Bradycardia (low heart rate) is when your resting heart rate falls below 60 beats per minute. There’s a wide range of causes, including aging, inflammatory conditions and certain medicines. Providers treat the underlying cause and, in some cases, implant a pacemaker. Athletes naturally have a lower heart rate that’s not a cause for concern.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
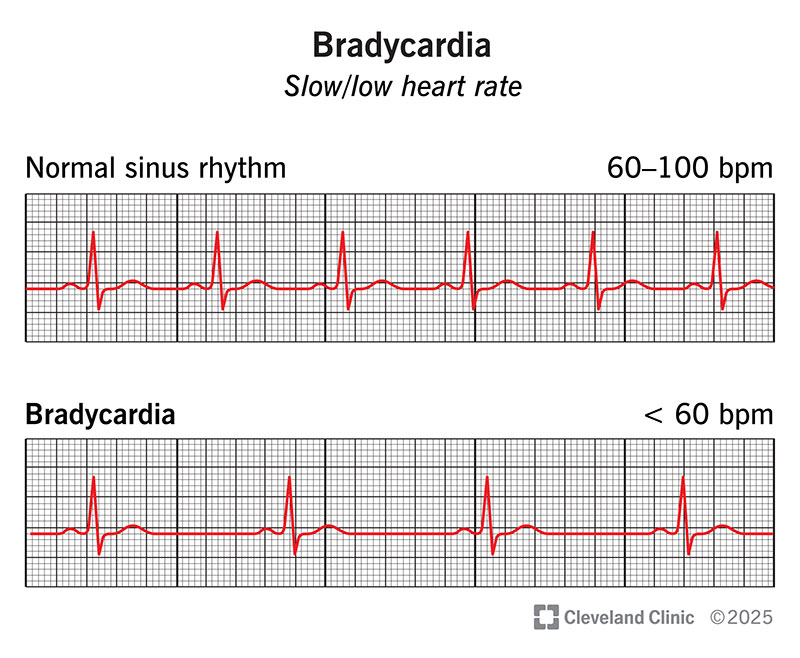
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17841-bradycardia)
Bradycardia, sometimes called a bradyarrhythmia, means your heart rate is below 60 beats per minute (bpm). It’s also called a low heart rate or slow heart rate. It’s normal for some people. But common causes that may need treatment include electrolyte imbalances, infections and certain heart conditions. Treating the cause can often restore a normal heart rate (60 to 100 bpm).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Bradycardia isn’t always a sign that something’s wrong. For example, if you’re an athlete, your heart is trained to pump blood more efficiently. This means it can beat more slowly while still sending enough blood to your body. It’s also normal for your heart rate to drop a bit while you sleep. This is called sinus bradycardia, meaning that the electrical system of your heart is still working appropriately.
It’s not always easy to tell if a low heart rate is normal or a cause for concern. That’s why if you notice your heart rate is lower than usual, you should contact a healthcare provider.
For many people, bradycardia doesn’t cause any symptoms. This is common among athletes with a low heart rate. But it’s also possible to feel totally fine yet have an issue that needs treatment.
Low heart rate symptoms may include:
These symptoms can develop if your heart isn’t pumping enough blood to meet your body’s needs. If your heart rate is unexpectedly low and you have any of these symptoms, seek medical care right away.
Problems with your heart’s conduction system cause bradycardia. Specifically, you can develop a slow heart rate if your heart’s natural pacemaker isn’t working as expected (sinus node dysfunction) or signals have trouble traveling from your upper to lower heart chambers (heart block). These are electrical issues — just like when your home Internet is slow or signals can’t get through to your TV.
Advertisement
Lots of things can disrupt your heart’s electrical activity, leading to bradycardia, including:
Healthcare providers diagnose bradycardia through a physical exam and testing. During the exam, they’ll review your medical history and ask about any symptoms. Be prepared to share details like how often you have symptoms, how long they last and what seems to trigger them.
For example, you might notice symptoms during exercise, when you shift positions, after you eat or after you take certain medicines. Keep notes on how and when heart rate changes happen. That info can help your provider make a diagnosis.
An electrocardiogram (ECG/EKG) is a key test that providers use to diagnose bradycardia. But it only tracks your heart’s electrical activity for less than a minute. This means it might not capture a low heart rate episode as it’s happening. For this reason, your provider may recommend ambulatory monitoring. This means you wear a device as you go about your daily routine.
Other tests you might need include:
Treatment for a low heart rate depends on the cause and how it’s affecting your body. There are so many different causes of bradycardia that providers need to tailor treatment to your needs. It may be as simple as switching up your usual medicines. Or you might need to take new medicines or have a procedure to fix an issue with your heart.
Advertisement
In general, to treat bradycardia, your provider may:
If you’re otherwise healthy and don’t have symptoms, you may not need treatment for bradycardia. This is the case with athletes who naturally have a low heart rate.
You should see your healthcare provider for an annual physical, whether you have bradycardia or not. These visits let your provider catch many health problems early, especially ones that don’t have symptoms you can feel.
Advertisement
If you’ve been diagnosed with bradycardia, your provider will tell you how often to come back for appointments. Always call your provider right away if you have new or changing symptoms.
Call 911 or your local emergency services number if:
Bradycardia is treatable and often curable. If you have bradycardia because of another condition, treating that condition may be all it takes to get your heart rate back to normal. In general, you’re more likely to have a good outcome with early diagnosis and treatment.
Bradycardia may be temporary or something you manage for the rest of your life. It depends on the cause. Your provider can tell you more about what to expect.
If your heart rate is slow (40 to 60 bpm) but you don’t have symptoms, there’s usually no reason to worry. But you should still tell your healthcare provider so they can make sure there’s nothing going on that needs treatment.
If your heart rate drops into the 30s, that’s getting into dangerous territory. You might not get enough oxygen to your brain. This can cause fainting, lightheadedness and shortness of breath. Seek medical attention right away.
Advertisement
Maybe you glanced at your fitness watch and noticed your heart rate was unusually low. Perhaps the watch even alerted you. Or maybe your healthcare provider mentioned your low heart rate at a checkup. No matter your situation, it’s common to worry when you learn your heart is beating too slowly.
Fortunately, for many people, bradycardia is temporary and treatable. Your provider will explain which treatments you might need and what you can expect.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
