With Budd-Chiari syndrome, the veins that carry blood away from your liver develop blockages or become too narrow. Causes include obstructions inside your blood vessels (like blood clots) and inflammation. Treatments help improve blood flow in your liver. They include blood thinners, minimally invasive procedures and surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
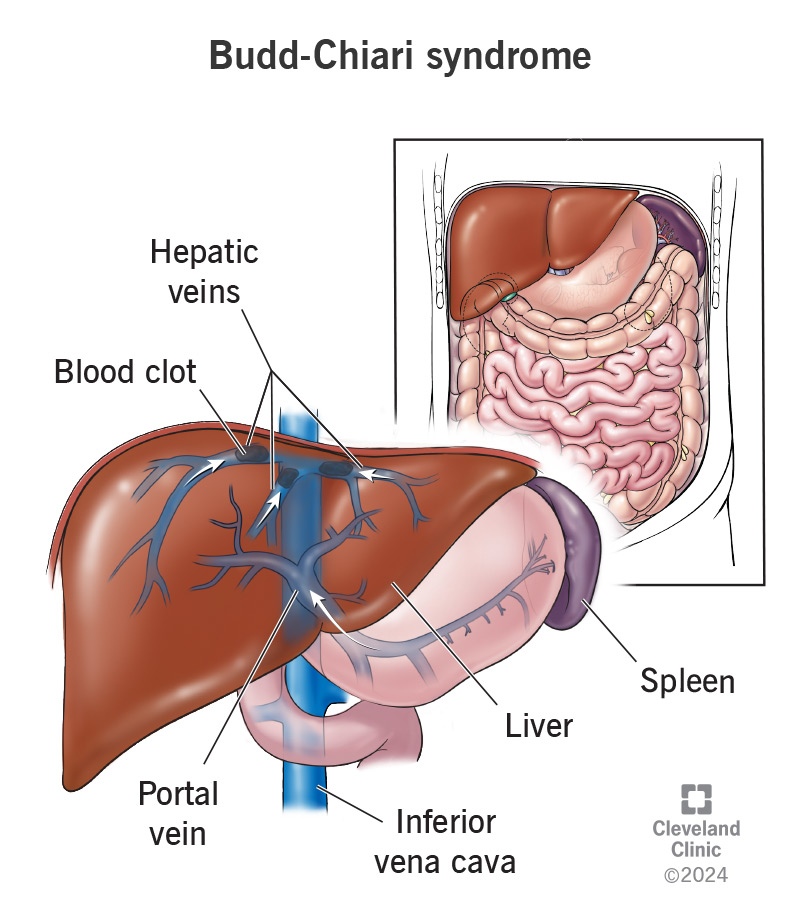
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21097-budd-chiari-syndrome.jpg)
Budd-Chiari syndrome involves narrowing or a blockage (obstruction) in one or more of the veins that drain your liver (hepatic veins). The narrowing can be from inflammation within your veins or pressure (compression) outside your veins. An obstruction may block all of a vein or only part of it. The obstruction can be from a blood clot, but not always.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Budd-Chiari can cause blood to back up into your liver, enlarging it. Your spleen may also enlarge.
Budd-Chiari syndrome may also cause other conditions, including:
Providers classify Budd-Chiari syndrome based on how long you’ve had it and the severity of your symptoms. Types include:
Budd-Chiari syndrome may be primary or secondary:
Advertisement
The signs and symptoms of Budd-Chiari syndrome include:
The timing of symptoms depends on the type of Budd-Chiari syndrome you have. People with acute forms typically notice symptoms more quickly than people with subacute or chronic Budd-Chiari syndrome. Researchers estimate that 15% to 20% of people with subacute and chronic forms don’t have symptoms.
Conditions and situations that lead to blood clots cause Budd-Chiari syndrome. These include:
One in five cases of Budd-Chiari syndrome is idiopathic. This means healthcare providers can’t determine a clear cause for the condition.
A healthcare provider can diagnose Budd-Chiari syndrome through a physical exam and tests. They’ll ask about your symptoms and look for signs of Budd-Chiari syndrome, like upper abdominal pain and swelling. They’ll arrange for blood tests to check your liver function and see if you’re at risk for blood clots. Up to 50% of people with Budd-Chiari syndrome have high liver enzyme levels.
Imaging tests can show if there’s narrowing or obstruction of your hepatic veins or IVC. These tests include:
Advertisement
Your provider (a radiologist or hepatologist) may order a liver biopsy to see if you have cirrhosis. A sample of your liver tissue will be sent to the pathology lab so a pathologist can examine it under a microscope.
Treatments for Budd-Chiari syndrome dissolve clots or improve narrowing in your hepatic veins or IVC to decrease swelling and scar formation in your liver. Whenever possible, treatments involve managing the underlying condition that caused you to develop clots. Also, managing complications, like portal hypertension (high blood pressure in your portal vein), is essential.
Your healthcare provider may prescribe blood thinners (anticoagulants), such as heparin or warfarin, to dissolve the blood clots.
You may need a procedure to help redirect blood flow and relieve pressure in your blood vessels. Procedures include:
Advertisement
You may need a liver transplant if other treatments haven’t helped or aren’t an option. For example, you’ll likely need a liver transplant if you have liver failure, cirrhosis of the liver, bleeding from varices or ascites that can’t be treated with medications.
Your prognosis depends on various factors, including how severe your condition is and your response to treatment. The outlook tends to be better if you don’t have:
Without treatment, most people with a completely blocked hepatic vein die of liver failure within three to five years. You can live longer with a liver transplant. Research shows people also usually live longer if their veins are only partially blocked or narrowed.
Your healthcare provider is your best resource for explaining your prognosis (likely outcomes) based on your specific diagnosis and health.
Follow your healthcare provider’s instructions on what follow-up care you’ll need to monitor your liver. You may need:
Advertisement
Questions to ask include:
Prompt treatment for Budd-Chiari syndrome is essential. Whether through medications or a procedure like TIPS, your healthcare provider will need to address the condition, so your hepatic veins can drain your liver. In severe cases, you may need a liver transplant. Regardless of the treatment type, it’s essential to follow your healthcare provider’s guidance on follow-up care. They can advise you on what steps to take to treat the underlying condition and reduce your risk of complications.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a disease that’s affecting your liver, you want expert advice and care. At Cleveland Clinic, we’ll create a treatment plan that’s right for you.
