Your body is held together by tissues that connect all the structures in your body. When you have a connective tissue disease, these connecting structures are negatively affected. Connective tissue diseases include autoimmune diseases like rheumatoid arthritis, scleroderma and lupus.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
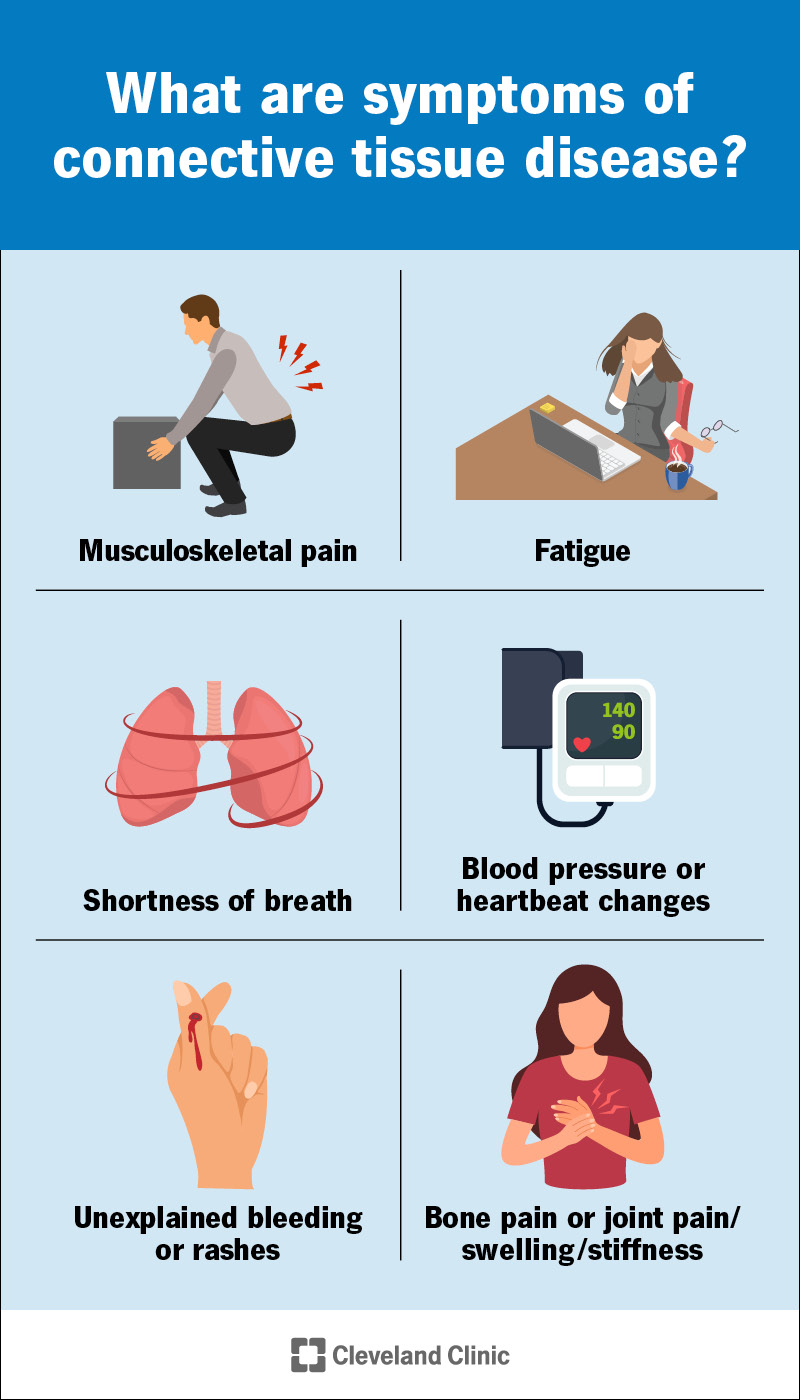
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/connective-tissue-diseases-infographic)
“Connective tissue disease” is an umbrella term for a wide range of diseases that can affect your connective tissues. These are the tissues that connect and support your organs and body structure. They hold your muscle fibers together and cover and protect your nerves. They also include your:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As these tissues are in almost every part of your body, connective tissue diseases can also affect you all over. They might affect one or two types of tissues throughout your body or many. They can also affect many organs. Different types of connective tissue disease have different symptoms.
There are over 200 known connective tissue disorders. They fall into three main categories:
Autoimmune diseases are what many people think of when they think of connective tissue disease. In these conditions, your immune system generates chronic inflammation in some parts of your body. Chronic inflammation causes pain, swelling and, eventually, permanent damage to your tissues.
Some examples of autoimmune connective tissue disorders include:
Advertisement
If you have overlapping features of several autoimmune connective tissue disorders, it’s called mixed connective tissue disease. If you have some symptoms of some autoimmune diseases, but they don’t meet the criteria for any specific disorder, it’s called undifferentiated connective tissue disease.
Genetic disorders of the connective tissue result from a gene mutation that you inherit at birth. The mutation affects how your connective tissues develop. It usually affects one of the two primary building blocks in all connective tissues: collagen or elastin. This causes various defects in your tissues.
Examples of hereditary connective tissue diseases include:
People born with these conditions can have a wide variety of symptoms and complications, ranging from mild to severe. As healthcare providers can’t treat the genetic defect, they treat the symptoms and complications individually as much as they can. They’ll monitor your condition throughout your life.
The type of cancer that can start in your connective tissues is called sarcoma. Sarcomas can start in your bones, cartilage, fat, muscles, ligaments, tendons or the deep layers of your skin. They can also start in other “soft tissues” that aren’t technically connective tissues, like epithelium and endothelium.
Examples of connective tissue sarcomas include:
Different connective tissue diseases can cause a wide variety of different symptoms. But there are some common themes. For example, most connective tissue diseases can cause symptoms all over your body. Musculoskeletal pain, weakness and/or stiffness are common, as are systemic symptoms, like fatigue.
Advertisement
Many connective tissue disorders can affect your lungs and cardiovascular system. Your lungs have a lot of connective tissues and rely heavily on them. Blood vessels run through most of your connective tissues, and because they're made of similar stuff, inflammation spreads easily between them.
As a result, many connective tissue diseases can cause musculoskeletal symptoms together with cardiopulmonary symptoms, like shortness of breath and changes to your blood pressure or heartbeat. If your blood vessels become inflamed, they can swell and break, causing unexplained bleeding.
Sarcomas often won’t cause symptoms until they grow large enough to compress an organ or vessel. But some can cause bone pain or joint pain where they start. Others may appear as a lump under your skin that may or may not be tender. Most sarcomas can spread, causing more widespread symptoms.
Connective tissue disease happens when something in your body malfunctions. In autoimmune disease, your immune system launches an attack against your own body. In genetic diseases, a mutated gene causes your tissues to develop wrong. Cancer happens when cells continue to divide uncontrollably.
For the most part, scientists don’t know the underlying reasons why these malfunctions occur. But certain risk factors might play a part in making you more vulnerable to these diseases. Severe infections that overstress your immune system and exposure to certain toxic chemicals are possible risk factors.
Advertisement
Your doctor may order various tests depending on what type of connective tissue disorder is suspected. They’ll first ask for your medical history and a family history, and will do a physical examination. Further tests may include:
Most connective tissue disorders are lifelong conditions. Healthcare providers do what they can to reduce their severity and treat the symptoms and complications individually. Autoimmune diseases and sarcomas can go into remission — periods without any signs or symptoms. But they can also recur (return).
Healthcare providers treat autoimmune diseases with a combination of anti-inflammatory drugs (corticosteroids) and immune system-repressing drugs (immunosuppressants) to stop the automatic inflammation. Treatments for sarcomas include surgery, chemotherapy and radiation therapy.
Scientists are researching genetic therapies that may one day be able to reduce the effects of genetic connective tissue disorders. For now, providers can only treat the symptoms. In addition to medications, they recommend regular low-stress exercise or physical therapy to help manage musculoskeletal pain.
Advertisement
The wide range of connective tissue disorders have very different outlooks and possible complications. Your healthcare provider is the best person to tell you what signs and symptoms to look out for and when to seek treatment. They may also recommend lifestyle changes to help optimize your overall health.
Connective tissue disease affects the tissues that hold things together in your body. In normal circumstances, you probably wouldn’t notice these tissues doing their jobs. But when they’re diseased, you feel it — often, all over. These diseases can cause a vast array of symptoms and complications.
It can be hard to recognize the signs and symptoms of a connective tissue disease. But getting a diagnosis and beginning treatment sooner puts you in a better position to manage your condition. Don’t ignore your symptoms, even if they seem unrelated. They could be different effects of the same disease.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
