Heart valve disease affects the valves that keep your blood flowing in one direction through your heart. Common types of heart valve disease include narrowing (stenosis), backward flow (regurgitation) or stretchy, floppy leaflets that don’t close tightly (prolapse). Treatments include medicines, valve repair or valve replacement.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
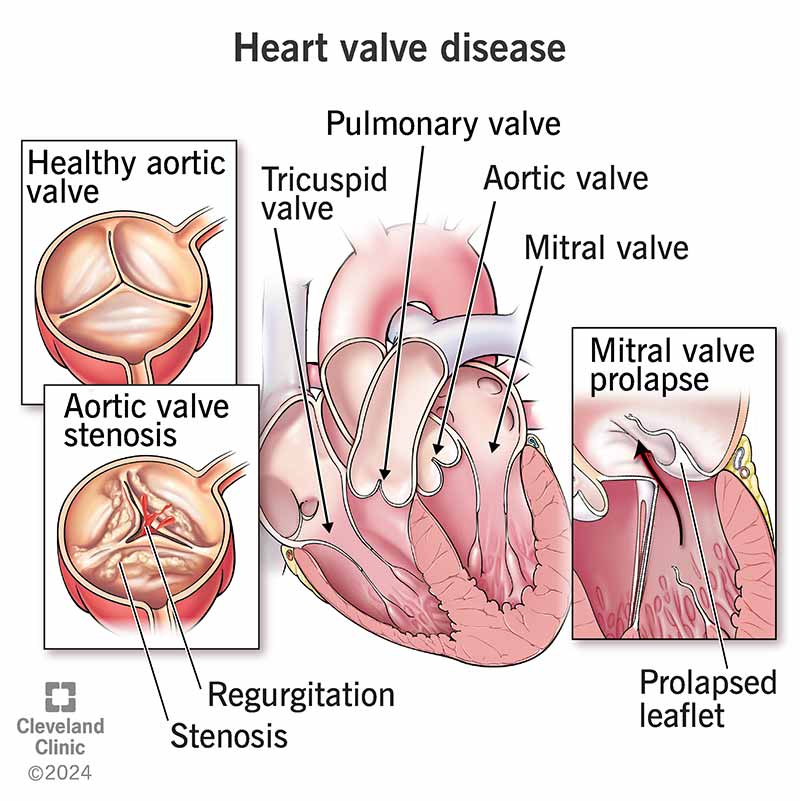
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17639-valve-disease)
Heart valve disease refers to any of several conditions that prevent one or more of the valves in your heart from working right. Left untreated, heart valve disease may reduce blood flow and cause your heart to work harder. Untreated heart valve disease can become life-threatening.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
But there’s hope. In many cases, your healthcare provider can do surgery or a minimally invasive procedure to repair or replace your heart valves. This restores normal function and allows you to return to normal activities.
The four valves in your heart make sure blood flows in only one direction through your heart. Your valves consist of small flaps of tissue (called leaflets) that open to allow blood to move forward through your heart during half of your heartbeat. These leaflets close to prevent blood from flowing backward during the other half of your heartbeat.
Your heart’s valves are:
There are different types of heart valve disease: stenosis, regurgitation, prolapse and atresia. They can affect more than one valve.
Tissues forming the valve leaflets become stiffer, narrowing your valve opening and reducing the amount of blood that can flow through it. Mild narrowing may not reduce the overall functioning of your heart. But the valve can become so narrow (stenotic) that it reduces your heart’s function, makes your heart pump harder and puts it under strain. As a result, the rest of your body may not get enough blood flow.
Advertisement
Also known as insufficiency or "leaky valve," this happens when your leaflets don’t close completely. This lets blood leak backward across your valve. Your heart has to pump harder to make up for this backward flow, and the rest of your body may get less blood flow.
Your mitral valve may not close tightly because the leaflets are extra stretchy. They go back into your left atrium when your heart beats. This is usually harmless, but can lead to regurgitation in some people.
Valvular atresia happens when a heart valve forms without an opening before birth. Healthcare providers usually diagnose this very early in infancy.
About 2.5% of Americans — many of them older adults — have heart valve disease. Each year, roughly 27,000 people die from heart valve disease in the United States. Mitral valve prolapse is a common heart valve problem.
Many people with heart valve disease don’t have symptoms. But when the condition worsens over time, your heart beats harder to make up for the reduced blood flow.
Heart valve disease symptoms may include:
Common heart valve disease causes include:
Risk factors that give you a greater chance of getting heart valve disease include:
Untreated valve disease may eventually lead to:
During a physical examination, a healthcare provider may find these signs of heart valve disease:
Advertisement
Several medical tests can also show heart valve disease. Repeating tests over time can help your provider see the progress of your valve disease and make decisions about your treatment. Valve disease can get worse over time. You may hear a provider describe valve disease with a letter for its stage. Stages start with A and end with D, which is the most severe.
Tests for heart valve disease diagnosis include:
Advertisement
Heart valve disease treatments depend on the cause and may include:
Although you can’t undo damage to a heart valve, you can treat the issue. The decision to prescribe medical treatment, surgical repair or surgical replacement depends on several factors, including:
If you’re pregnant and have heart valve disease, you can get extra rest and/or take certain medicines that are safe for your baby.
If you know about your valve disease before pregnancy, ask your healthcare provider if you should have tests or see a cardiologist before trying to become pregnant. This can help ensure that you get the right treatment before and during pregnancy. If you have a severe valve problem, your provider may recommend valve repair or replacement before pregnancy.
Although medicines can’t cure heart valve disease, they — and a healthy lifestyle — can help with symptoms and decrease your chance of having a stroke or cardiac arrest. You may be able to stop taking some medications after valve surgery, but you may need to take other medicines for the rest of your life.
Advertisement
Your healthcare provider may prescribe medications to help you with:
Heart valve disease is a problem with the opening or closing of your leaflets, and you may need surgery to repair or replace your valve. Some infants who have congenital (present at birth) valve issues need surgery during childhood.
Usually, the surgeon and cardiologist will know which treatment will be best before surgery day. Other times, the surgeon decides during surgery, when they can see your valve.
Often, providers may combine valve surgery with other procedures (like bypass surgery or surgery to treat atrial fibrillation) to fully treat your heart disease.
Heart valve repair allows your surgeon to fix your faulty valve, often without the use of artificial parts. In some cases, like a narrow mitral valve, your provider may use a balloon on a catheter (valvuloplasty) to widen your valve. They may perform an annuloplasty to fix or reinforce the ring around your valve so it closes better.
The advantages of valve repair are:
Surgeons have to replace valves they can’t repair. Replacing your heart valve involves removing your old valve and sewing a new valve to the ring-shaped part of your old one. The new valve could be mechanical or biological (made with tissue from a human, cow or pig). These replacement valves can provide function when repair can’t. But depending on the type of valve you get, you may have to take certain medications to prevent blood clots or get a new valve again in 10 or 15 years.
Depending on the type of valve problem and your other medical conditions, you may be able to have minimally invasive valve repair or replacement.
Older people and those whose health isn’t good to begin with have a higher risk of complications from valve replacement surgery.
Complications, which are rarely fatal, may include:
You may be in the hospital for about five to seven days after heart valve surgery. After that, it can take about four to eight weeks to recover. Your provider may recommend cardiac rehab, a carefully monitored program to assist with your recovery.
If you have heart valve disease, you’ll have it for your whole life. But your experience of heart valve disease depends on the valve affected and the severity of the problem.
Some people may have valve disease and never experience any symptoms. Others may have many symptoms and need a valve repair or replacement. Even if your healthcare provider repairs or replaces your valve, you’ll still need to take medicine and possibly have another replacement in 10 or 15 years.
It’s important to follow up regularly with a healthcare provider to monitor the progression of your valve disease over time.
Although you can’t change some risk factors, like growing older, there are things you can do that may reduce your risk of heart valve disease. These include:
If you have heart valve disease, ask your healthcare provider about the increased risk of getting infective endocarditis. This infection can damage or destroy your heart valves and can be fatal. You’re at risk even if you had surgery to repair or replace your valve. To prevent infective endocarditis:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_mhp4cjbq/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn about heart valve disease from vascular surgeon, Lee Kirksey, MD.
Keep taking any medicines your healthcare provider prescribed for you and go to all follow-up appointments.
You’ll need to schedule regular follow-up visits with your cardiologist to make sure your heart valves work as they should. Ask your provider how frequent these visits should be. You may also need to repeat tests, like an echocardiogram.
Contact your provider sooner if your symptoms become more severe or frequent. You should also tell your provider if you have infective endocarditis.
You should call 911 or your local emergency number if you have these symptoms after heart valve surgery:
Questions to consider asking your provider include:
It can be a relief to know that the fatigue you’ve been feeling isn’t part of aging. The good news about a heart valve issue is that you can manage it with medications and/or surgery. Your healthcare provider can talk with you about the best option for you. Regardless of what your provider does, you can help yourself feel better by being more physically active, eating heart-healthy foods and avoiding tobacco products. Be sure to keep taking any prescribed medicines and go to all of your follow-up appointments.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
It can be scary and overwhelming when something is happening with your heart valves. Cleveland Clinic heart specialists are ready to get you the help you need.
