Sjögren’s syndrome happens when your immune system damages the glands that produce and control moisture in your body. The most common symptom is chronic, unusual dryness in your eyes, mouth or vagina. A healthcare provider will help you find treatments that manage the symptoms and how much they affect your daily routine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
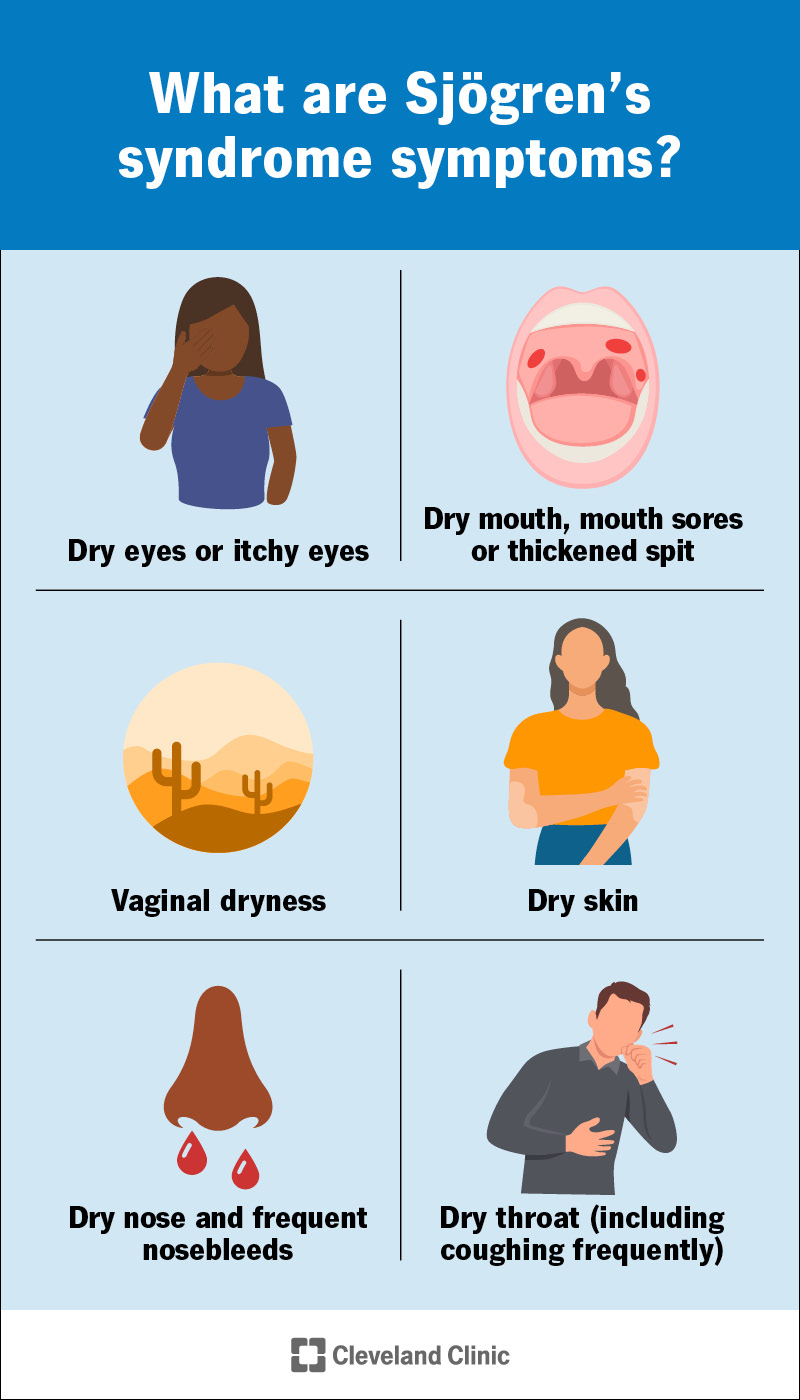
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/sjogrens-syndrome-infographic)
Sjögren’s syndrome is an autoimmune disease that makes your glands produce less moisture than they should. It causes chronic (long-term) dryness throughout your body, especially in your eyes and mouth.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Sjögren’s syndrome is pronounced “SHOW-gren’s syndrome.” Some healthcare providers call it Sjögren’s disease.
If you have Sjögren’s syndrome, your immune system damages glands in your body that produce and control moisture, including in your:
Visit a healthcare provider if you’re experiencing new dryness in your eyes, mouth or anywhere else in your body — especially if you’re also experiencing new pain or other symptoms.
Healthcare providers classify Sjögren’s disease into two types:
Unusual dryness is the most common symptom of Sjögren’s syndrome. You might notice:
In addition to dryness, you might have other symptoms, including:
Advertisement
Sjögren’s syndrome is an autoimmune disease. These happen when your immune system damages your body instead of protecting it. Experts aren’t sure what makes your immune system attack your glands and cause Sjögren’s syndrome.
Primary Sjögren’s syndrome happens with no known trigger or cause.
Other health conditions trigger secondary Sjögren’s syndrome. Autoimmune diseases or viral infections usually cause it.
Any autoimmune disease can lead to secondary Sjögren’s syndrome. Some common triggers include:
Viral infections that can trigger secondary Sjögren’s syndrome include:
Anyone can develop Sjögren’s syndrome. But you may be more likely to if you:
Sjögren’s syndrome can cause some complications, including:
Having Sjögren’s might make you more likely to develop other autoimmune conditions. But that doesn’t mean you definitely will.
Most people with Sjögren’s don’t experience severe complications. You may be more likely to if you have secondary Sjögren’s. Ask your healthcare provider what to expect.
A healthcare provider will diagnose Sjögren’s syndrome with a physical exam and some tests. They’ll examine your body and ask about symptoms you’ve experienced. Tell your provider when you first noticed changes in your body. Let them know if certain times of day or activities make the symptoms worse.
Diagnosing Sjögren’s syndrome is usually part of a differential diagnosis. This means your provider will probably use a few tests to rule out other conditions that cause similar symptoms before diagnosing you with Sjögren’s syndrome. You might need:
You might need to see a few specialists, including:
Advertisement
Your healthcare provider will suggest treatments to manage the symptoms you experience. There’s no cure for Sjögren’s syndrome. But your provider will help you find treatments that reduce how often it affects your day-to-day routine.
The treatments you’ll need vary. It depends on where Sjögren’s syndrome affects you.
Some common treatments include:
Advertisement
Treatments for pain and other symptoms can include:
See a healthcare provider if you notice new symptoms. Tell your provider if the symptoms happen more often or are more severe. Monitor the symptoms and keep track of any changes you notice. You might want to keep a symptom journal. This can help you remember everything you experience.
Your provider will tell you how often you’ll need regular follow-up appointments, tests or additional screenings. Sjögren’s disease symptoms can be subtle. You’re the best judge of when something doesn’t feel quite right in your body. Talk to your provider if you think a treatment isn’t working or isn’t as helpful as it used to be.
Go to the emergency room or call 911 (or your local emergency services number) if you feel like you can’t breathe or swallow.
Advertisement
You should expect to manage symptoms for a long time. Maybe for the rest of your life. But the symptoms should get less severe as you find treatments that work for you. You’ll learn how to manage them. Your healthcare provider will help you find new or different treatments as needed. They may be able to suggest new options or adjust your medications if anything changes.
Sjögren’s syndrome can be extremely annoying to manage. It’s frustrating to have dry eyes, a dry mouth or worry if having sex will hurt because of vaginal dryness. The good news is, you’ll be able to manage the symptoms very well once you find treatments that work for you.
Talk to your healthcare provider about adjusting your treatments if you feel like the symptoms are changing, getting worse or affecting your daily routine more than they should. Ask your provider how often you’ll need eye exams, dental cleaning or other exams and tests. These routine checkups can help you avoid complications.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
