Parenteral nutrition is a way for you to receive nutrients by bypassing your digestive system. People who can’t use their digestive systems because of a condition can temporarily or permanently receive nutrition intravenously, through an IV catheter. Parenteral nutrition can be supplementary (partial) or complete (total parenteral nutrition).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
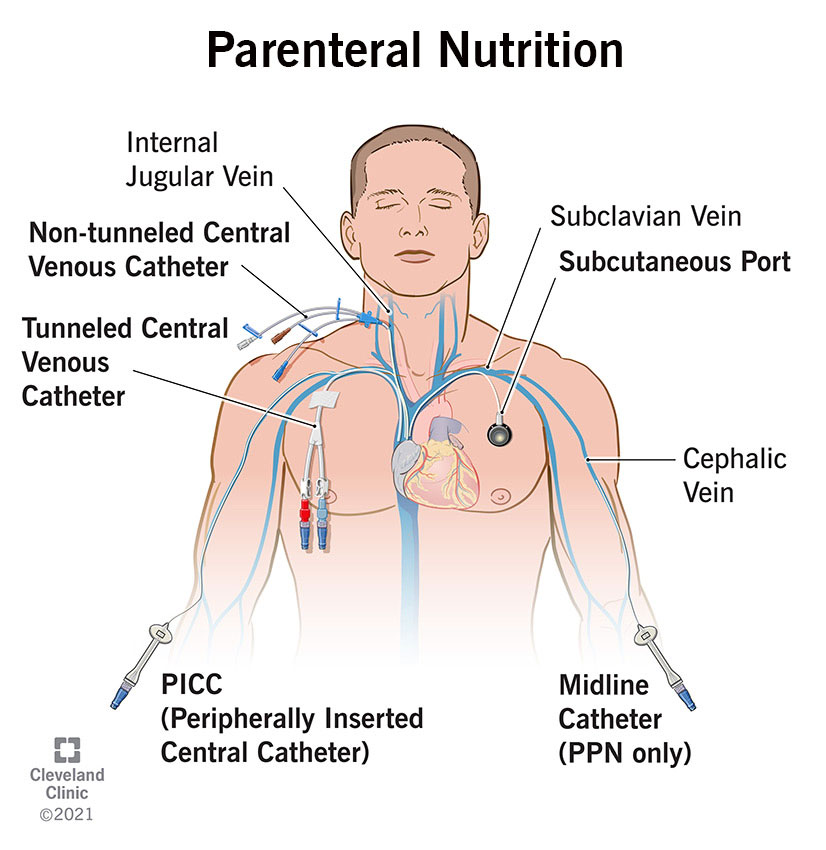
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22802-parenteral-nutrition)
Parenteral nutrition means feeding intravenously (through a vein). "Parenteral" means "outside of the digestive tract." Whereas enteral nutrition is delivered through a tube to your stomach or the small intestine, parenteral nutrition bypasses your entire digestive system, from mouth to anus. Certain medical conditions may require parenteral nutrition for a short or longer time. Some people need it to supplement their diet, and some people need to get all of their calories intravenously.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Parenteral nutrition can be partial or total.
Sometimes parenteral nutrition is classified by the type of vein that is used to deliver the nutrition.
Advertisement
Parenteral nutrition is a chemical formula with standard variations and can be customized to your specific nutritional requirements. It may include different amounts of any of the six essential nutrients that your body requires: water, carbohydrates, proteins, fats, vitamins and minerals. Even when you receive total parenteral nutrition, your formula will be tailored to you based on lab results. Parenteral nutrition is complete enough to replace mouth feeding for as long as necessary — even for life.
Partial parenteral nutrition is often given temporarily to people who need an immediate boost of calories before transitioning to a longer-term solution — either enteral feeding or gradually resuming mouth feeding. PPN is also commonly given to long-term hospital patients who tend to have general malnutrition for a variety of reasons.
You might need total parenteral nutrition if your digestive system isn’t functioning or if you have a gastrointestinal disease that requires you to give it complete rest. Some people might just need general nutrition therapy but might have medical reasons why enteral feeding won’t work for them.
Specific conditions that may require TPN include:
Your healthcare team will determine your nutritional needs based on your health history, BMI and lab test results. Guidelines recommend that doctors, nurses, nutritionists and pharmacists collaborate to design your formula. A specialist will prepare your formula in 24-hour doses. All doses must be refrigerated until the day they are used and can be stored for up to seven days. Refrigerated formulas should be taken out a few hours prior to use to adjust to room temperature.
Placing the IV catheter in your body will require two points of penetration through your skin. Your healthcare provider will offer you anesthesia to numb the pain and help you relax and carefully clean and sterilize the two points. They’ll begin by inserting a needle threaded with a guidewire through the skin into your vein. Then they’ll remove the needle, place the catheter tube over the guidewire and remove that. They might use a small ultrasound device to guide the placement of the catheter or an X-ray to confirm the correct placement afterward.
There are three types of catheters they might use:
Advertisement
If you have an external catheter, you or your healthcare provider will attach the external end to another tube that connects to the IV bag with your nutrition solution. If you have an internal catheter, you’ll attach the IV bag to a tube connected to a special needle (called a Huber needle) that inserts into the implanted port. The parenteral nutrition infusion takes about 10 to 12 hours to fully transfer from the IV bag into your body. You may choose to take it at night while you sleep.
Parenteral nutrition can be administered in a hospital, long-term care facility or at home. Healthcare providers administering parenteral nutrition are careful to maintain strict sterile standards to prevent infection. Anyone administering parenteral nutrition at home will receive thorough training in how to recognize signs of contamination or infection. You’ll also change the dressings at the incision sites at least once a week and change the tubing connecting the catheter to the infusion bag every day.
Healthcare providers will constantly monitor your fluid intake and output and periodically weigh and measure you. They will also take regular blood tests to make sure you have the right balance of essential nutrients and adjust your formula accordingly. Some of the things they will monitor include:
Advertisement
While parenteral nutrition can be used long-term if necessary, enteral feeding is better and oral feeding is ideal. Your healthcare team will want to transition you to one of these, or a combination of the two, as soon as your body allows, to avoid the long-term complications of parenteral feeding.
The transition is gradual, both because of your underlying gastrointestinal condition and because certain functions of the digestive tract can begin to atrophy when it hasn't been used for a while. Your healthcare team will probably start you on a clear liquid diet. If you tolerate that well, you’ll transition to a full liquid diet, and finally, solid food.
The primary advantage of parenteral nutrition is to give your gastrointestinal system a chance to heal from severe illness or surgery. For long-term hospital patients, especially geriatric patients who have trouble sustaining their nutritional needs through eating or with enteral nutrition, partial parenteral nutrition can provide an important boost to help their bodies manage their other difficulties. For people with permanently impaired gastrointestinal function, or for extremely premature and sick infants who haven’t yet developed the ability to feed normally, total parenteral nutrition can be life-saving.
Advertisement
Parenteral nutrition is considered less ideal than enteral feeding because of the higher risk of complications involved. The primary concerns are infection of the bloodstream from the IV catheter and atrophy of the digestive tract when it isn’t being used. There are other risks, however.
The most common complications include:
Other possible complications include:
After you have successfully weaned from parenteral nutrition, your healthcare team will continue to monitor your weight and nutrition levels for a while to make sure your oral nutrition and hydration are sufficient. If you had liver complications during parenteral nutrition, those higher enzyme levels may persist for years. However, with a healthful, nutritious diet, your long-term health outlook is good.
Parenteral nutrition is an extreme intervention, but someday you or your child may need it. Parenteral nutrition may sustain you or your child through a difficult interval in their or your health. If that interval is long, you may end up administering parenteral nutrition at home. It may start as an inconvenience, but will soon evolve into just another routine. During parenteral nutrition, your healthcare team will continue to monitor your nutritional needs and reactions with extreme care. When the time comes to wean from parenteral nutrition, they will help you return to ordinary eating with equal care.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
