Fat embolism syndrome is a rare condition that usually follows breaking a major bone. It most often happens when you break your pelvis or a bone in your legs, but can rarely occur with other medical conditions or circumstances. Most people with this condition recover fully and don’t have any long-term effects.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
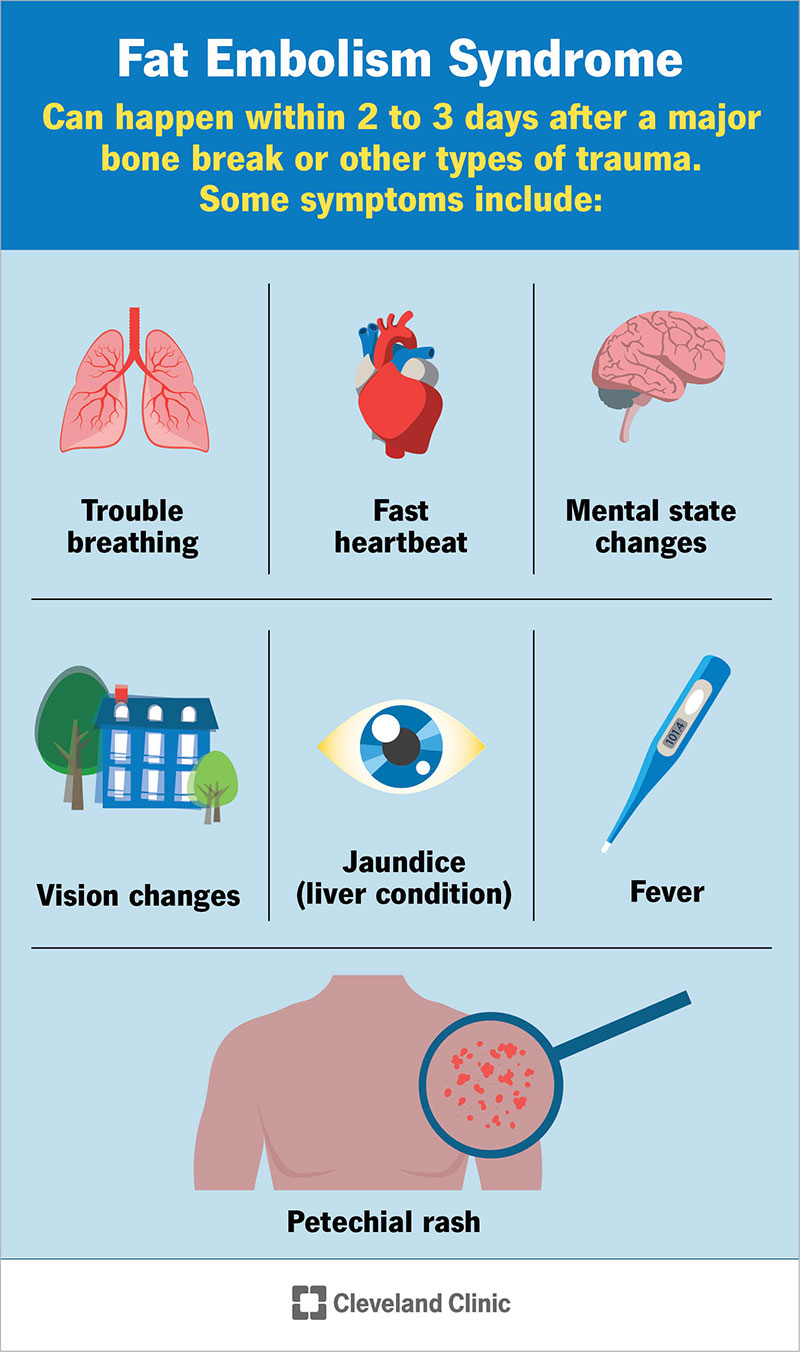
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/23995-fat-embolism-syndrome)
Fat embolism syndrome is a condition where particles of fat get into your bloodstream and block blood flow. Blockages can affect your brain, lungs, skin and other areas. This condition is rare and usually isn’t serious, but it can be dangerous when it's severe.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Breaking down the differences between a pulmonary embolism and a fat embolism starts with defining some key terms.
While blood clots are far more likely to cause pulmonary embolism, fat embolisms can still cause pulmonary embolisms, too (which are life-threatening medical emergencies). Fat embolism syndrome also causes problems with breathing even when it doesn’t cause a pulmonary embolism.
A fat embolism can happen to anyone, but they are extremely rare in children. This condition is most likely to happen when you fracture your pelvis (the bone that forms your hips) or the long bones in your body.
In rare cases, other conditions or circumstances can also cause this condition. Some examples include:
While a fat embolism can happen every time you fracture a bone, it’s usually not enough to cause a problem.
Advertisement
In people with an isolated break of a long bone like the femur, fat embolism syndrome happens in between 0.5% and 2% of all cases. When it involves multiple broken bones, especially fractures in your pelvis, this condition happens in between 5% and 10% of cases.
Fat embolism syndrome can be a dangerous condition at more serious levels because it can make it hard for you to breathe. At more severe levels, this disease is sometimes deadly because of how it affects your lungs, or because the impact on your lungs puts so much strain on your heart that your heart fails.
A fat embolism is when one or more droplet-like particles of fat enter your bloodstream and block circulation through some of your blood vessels. Fat emboli (the term for more than one) form anytime you break a bone, but they’re usually too small to cause any blockages. That means it’s rare for fat emboli (pronounced EM-bo-lye) to cause problems.
Fat emboli are much more likely to cause a problem when they happen after you break certain bones. About 95% of cases involve fractures of the pelvis or long bones in the body, especially the femur (thighbone), tibia (shinbone) and fibula (which runs behind the tibia) bones in the legs.
Most of the time, the particles of fat in your bloodstream can get stuck near the surface of your skin in smaller blood vessels called capillaries, causing a rash and other mild symptoms. Fat emboli can also affect small vessels in critical areas like your heart, brain, eyes or lungs, causing severe and life-threatening problems.
Three specific effects are usually enough for a doctor to diagnose this condition (though a diagnosis is also possible without all three). Those include a distinctive rash on your skin and effects on your brain and lungs.
Fat embolism syndrome usually happens within 2 to 3 days after a major bone break or other types of trauma. But it can happen as soon as 12 hours after an injury. The main symptoms include the following:
Advertisement
Other possible symptoms include:
Doctors may also test for the following clinical signs. These are changes that diagnostic and lab tests can find but that you can’t feel as symptoms:
Fat embolism syndrome isn't contagious.
At this time, there’s no universally accepted standard for diagnosing this condition. Because of that, doctors make this diagnosis based on your symptoms, a physical exam, diagnostic and lab testing.
The physical exam involves a doctor looking at your body for signs and symptoms of potential medical problems. They may also listen to your heart and breathing with a stethoscope.
The three main symptoms of this condition, trouble breathing, mental status changes and petechial rash, are signs and symptoms that are usually visible. That means in many cases, especially those that are more severe, a physical examination is enough to diagnose this condition.
Testing for this condition can include any of the following.
Advertisement
There’s no cure for fat embolism syndrome, and there’s no standard treatment plan for cases of the condition. Treatments for fat embolism syndrome can include medications, life-supporting devices and treatments to prevent further complications.
The main goal with this condition is providing supportive care. That means healthcare providers focus on treating the symptoms and effects of the underlying disease rather than the disease itself.
Possible treatments used with fat embolism syndrome include:
Advertisement
Fat embolism syndrome typically doesn’t have any direct complications. However, severe cases can result in long-term effects in your brain, eyes or lungs. However, most people will go on to recover fully. You should ask your healthcare provider about the possible and likely side effects or complications in your case. They are the best source of information because they can tailor that information to your specific circumstances and needs.
Some evidence suggests fat embolism syndrome can put you at a greater risk for problems like deep vein thrombosis or long-term effects on your brain. However, that evidence isn't confirmed, and it will take more research to determine if this is the case.
Because fat embolism syndrome can cause problems with your breathing and disrupt your brain's normal functions, you shouldn't try to care for it independently. The best thing to do is to go to the hospital and seek medical attention.
Fat embolism syndrome is deadly in between 5% and 20% of cases, with the death rate trending downward for several years now. The drop in the death rate is largely due to preventive measures and better in-hospital monitoring for those at greatest risk.
Fat embolism syndrome is most dangerous when it causes severe breathing problems or heart failure. The risk for developing either of those problems is highest when this condition is severe or when there are delays in treatment.
In moderate and mild cases, fat embolism syndrome usually resolves on its own and rarely causes long-term effects.
In most cases, fat embolism syndrome isn't a severe condition, and it goes away on its own within a few days. It can take days or weeks for any skin or neurological (brain-related) problems to go away in severe cases. Respiratory problems will usually go away on their own within a year. Respiratory problems that don't get better on their own usually aren't severe enough to need ongoing medical care.
Because fat embolism syndrome often follows broken bones, it's very common for people to have broken bones stabilized. This usually involves realigning and immobilizing broken bones, but it can also involve surgery with more severe fractures.
Healthcare providers may also prescribe corticosteroids after a severe fracture to try and prevent this condition from developing. However, more research is necessary to confirm if the benefits from this approach are greater than the potential risks.
In general, most people won’t need to take special precautions after fat embolism syndrome. However, it’s important to be careful with any broken bones that led to developing the condition. Re-breaking a bone may cause this condition (if you didn’t have it before) or cause it to happen again.
If you have specific questions about your circumstances and case, your healthcare provider is the best person to guide you on what you can to help yourself as you recover from this condition.
Your provider will likely recommend follow-up visits and care to monitor any long-term effects related to fat embolism syndrome, but these are rare. Your provider can also tell you the signs and symptoms to watch for that indicate you need medical attention.
You should go to the hospital anytime you have a broken arm or leg. Hospital facilities can best treat these kinds of fractures and help you avoid complications or other problems.
You should also go to the hospital if you have fat embolism syndrome and start having changes in your mental state or any symptoms related to pulmonary embolism.
Mental health change symptoms include:
Pulmonary embolism symptoms include:
Fat embolism syndrome is a rare condition that usually goes away on its own without long-term impacts. However, it can be dangerous or even deadly in some cases — especially severe cases or those that don't get quick treatment. Fortunately, advances in medical care have greatly reduced the risks from this condition, especially with fast diagnosis and treatment.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
