Hepatic encephalopathy, also called portosystemic encephalopathy, happens when your liver isn’t filtering toxins as it should. These toxins build up in your blood and affect your brain, causing confusion, disorientation and other changes. Hepatic encephalopathy can get better with treatment, but it can be life-threatening without.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hepatic encephalopathy is brain dysfunction caused by liver dysfunction. “Encephalopathy” is brain dysfunction, and “hepatic” means liver-related.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Encephalopathy affects your central nervous system and how you think, feel and act. Symptoms can range from confusion and disorientation to erratic behavior and personality changes. It can get better with treatment, but it can be life-threatening without.
Hepatic encephalopathy is caused by neurotoxins in your blood — substances that are toxic to your brain and nervous system. Normally, your liver filters these toxins from your blood. But if your liver isn’t performing this function as usual, the neurotoxins continue to circulate. Eventually, they enter and affect your brain. This usually happens in advanced liver disease, when liver functions begin to fail.
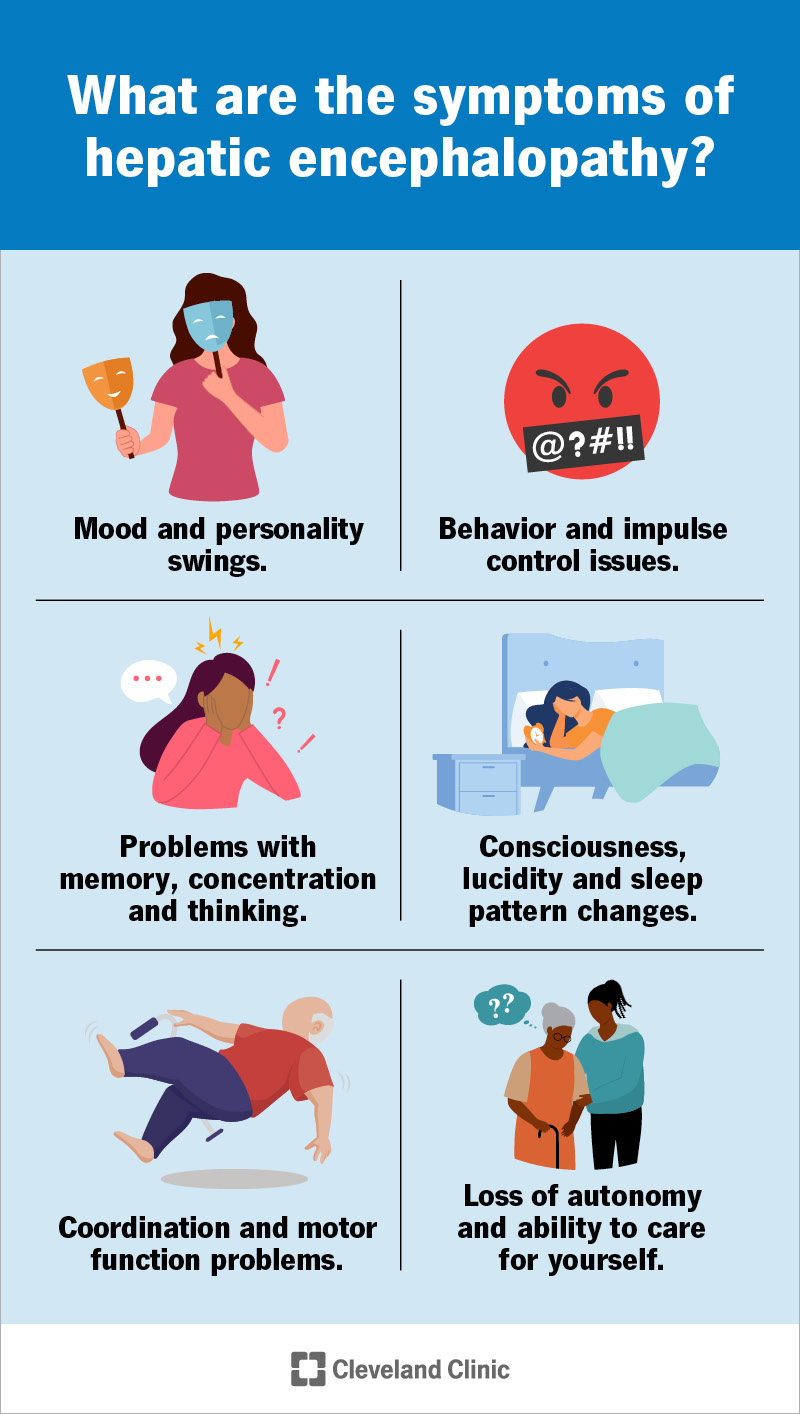
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21220-hepatic-encephalopathy.jpg)
Hepatic encephalopathy can show up in a wide variety of ways. Not everyone will have every symptom. It can affect your:
Symptoms may occur suddenly or come on gradually, and they may be steady and lasting or come and go in episodes. They may get better or worse, depending on your overall health condition. Hepatic encephalopathy can be mild to severe, and symptoms may be barely noticeable to striking. Healthcare providers sometimes group symptoms by their severity as a way of grading, or staging, the disease.
Advertisement
The West Haven Criteria is the most common grading system healthcare providers use for hepatic encephalopathy. It grades symptoms on a scale of 0 to 4. Stages 0 to 1 are sometimes called minimal hepatic encephalopathy (MHE) or covert HE. Symptoms in these stages may not be outwardly noticeable. Stages 2 to 4, also called overt hepatic encephalopathy, feature more obvious symptoms.
Possible symptoms by grade include:
Grade 0
Grade 1
Grade 2
Grade 3
Grade 4
Any symptoms of overt hepatic encephalopathy are serious. It’s important to treat the condition as soon as possible to prevent it from worsening or causing permanent damage. Severe hepatic encephalopathy can advance to coma or even death. If you see Grade 3 symptoms, like severe drowsiness, confusion or amnesia, disorientation in space and time, or involuntary movements, treatment is especially urgent.
Hepatic encephalopathy happens when your liver doesn’t filter neurotoxins out of your blood as it normally would. This might be because your liver has temporarily or permanently lost some of its function (liver failure). It might also be because the blood that normally passes through your liver for filtering isn’t passing through it anymore (portosystemic shunt). Sometimes, both things are happening.
The blood your liver filters comes directly from your digestive system, via your portal vein (portal circulation). This blood carries waste products left over from the digestive process, including ammonia and others. Your liver filters them out before sending the blood back out to your body (systemic circulation). If it doesn’t, they build up in your blood and eventually damage your brain tissues.
Advertisement
Healthcare providers define different types of hepatic encephalopathy based on the original cause.
Type A is caused by acute liver failure. This is a sudden loss of liver function due to a sudden, severe liver injury. Viral infections, autoimmune liver disease and acetaminophen poisoning are common causes. Cerebral edema, swelling in your brain, is a frequent side effect that may contribute to the effects of hepatic encephalopathy. Acute liver failure is an emergency and some cases may require a liver transplant.
Type B is caused by a portosystemic shunt. A shunt is when blood flow bypasses its normal route through a new, abnormal passageway. A portosystemic shunt is when your portal circulation bypasses your liver on its way to your systemic circulation. Your body may create a shunt if there's a blockage in the normal pathway. Sometimes, a healthcare provider creates one for you for the same reason (transjugular intrahepatic portosystemic shunt, or TIPS). Hepatic encephalopathy is a possible complication in both cases.
Type C is caused by chronic liver failure. Chronic liver failure is the gradual decline of liver function from chronic liver disease. It’s not reversible. Chronic hepatitis C, chronic alcohol use disorder and metabolic dysfunction-associated steatotic liver disease (MASLD) are common causes. At this stage, extensive scarring in your liver (cirrhosis) may prevent it from working right. Scarring may also compress your portal vein (portal hypertension,) triggering a portosystemic shunt. (This would still be Type C.)
Advertisement
Chronic liver disease works slowly, and you can live with it for a long time before it really begins to affect you. Your body compensates for it until it can’t, which is when liver failure sets in. Healthcare providers have noticed that it’s often a secondary health problem or stress factor that tips the scales enough to trigger hepatic encephalopathy in people with chronic liver disease. These triggers might include:
A hepatologist or gastroenterologist usually diagnoses hepatic encephalopathy. Diagnosis involves:
You might have:
Advertisement
Treatment for hepatic encephalopathy includes:
Treatment for the first two will vary, depending on the nature of the conditions affecting you.
For liver failure, whether acute or chronic, there’s often no direct treatment. Healthcare providers try to reduce any stress factors affecting your liver and offer supportive care to address symptoms and complications. If they deem it necessary, they’ll put you on a waiting list for a liver transplant. For a portosystemic shunt, providers may use interventional radiology techniques to redirect your blood flow.
Healthcare providers target the neurotoxins in your blood at their source, which is in your gut. As many of these toxins are byproducts of certain bacteria in your gut, providers may prescribe antibiotics to reduce the number of these bacteria. They combine these with an osmotic laxative to speed up the passage of food waste through your gut and reduce how much it can absorb into your bloodstream.
The most common medications healthcare providers prescribe are:
Supplemental medications include:
In the case of acute liver failure, which is an emergency, hemodialysis may be helpful for treating Type A hepatic encephalopathy. This is a way of filtering toxins from your blood, using a dialysis machine.
With timely treatment, recovery is possible, but how much your brain recovers can vary. In general, if the causes affecting you are brief, and if they’re relatively mild, you’re more likely to recover fully. If you have a permanent condition, you’ll need ongoing therapy to manage your neurotoxin levels. Even with treatment, chronic liver failure will continue, and hepatic encephalopathy could relapse or recur.
Hepatic encephalopathy is one factor affecting your life expectancy. The conditions causing it are others. Healthcare providers can’t predict life expectancy in every scenario. For example, if you have hepatic encephalopathy with acute liver failure, this is an emergency that you may or may not survive. Having hepatic encephalopathy makes things more serious. But if you do survive it, your life expectancy afterward might be normal.
On the other hand, if you have chronic liver failure, this is eventually fatal regardless of hepatic encephalopathy. Having hepatic encephalopathy makes things more serious. At this stage, most models predict a life expectancy of up to two years. Roughly half of people with both conditions live a full year after diagnosis, and half of those live another full year. But this changes if you have a liver transplant.
If you have persistent or recurrent hepatic encephalopathy, taking care of yourself is more important than ever. You might also need more help than ever to do it. You’ll do better in the long run if you can:
Whether you’ve had a long history of liver disease or no history of it at all, hepatic encephalopathy can sneak up on you. It’s often others around you who are the first to notice subtle changes. As acute liver disease happens suddenly, and as chronic liver disease can go on for a long time without causing symptoms, sometimes, hepatic encephalopathy is the first real red flag of liver failure to appear.
This diagnosis can feel overwhelming, for both you and your loved ones. Even if you’ve had other physical symptoms, altered mental status is another thing. It can feel like you’re losing yourself, or your loved ones are losing you. But don’t lose hope: Noticing and seeking treatment is half the battle, and hepatic encephalopathy can get better. This is the time to lean on your personal support and professional healthcare teams.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic providers compassionately diagnose and treat all liver diseases using advanced therapies backed by the latest research.
