Liver failure means that your liver is shutting down and failing to perform its essential functions. This can happen rapidly or gradually. Symptoms of liver failure can affect almost every major body system. When liver failure is final, it can be fatal without a liver transplant.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your liver is one of your essential organs, one you can’t live without. It performs hundreds of important bodily functions. When your liver fails to keep up with its many jobs, your overall health will fail, too. This is liver failure. It means that your liver is no longer able to function adequately for your body’s needs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Liver failure is a process, which may be fast or slow. Acute liver failure happens rapidly, within days or weeks. Chronic liver failure, the more common type, happens gradually, over months or years. As your liver begins to lose its functionality, you’ll notice more and more the symptoms of liver failure.
Acute liver failure happens suddenly, when something overwhelms your liver’s capacity to cope. It’s usually a large toxic load, like poisoning. Sometimes, it’s a severe viral infection. In acute liver failure, your liver rapidly begins to shut down, causing immediate symptoms. This is a medical emergency.
Chronic liver failure is the end stage of chronic liver disease. It happens when something has been damaging your liver for a long time, and the damage has finally become irreversible. Chronic liver failure follows cirrhosis, severe scarring of your liver tissues. Scar tissue prevents your liver from functioning.
Most medical authorities define chronic liver failure as the end stage of chronic liver disease. Liver disease can progress through several stages. However, it’s important to remember that these stages aren’t discreet from each other. Someone with fibrosis (scarring) can still have inflammation (hepatitis):
Advertisement
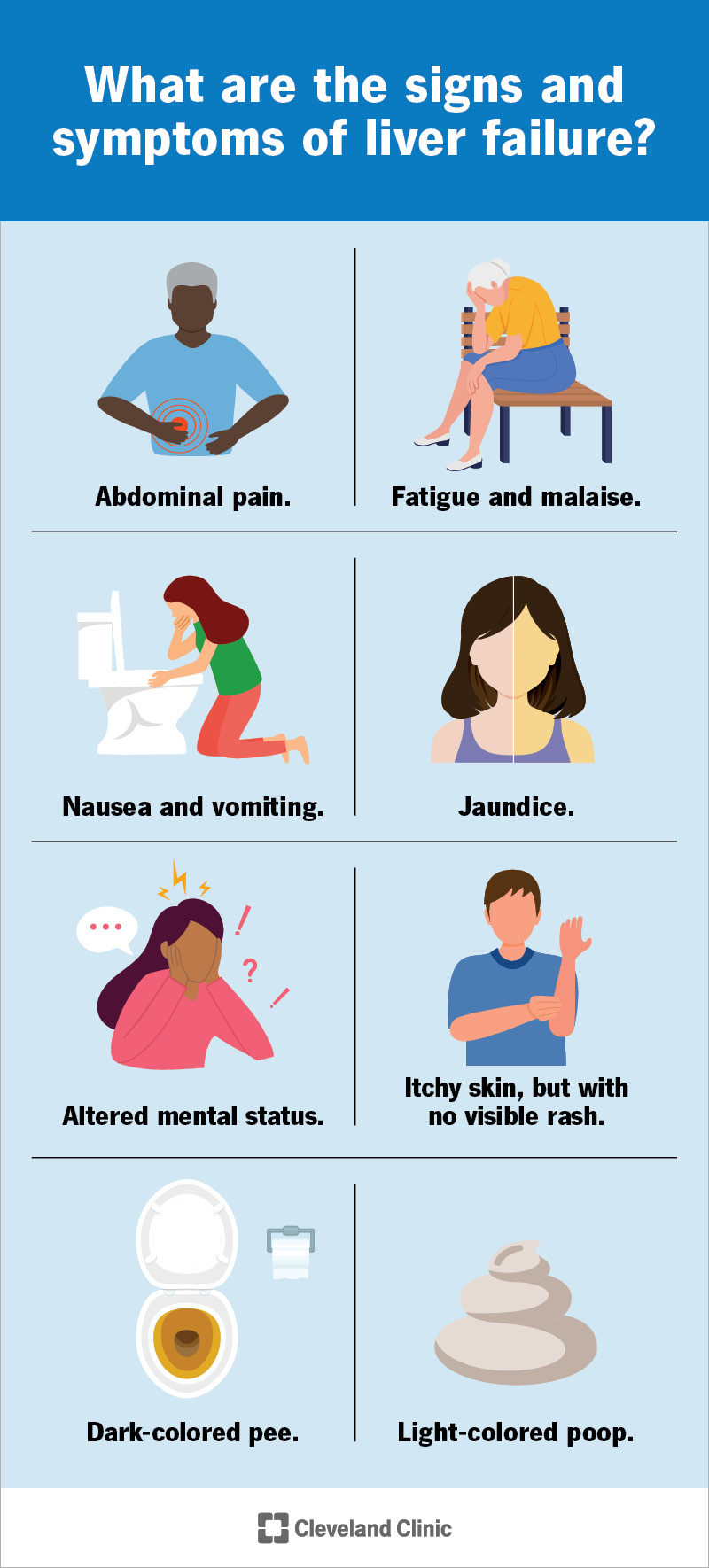
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17819-liver-failure)
You may notice different signs and symptoms of liver failure based on how advanced it is and which complications have begun to occur. The first symptoms of chronic or acute liver failure may include:
Symptoms more specific to liver disease may appear after these. The first warning signs of a damaged liver that’s starting to fail are signs of bile and other toxins building up in your blood. These may include:
Chronic liver failure may also show up in subtler ways, like:
Other serious signs of liver failure include:
Advertisement
Liver failure can affect your sex hormones, leading to an imbalance of estrogen and testosterone. This may cause different symptoms in females or males. Menstrual cycles may become irregular or stop. Testicles may shrink and breast tissue may enlarge in males.
Liver failure will cause toxins to flood your bloodstream, which feels pretty terrible. When your liver can’t filter toxins from your blood anymore, you’ll feel nauseous, tired and weak. Toxins may also infiltrate your brain, causing confusion, irritability, anxiety, drowsiness or motor dysfunction.
Acute and chronic liver failure happen in different ways, but they’re both due to overwhelming stress on your liver. Some of the same toxins and diseases can stress your liver all at once or gradually over time, depending on how severe they are. Other causes of liver failure only happen suddenly or gradually.
Acute liver failure usually occurs in people with no prior history of liver disease. It happens when something overwhelmingly injures your liver. This might be an overwhelming toxic load that your liver encounters as it’s filtering your blood. It can also be an acute infection that attacks your liver directly.
Causes include:
Advertisement
Chronic liver failure is the result of cirrhosis. The scarring process prevents blood and oxygen from nourishing your liver tissues, causing cell death. As liver cells die, your liver functions less and less. Cirrhosis is the result of long-term hepatitis, which many chronic liver diseases can cause.
These include:
Advertisement
Your liver performs many important functions, supporting many different body systems. When these begin to fail, you’ll notice the effects throughout your body. For example, you might notice:
In addition to these effects, many people with chronic liver failure already have complications from cirrhosis. Cirrhosis causes the side effect of portal hypertension, which in turn can cause:
Complications of portal hypertension are the most frequent causes of hospitalization and death in people with chronic liver failure, and many of these can begin before chronic liver failure starts.
If you have signs and symptoms of liver failure, a healthcare provider will run tests to confirm it. These may include:
Treatment for liver failure involves:
Supportive care to help stabilize your condition might include:
Treatments to address the causes of liver failure might include:
Your healthcare team will monitor your condition and manage complications as they arise. They’ll recommend you for a liver transplant if they judge that your prognosis (outlook) is worse without one. Providers have clinical scoring systems for judging your prognosis and whether to recommend a liver transplant.
There’s always some risk in having an organ transplant, especially when you’re not in good health for the procedure. But when the process of organ failure is near the end stage, that risk may save your life. If your healthcare team recommends you for a liver transplant, you’ll join a national waiting list.
You can recover from acute liver failure, though this is difficult to predict. Chronic liver failure isn’t reversible, but it’s a gradual process, and sometimes you can slow it down. In general, your prognosis is better if there’s a specific treatment available for your condition and if you begin treatment sooner.
Acute liver failure can be fatal in days, weeks or months. Chronic liver failure can last for months to years. How long the process takes depends on many factors, including:
Healthcare providers consider all these factors when placing you on the waiting list for a liver transplant. They use scoring systems to determine the urgency of your need and your place on the list.
Acute liver failure is rare, but it only takes one unfortunate event to trigger it. You can help to prevent this by following some common-sense safety guidelines:
Preventing chronic failure is more about general lifestyle choices. Chronic liver disease takes a long time to progress to liver failure. If you develop liver disease, you can slow, stop or even reverse the process by making changes earlier on. For example:
Acute liver failure is an emergency. If you think you might have it, you need to go straight to the hospital. Chronic liver failure isn’t an emergency, but it’s equally serious. If you’ve been diagnosed with chronic liver failure, you can help support your liver by maintaining a healthy diet and lifestyle.
Your liver is the largest organ in your body, a sign of the outsized role it plays in your life. When your liver begins to fail, you’ll feel it in all sorts of ways. Fortunately, your liver doesn’t fail all at once. Whether you have acute or chronic liver failure, earlier recognition and treatment can often make a difference in extending the life of your liver. At the end stage, a liver transplant could save your life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Hearing you need a liver transplant can be life-changing. But Cleveland Clinic is here for you with expert care that’s focused on you every step of the way.
