | |||
| In-range (mg/dL) | |||
| N/A. | |||
| Prediabetes (mg/dL) | |||
| N/A. | |||
| Diabetes (mg/L) | |||
| 200 or higher (with classic symptoms of hyperglycemia or hyperglycemic crisis). | |||
| A1c | |||
| In-range (mg/dL) | |||
| Less than 5.7%. | |||
| Prediabetes (mg/dL) | |||
| 5.7% to 6.4%. | |||
| Diabetes (mg/L) | |||
| 6.5% or higher. |
Diabetes is a complex condition, so its management involves several strategies. In addition, diabetes affects everyone differently, so management plans are highly individualized.
The four main aspects of managing diabetes include:
Due to the increased risk for heart disease, it’s also important to maintain a healthy:
The prognosis (outlook) for diabetes varies greatly depending on several factors, including:
Chronic high blood sugar can cause severe complications, which are usually irreversible. Several studies have shown that untreated chronic high blood sugar shortens your lifespan and worsens your quality of life.
In the United States, diabetes is the eighth leading cause of death. A large number of people with diabetes will die from a heart attack or stroke.
However, it’s important to know that you can live a healthy life with diabetes. The following are key to a better prognosis:
Studies show that people with diabetes may be able to reduce their risk of complications by consistently keeping their A1c levels below 7%.
You can’t prevent autoimmune and genetic forms of diabetes. But there are some steps you can take to lower your risk for developing prediabetes, Type 2 diabetes and gestational diabetes, including:
It’s important to note that there are some diabetes risk factors you can’t change, such as your genetics/family history, age and race. Know that Type 2 diabetes is a complex condition that involves many contributing factors.
If you haven’t been diagnosed with diabetes, you should see a healthcare provider if you have any symptoms of diabetes, such as increased thirst and frequent urination.
If you have diabetes, you should see your provider who helps you manage diabetes (such as an endocrinologist) regularly.
Being diagnosed with diabetes is a life-changing event, but it doesn’t mean you can’t live a happy and healthy life. Managing diabetes involves consistent care and diligence. While it’ll likely be very overwhelming at first, over time you’ll get a better grasp on managing the condition and being in tune with your body.
Be sure to see your healthcare provider(s) regularly. Managing diabetes involves a team effort — you’ll want medical professionals, friends and family on your side. Don’t be afraid to reach out to them if you need help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you’ve been living with diabetes for years or you’re newly diagnosed, you want experts you can trust. Our team at Cleveland Clinic is here to help.
