An embolism is an obstruction or blockage in a blood vessel. Most often, it starts as a blood clot from elsewhere that breaks off and travels through your bloodstream. When a blood clot or another substance becomes an obstacle, it’s an embolism. This keeps blood from moving through a blood vessel and reaching tissues or organs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
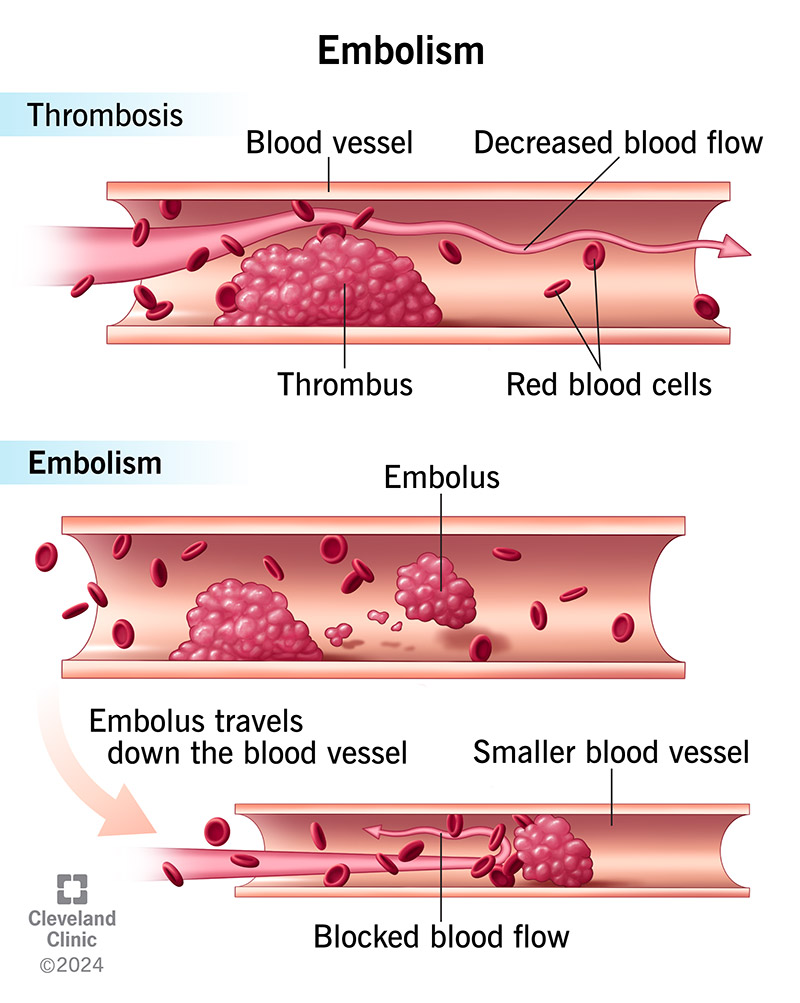
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/thrombosis-and-embolism)
An embolism is a blockage in your blood vessel — usually from a blood clot that started elsewhere. Other substances that can move around your body can travel away from where they started and block a blood vessel, too.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some blood vessels may be more likely to have a blockage just because their size and shape make it easier for things to get stuck. A blockage may be more likely to happen when blood vessels become smaller, like where one artery branches off another one, or where plaque buildup (atherosclerosis) makes an artery narrow.
Emboli can happen in your brain, lungs, kidneys or spleen, to name a few locations. Your lungs are the most common location for an embolism. A blood clot that travels from your veins to your lungs is called a pulmonary embolism (PE).
Embolisms differ by the substance creating the blockage.
Types of embolism include:
Embolisms are common. About 900,000 people a year get a venous thromboembolism diagnosis in the U.S.
Pulmonary embolisms are the world’s third leading cause of cardiovascular (heart and blood vessel) death. (Strokes and heart attacks are the top two causes.)
Venous thromboembolism is more common than arterial thromboembolism.
When you have an embolism in an artery, it blocks blood that’s trying to get through. Blood carries oxygen that all your cells need. If blood can’t get through, oxygen can’t either. This lack of oxygen causes an “infarct” and damages the organ that needs oxygen. This can cause pain from the organ that has an infarct. In some cases, this lack of oxygen can be fatal.
Advertisement
Small emboli may break off of a thrombus in a vein and travel back to the right side of your heart, which pumps blood into your lungs. These emboli (called pulmonary emboli) get stuck in the small pulmonary vessels of your lungs and cause a lung infarct. In rare cases, large pulmonary emboli can even block the normal flow of blood from the right heart into your lungs.
Embolism symptoms vary by the type and location of the blockage. Some people don’t have symptoms at all. Symptoms may include:
Most emboli are pulmonary emboli that originate from blood clots that start in the leg veins (deep vein thrombosis). Sometimes, deep vein thrombosis in the arm veins can also lead to pulmonary embolism.
Other embolism causes include:
The risk factors for the most common type of embolism (from a blood clot) include:
The complications of embolisms vary by where they happen. An embolism can lead to:
A healthcare provider can do a physical exam to check for signs of an embolism. Depending on the type of embolism, they may see something on your skin or see that you’re having trouble breathing, for example. If they suspect an embolism, they can order tests.
Depending on the type of embolism, a provider can diagnose it with:
Advertisement
The goal of embolism treatment is to restore blood flow by removing the blockage from your blood vessel. Medication is usually the first-choice treatment.
Embolism treatments may include:
In serious cases, people with an embolism may need additional life support, including CPR, ECMO and a machine that helps them breathe.
Anticoagulants and thrombolytics carry a risk of bleeding. The risks of clot removal (embolectomy) include:
Some people with embolisms may not have symptoms, while others have severe ones. Your outlook depends on several factors, like the size, severity and location of the embolism.
Embolisms can be life-threatening. Prompt diagnosis and treatment may improve your outcome.
Yes, you can prevent some embolisms. If you’re at risk of an embolism, a provider may recommend:
Advertisement
You may need rehabilitation to help you recover after an embolism. This is because you may have damage to your brain or lungs, for example. This damage happens because the embolism kept oxygen from reaching the affected organ or area.
You should get immediate care if you’re having symptoms of an embolism.
After having an embolism, you’ll need follow-up appointments with your provider. They’ll want to make sure you’re taking your anticoagulants as instructed and they’ll check to see that your bleeding risk hasn’t changed.
Questions to ask your healthcare provider may include:
It’s understandable to be concerned about embolisms, as they can be life-threatening. That’s why getting prompt treatment is so important. If you have symptoms of an embolism, get medical attention quickly. After treatment, turn to your family or friends for support during your recovery. Speak with a counselor if you feel worried about having another embolism.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
