Pulmonary edema is a buildup of fluid in your lungs. A main cause of pulmonary edema is congestive heart failure. It can occur due to nonheart-related conditions, too. Symptoms include shortness of breath and difficulty breathing. Sudden (acute) pulmonary edema requires immediate treatment. Pulmonary edema can also develop over time (chronic).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
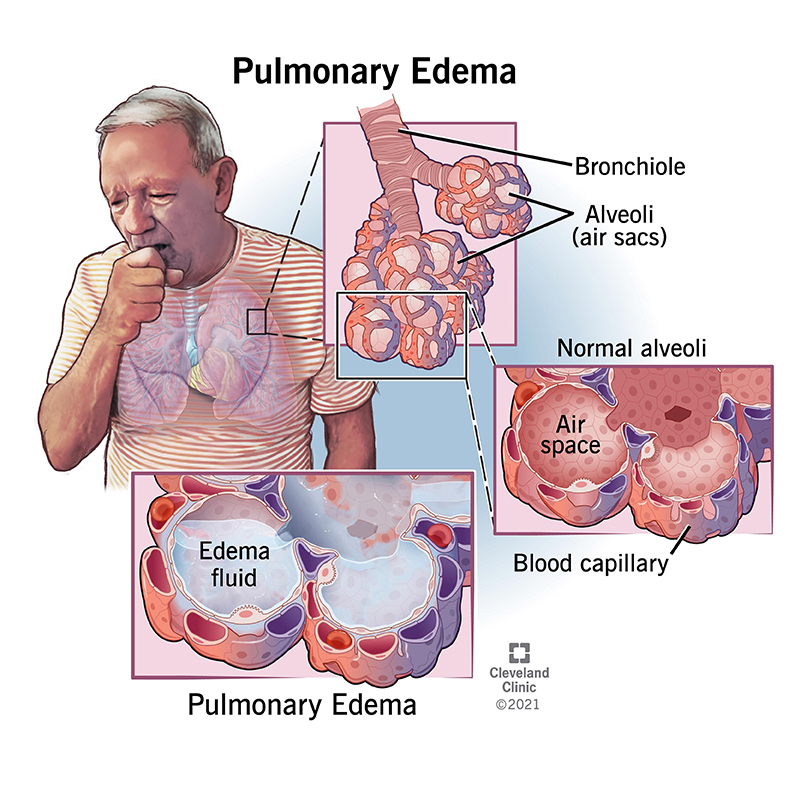
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24218-pulmonary-edema)
Pulmonary edema is the abnormal buildup of “fluid in the lungs.” Fluid buildup in your lungs can lead to shortness of breath, coughing up of foam and loose mucus, wheezing, chest tightness and difficulty breathing. Pulmonary edema can be life-threatening and requires immediate medical treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
High altitude pulmonary edema (HAPE) occurs when you’re at high altitudes or if you’re rapidly going up (ascending) a mountain. HAPE is a severe form of altitude sickness (also known as mountain sickness), which occurs because oxygen levels are lower at higher altitudes.
HAPE can make you tired, weak, achy and short of breath. It can cause coughing and chest tightness. HAPE is a medical emergency and can be life-threatening. If you have HAPE, you need to go down (descend) immediately and receive medical treatment.
Both pulmonary edema and pneumonia involve a buildup of fluid in your lungs. An infection causes pneumonia. The infection can be viral, bacterial or fungal. These organisms can cause infected fluid to fill your air sacs. An infection doesn’t cause pulmonary edema, and the fluid is typically thinner and watery.
Pleural effusion is when abnormal amounts of fluid buildup outside of your lungs in the pleura, which is a lining around your lungs. The pleura sits between your lungs and the inside of your chest wall, and usually only has a thin rim of fluid inside it. Pleural effusion is commonly caused by pneumonia, congestive heart failure or cancer. Unlike pulmonary edema, the fluid sits outside of your lungs and can compress your lungs, which are spongy.
Advertisement
Immersion pulmonary edema is sometimes called swimming-induced pulmonary edema. It occurs when competitive swimmers and divers develop lung injuries because their lung capillaries burst. During diving, blood is sent to your lungs from your legs and abdomen. That excess blood increases pressure in the blood vessels of your lungs. The vessels leak, and the fluid goes into your air sacs.
The causes of pulmonary edema can be broken down into two groups: cardiogenic (heart-related) or noncardiogenic (not heart-related).
Cardiogenic pulmonary edema means fluid backs up in your lungs from a heart problem. The most common cause of cardiogenic pulmonary edema is congestive heart failure. When the left side of your heart stops pumping blood correctly, the blood backs up into the blood vessels in your lungs. As the pressure in your blood vessels increases, fluid is pushed into the air sacs in your lungs.
Congestive heart failure that leads to pulmonary edema can be from:
Noncardiogenic pulmonary edema occurs when other diseases cause fluid to accumulate in your lungs. It isn’t caused by increased blood flow in your lungs due to a backup from heart problems. Instead, the blood vessels in your lungs become inflamed or injured. The blood vessels then become leaky, and fluid goes into your air sacs.
Adult respiratory distress syndrome (ARDS) is another common name for noncardiogenic pulmonary edema. In ARDS, inflammation is the main problem, with causes that include:
Negative pressure pulmonary edema can occur after a blockage in your upper airway. Straining to breathe when this obstruction happens causes injury to your pulmonary blood vessels, and they leak into your air sacs. In high altitude pulmonary edema (HAPE), your pulmonary blood vessels constrict and become leaky.
Pulmonary edema can come on suddenly (acute) or develop as a long-term (chronic) condition.
Signs and symptoms of sudden pulmonary edema include:
Advertisement
The signs and symptoms of long-term pulmonary edema include the same symptoms as sudden pulmonary edema, although the symptoms may be milder. Other symptoms of long-term pulmonary edema include:
A healthcare provider will perform a physical exam to see if you have fluid in your lungs. They’ll listen to your heart and lungs with a stethoscope. They’ll be examining you for:
If your healthcare provider thinks you may have fluid in your lungs, they’ll order additional tests, including:
Pulmonary edema is a serious condition. If you have sudden (acute) pulmonary edema, you need immediate treatment. You may need to be treated in the emergency room (ER) or intensive care unit (ICU).
Advertisement
Some treatment options include:
If you’re at a higher risk of pulmonary edema, you can take steps to take care of yourself. These steps include:
Sudden (acute) pulmonary edema can be life-threatening. Call 911 or go to the emergency room (ER) if you have any of the following symptoms:
Advertisement
Survival rates depend on the cause of the condition and how quickly you receive treatment. If you have acute (sudden) pulmonary edema, you need immediate treatment.
Severe cases of pulmonary edema can be life-threatening if you don’t receive treatment right away.
Pulmonary edema is a serious condition. If you have acute (sudden) pulmonary edema, you need immediate treatment. You may be treated in the emergency room (ER) or intensive care unit (ICU). Chronic pulmonary edema may require hospitalization as well.
Pulmonary edema is a serious medical condition. If you have acute (sudden) pulmonary edema, you need to be treated right away. The outlook for pulmonary edema depends on the cause of the condition, how severe your case is and how quickly you receive treatment. With immediate treatment, your chances of recovery are higher. Be sure to keep in contact with your healthcare provider, and get immediate help if you have any symptoms of pulmonary edema.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
