Aortic valve stenosis (or aortic stenosis) happens when the aortic valve in your heart is narrowed or blocked. This interferes with the normal blood flow out of your heart. It makes your heart work harder, causing heart damage, major health problems and even death. Replacing the valve is the best treatment and gives you a good prognosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
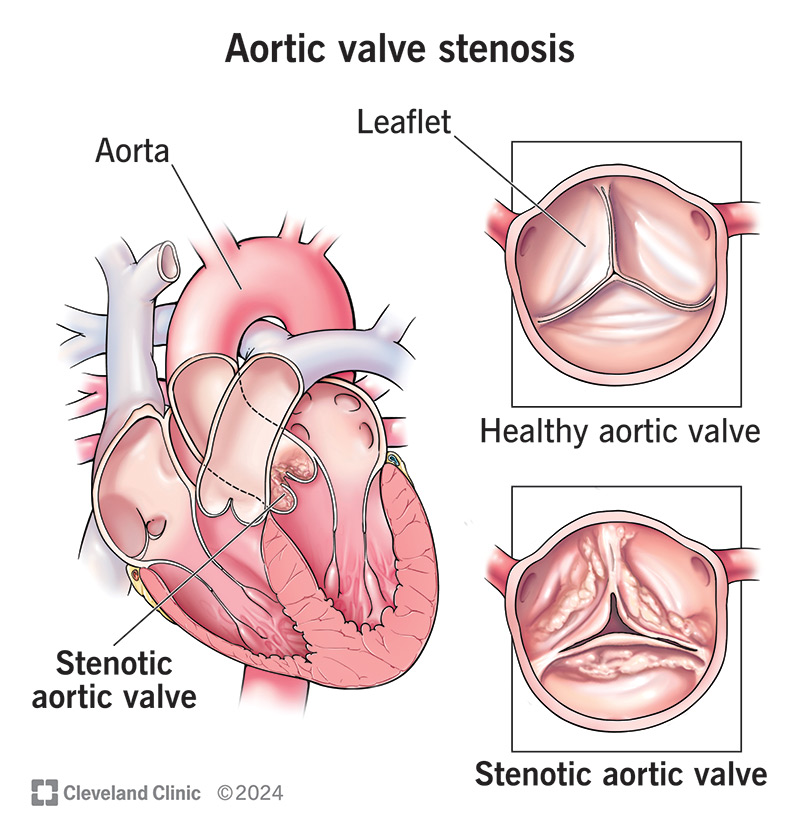
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23046-aortic-valve-stenosis)
Aortic valve stenosis (or aortic stenosis) describes an aortic valve in your heart that’s narrowed or blocked. This interferes with the normal blood flow out of your heart. Because this condition restricts blood flow, it also limits how much oxygen your body gets. This can cause chest pain, shortness of breath and fainting. Aortic stenosis can cause heart damage, major health problems and even death.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
One of four valves in your heart, your aortic valve is the last one that blood flows through before going out to your body. Your aortic valve has three flaps (leaflets) that open to let blood pass through and then seal shut to keep blood from flowing backward into the last heart chamber.
A problem with this valve can be concerning. But today, there are more options than ever to treat aortic stenosis.
Aortic stenosis is common in people over 65. But many people don’t know they have it until it causes symptoms or shows up on a screening or diagnostic test.
Several diseases can also cause it to develop when people reach middle age. In rare instances, children can have a congenital (present at birth) condition that causes aortic valve stenosis.
Aortic stenosis symptoms (progressing from less severe to more severe) include:
Your primary care provider may refer you to a cardiologist (heart doctor) if they suspect you have aortic stenosis.
Advertisement
For some people, aortic valve stenosis can happen slowly and take several years. For others, it can happen much faster. If you wait too long for treatment, you may have heart damage that a provider can’t repair or reverse. In cases of severe aortic stenosis, there’s also a risk of dying suddenly. Because of this, your healthcare provider may advise you not to delay treatment.
Aortic stenosis in adults has three main causes:
Risk factors for aortic valve stenosis include:
When you have aortic stenosis, it takes more effort to move blood through your aortic valve. Your heart works harder than it should to push the blood through. This can lead to a heart attack, heart failure or sudden cardiac death.
People with aortic valve stenosis may also get pulmonary hypertension, bleeding or infective endocarditis.
A cardiologist will typically diagnose this condition based on your symptoms (if you have them) and one or more of the following diagnostic tests:
Advertisement
Based on your symptoms and how well your aortic valve works, your provider may describe your case with a letter and, possibly, a number after it. Stages run from A through D, with D being the worst. Numbers 1 through 3 further describe cases, with 3 being the worst.
If you have stenosis but no symptoms, your healthcare provider may advise you to simply monitor the issue with follow-up visits and tests. If you develop symptoms, your provider can offer you aortic stenosis treatment options, including:
Advertisement
Recovery from aortic valve stenosis repair or replacement depends on the method a provider uses. Surgical methods take the longest. People who have surgery are typically in the hospital for several days, with full recovery usually taking several weeks.
Transcatheter methods like balloon valvuloplasty and TAVR have shorter recovery times. In some cases, people who have these types of procedures can go home either the same or the next day and resume their everyday lives shortly after.
Your outlook with aortic stenosis depends on how quickly you get treatment.
Advertisement
Treating bacterial infections promptly is the only way to prevent aortic stenosis. This includes taking antibiotics and other medications as directed, not just until you feel better.
You usually can’t prevent aortic valve stenosis that results from aging or from inherited or chronic conditions.
If you have mild aortic stenosis or no symptoms, you may only need routine echocardiograms and regular follow-up appointments.
If you have moderate aortic valve stenosis, you may need to monitor symptoms, get routine echocardiograms and limit your activity. You may also need to take medications to prevent clotting or treat other issues related to aortic stenosis. You may need to take medication either temporarily or permanently. Your healthcare provider can explain what medications you’ll need to take, how you should take them and for how long.
With severe aortic valve stenosis, you’ll likely need follow-up visits after a valve repair or replacement. You may also need to take certain medicines.
For all severity levels, your provider will likely recommend eating low-salt, low-fat foods and getting regular physical activity. They can tell you what level of activity is right for you.
If you choose not to have treatment or haven’t received treatment yet, you should call your healthcare provider if the following happens:
After starting a new medication, you should go to the emergency room if any of the following happens:
After a surgery or catheter procedure, you should go to the ER if any of the following happens:
Questions to consider asking your provider include:
There’s a part in your heart that isn’t working right. What now? Talking to a healthcare provider about aortic stenosis sooner rather than later, especially if you have symptoms, can make a huge difference in your life. Aortic stenosis is a complicated condition, but advances in surgical and catheter-based techniques mean the ability to treat it has never been better.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your child is diagnosed with aortic valve stenosis, they’ll have a lifetime of heart care ahead. Cleveland Clinic Children’s gives them a great head start.
