Tricuspid valve regurgitation is when the valve between your right atrium and right ventricle doesn’t fully close. This causes some blood to flow the wrong way. Trace tricuspid regurgitation (a small amount of backward flow) isn’t a concern. But severe regurgitation can cause symptoms and complications. Treatment includes medications and surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
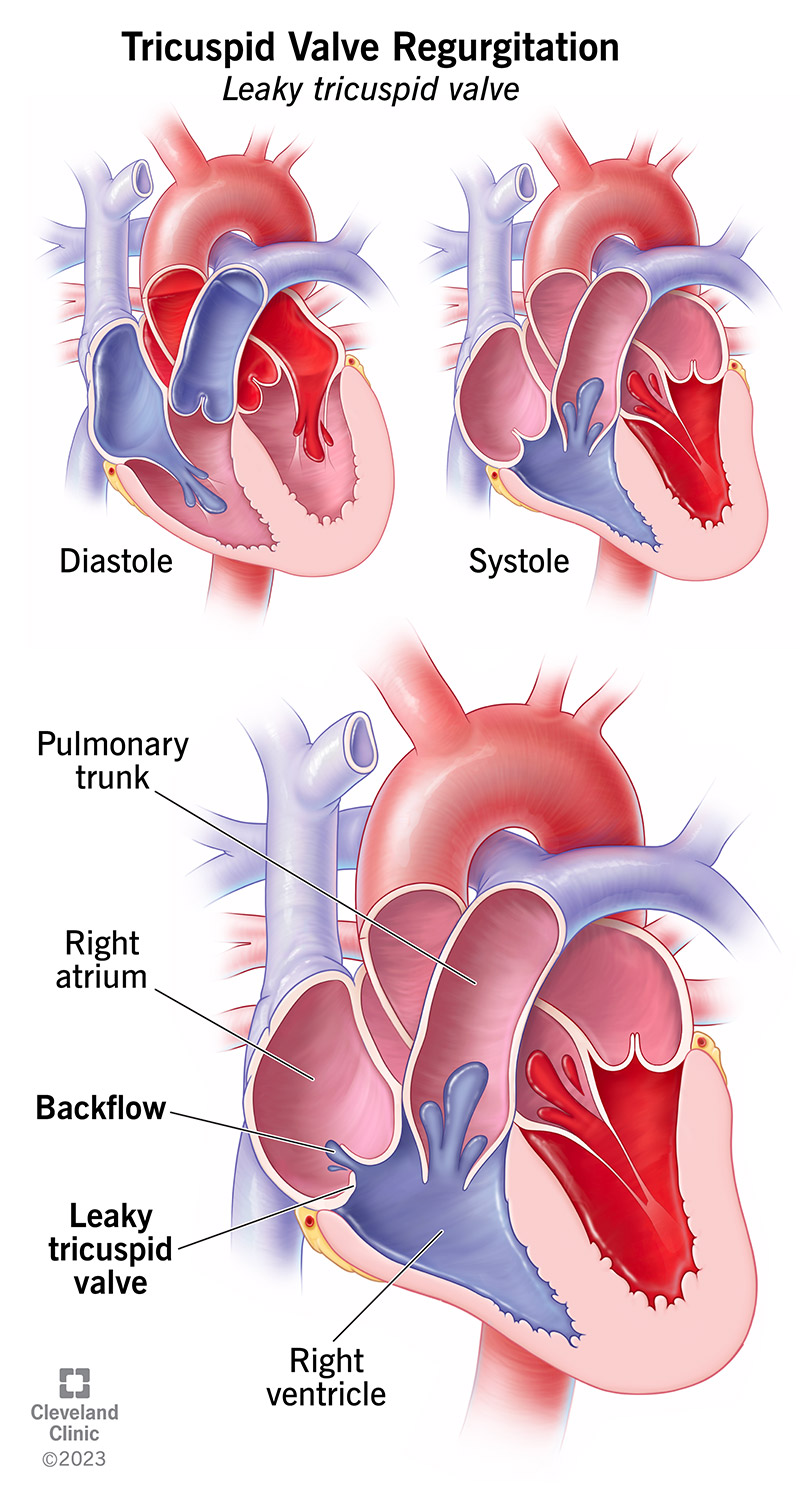
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21627-tricusp-valve-regurgitation-illustration)
Tricuspid valve regurgitation is when the “door” connecting the upper and lower chambers on the right side of your heart doesn’t properly close. This leaky door allows some blood to flow backward each time your heart beats. Tricuspid valve regurgitation is a form of heart valve disease. It can range from trivial (no effects on your body) to severe. Over time, moderate to severe backward blood flow through any of your heart valves can make your heart work harder and take a toll on your cardiovascular system.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Other names for this condition include:
To understand this condition, it helps to know a bit about how your tricuspid valve works.
Your tricuspid valve manages blood flow from your right atrium down into your right ventricle (which pushes the blood into your main pulmonary artery). It’s made of a tough, fibrous ring (annulus) that supports three leaflets, or flaps. These leaflets open when your heart relaxes (diastole) to let blood flow from your right atrium into your right ventricle. They close when your heart contracts (systole) to prevent blood from flowing the wrong way, back into your right atrium.
When you have tricuspid valve regurgitation, your leaflets don’t fully seal when your heart contracts. As a result, some of the blood that should get pushed into your pulmonary artery leaks backward into your right atrium. Greater amounts of backward flow lead to more severe valve disease.
Trace, or trivial, tricuspid valve regurgitation (a very small amount of backward flow) is common and harmless, and you won’t feel any symptoms. Mild tricuspid valve regurgitation also causes no symptoms and should have little or no impact on your life. However, your healthcare provider will monitor your condition and may recommend lifestyle changes.
Advertisement
Moderate to severe tricuspid regurgitation is more serious. It may cause symptoms and require treatments ranging from medications to surgery.
There are three types of tricuspid regurgitation:
Moderate to severe tricuspid regurgitation affects between 5 in 1,000 and 8 in 1,000 people in the U.S.
Many more people have trace (also called trivial) tricuspid valve regurgitation. This means the structure of their valve is usually normal, but a very small amount of blood leaks backward with each heartbeat. Trace regurgitation doesn’t cause any symptoms or lead to complications. But it’s a common finding in advanced imaging tests.
Trace or mild tricuspid regurgitation causes no symptoms. You may have symptoms with moderate to severe regurgitation, often due to the underlying conditions causing it.
Possible symptoms (things you feel) include:
Possible signs (things your healthcare provider may notice) include:
Structural changes to the right side of your heart cause most cases of moderate to severe tricuspid regurgitation. Such changes can occur when there’s consistently too much pressure or blood in the right side of your heart. This overworks your right atrium and right ventricle, causing one or both to enlarge.
As one or both of these chambers get bigger, the tough ring (annulus) that supports your tricuspid valve leaflets may grow wider. Healthcare providers call this “annular dilation.” When the annulus is too wide, the leaflets it supports can’t fully come together (coapt).
Advertisement
Also, in some cases, the strong cords of tissue that connect your leaflets to your heart muscle and provide support to the leaflets may become tethered, or limited in their range of motion. These problems prevent your leaflets from closing properly, leading to a leaky valve.
Many different medical conditions can cause your right atrium and/or your right ventricle to enlarge. Examples include:
People with tricuspid regurgitation due to an enlarged heart have the “secondary” form of the condition. This means the leaky valve happened because of another medical issue, and the valve’s leaflets are structurally normal.
Less often, tricuspid regurgitation results from abnormal or damaged valve leaflets. Healthcare providers call this form “primary tricuspid regurgitation.” It has many possible causes, ranging from medical conditions to trauma.
Factors that can damage your tricuspid valve leaflets, leading to a leaky valve, include:
Advertisement
Severe tricuspid regurgitation can cause organ damage and lead to:
Your healthcare provider will perform a physical exam and order tests as needed to diagnose this condition.
During a physical exam, your provider will use a stethoscope to listen to your heart and breathing. A heart murmur is sometimes detectable during an exam. Your provider may also feel your neck and belly (near your liver). Feeling a strong pulse in either place is a sign of tricuspid regurgitation.
Healthcare providers typically use echocardiography to diagnose tricuspid regurgitation. This test can also identify any valve abnormalities that would indicate the primary form of the condition. Rarely, if an echocardiogram doesn’t provide enough information, providers order a cardiac catheterization.
Other tests your provider may order to find the cause of regurgitation or learn its effects on your body include:
Treatment of tricuspid regurgitation can involve one or more of the following:
Advertisement
Your provider will tailor a treatment plan to your needs, including the severity of the regurgitation and its causes.
The impact on your daily life depends on your condition’s cause and severity. Your healthcare provider is the best person to tell you how this condition may affect your routine. They may recommend you make lifestyle changes or take medications to improve your heart function or overall health. It’s important to follow your provider’s guidance and ask if anything is unclear.
It’s not always possible to prevent this condition, which has many possible causes. But you can take some steps to lower your risk.
Many different forms of heart disease can cause tricuspid regurgitation. So, keeping your heart as healthy as possible can help lower your risk of heart diseases that lead to a leaky valve. Here are some tips.
See your provider for yearly check-ups and go to all of your follow-up appointments. Your provider will tell you how often you need to come in.
Call your provider right away if you have new or worsening symptoms. You should also tell them if any symptoms start to interfere with your usual activities.
Call 911 or your local emergency number if you:
Tricuspid valve regurgitation is a medical condition that can affect your daily life greatly or not at all, depending on the severity. Thanks to advances in modern medicine, it’s possible to treat this condition with medications and surgeries. That’s why it’s important to see a healthcare provider regularly. Your provider will keep an eye on your heart health and diagnose any valve problems early, before they can damage your heart or other organs.
If your provider mentions you have trace or trivial tricuspid valve regurgitation, don’t panic. This is common and doesn’t affect your heart function. Your provider will tell you if there’s a reason for concern and what you can do to manage your condition.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Problems with your heart can be scary. Our experts can diagnose and treat mitral & tricuspid heart valve disease.
