If you have hemochromatosis, your body absorbs and retains too much iron. With no natural way to get rid of it, your body stores it in your tissues and organs. Too much iron can become toxic and damage your organs, especially your heart, liver and pancreas. Treatment can help reduce your iron levels to prevent these complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
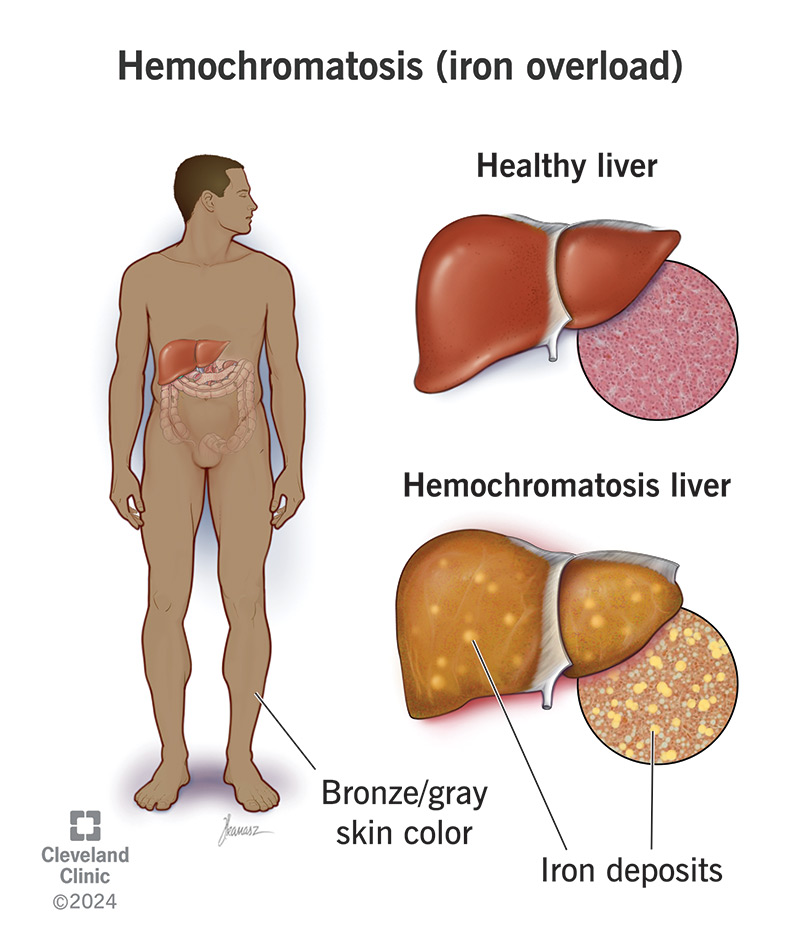
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14971-hemochromatosis-iron-overload.jpg)
Hemochromatosis (HEE-mow-KROW-muh-TOW-sis) is a condition in which your body absorbs and retains too much iron. It’s also called iron overload. Your organs store the excess iron, which damages them over time. It especially damages your heart, liver and pancreas. Iron overload can become life-threatening without treatment. But fortunately, it is treatable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Common symptoms of hemochromatosis (iron overload) include:
These symptoms happen when iron builds up to levels that start to affect your organs. Although hemochromatosis usually starts at birth, it takes a long time for iron to build up. Most people don’t develop symptoms until their 40s or 50s. If you have a milder form of hemochromatosis, you might not ever notice it. Or symptoms might appear much later in life and resemble normal signs of aging.
Most people with hemochromatosis inherit it from their parents. This is called hereditary hemochromatosis, or primary hemochromatosis. The cause is an altered gene that they pass on to you. It takes two copies of the altered gene — one from each parent — for you to develop hemochromatosis. If your parents each have only one copy, they likely won’t have the condition or know about the gene.
Changes in the HFE gene usually cause hereditary hemochromatosis. The two most common variants are C282Y and H63D. A less common form of the condition, called juvenile hemochromatosis, comes from changes in the HJV or HAMP genes. These changes cause iron to build up much more quickly, so symptoms appear sooner. Juvenile hemochromatosis typically appears between the ages of 15 and 30.
Advertisement
You can also develop hemochromatosis secondary to another medical condition or treatment. For example, if you have anemia, you can develop iron overload from frequent blood transfusions. If you have advanced liver disease, your liver may not be able to process iron properly, causing it to build up. Rarely, a developing fetus with preexisting liver disease can develop neonatal hemochromatosis.
Hereditary hemochromatosis is more common in white people with ancestors from Northern Europe. It’s less common in people of African American, Hispanic, Asian or Native American descent. You can find out if you have one or more copies of the altered HFE gene through genetic testing. If you’re planning a family, you and your partner may want to find out if you each carry one of the genes.
Risk factors for secondary hemochromatosis include:
Your body needs iron, but too much becomes toxic. Your body doesn’t have a built-in way to get rid of excess iron. So, it stashes it away in your tissues. As iron builds up, you may start to see it in your skin and feel it in your joints. It may also start to cause problems with your organs and glands, including your:
Iron overload affects your heart, liver and pancreas the most. It can lead to serious complications like:
To find out if you have hemochromatosis, your healthcare provider will start by asking some questions. For example, they might ask:
They’ll perform a physical exam to look for signs and symptoms of iron overload.
Other tests might include:
Hemochromatosis treatment includes changes to your eating habits and other methods to help reduce iron levels in your body. These treatments can help prevent or delay further damage to your organs.
Advertisement
If another condition caused your hemochromatosis, you may need separate treatment for that condition. You may also need separate treatment for problems caused by hemochromatosis.
The outlook for hemochromatosis depends on how soon you get a diagnosis and treatment. If hemochromatosis progresses for a long time without treatment, it can do real damage to your organs. Some damage may be irreversible. But with timely recognition and treatment, hemochromatosis is a manageable disease. You can live a typical, healthy life, and may even be able to reverse organ damage.
Advertisement
If you remember Popeye, or having to eat spinach as a kid, you know that getting enough iron is a health goal. So, you might be surprised to learn that you can actually get too much. It usually takes a glitch in your genetic code for this to happen — and it typically takes decades. But iron overload can do real damage if it goes untreated. Regular checkups and blood tests can help catch it before that happens.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
