Septic shock is the last and most severe stage of sepsis. Sepsis occurs when your immune system has an extreme reaction to an infection. The inflammation throughout your body can cause dangerously low blood pressure. You need immediate treatment if you have septic shock. Treatment may include antibiotics, oxygen and medication.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
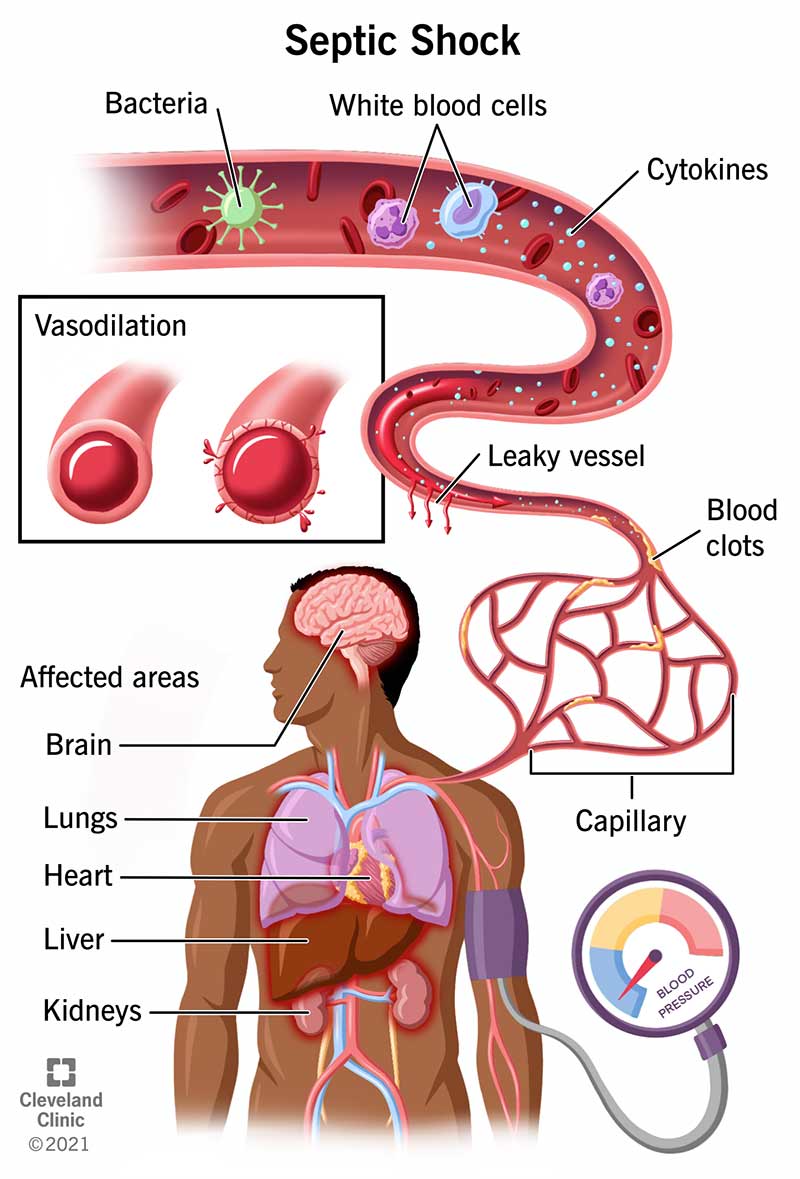
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23255-septic-shock)
Septic shock is a serious medical condition that can occur when an infection in your body causes extremely low blood pressure and organ failure due to sepsis. Septic shock is life-threatening and requires immediate medical treatment. It’s the most severe stage of sepsis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Septic shock is the last and most dangerous stage of sepsis. Sepsis can be divided into three stages: sepsis, severe sepsis and septic shock.
Septic shock is the third stage of sepsis. Early signs of sepsis can include:
When sepsis turns to septic shock, you may experience additional symptoms. These include:
Any infection can lead to sepsis which can then develop into septic shock if it worsens. Not every infection will lead to sepsis or septic shock. But, if an infection causes enough inflammation, it can develop into sepsis. Most of the common infections are from bacteria, but both viruses and fungi can also cause infections and sepsis. Infections can start anywhere but commonly begin in your lungs, bladder or stomach.
Advertisement
Your septic shock risk increases if you have a weakened immune system which increases your risk for sepsis. People with weakened immune systems include:
People with chronic medical conditions have an increased risk of sepsis. These conditions include:
In addition, people who’ve had recent infections, surgeries, transplants or medical devices implanted have an increased risk of sepsis.
Septic shock is a very serious medical condition. It’s the most severe stage of sepsis. Septic shock can lead to:
Your healthcare provider may suspect sepsis if you’ve had an infection and you suddenly develop a fever or hypothermia, rapid heart rate or breathing rate, or low blood pressure.
Your healthcare provider may run blood tests to check for:
Your healthcare provider may also collect samples of your urine, saliva, tissues and/or cerebrospinal fluid for further tests.
In addition, you may have imaging tests to find the source of infection. These imaging tests include:
If you have septic shock, you need immediate treatment. Treatment is usually in an intensive care unit (ICU).
Your healthcare provider will start you on antibiotics immediately. They will also give you fluids through your vein (intravenously) to rehydrate you and help increase your blood pressure.
You may receive oxygen through a face mask or a nasal cannula, a small plastic tube with two openings for your nostrils. A breathing tube may be placed in your windpipe (trachea) to connect you to a breathing machine (ventilator) if you can’t breathe well on your own.
In addition, you may need surgery to remove the source of the infection. Abscesses may be drained. Dead or infected tissue may be removed. Catheters, tubes and medical devices may be removed or changed.
If fluids don’t increase your blood pressure, you may receive medication to raise it. Medications such as vasopressin (Pitressin®) or norepinephrine (Levophed®) cause your blood vessels to narrow and increase the blood flow to your organs.
You may receive insulin if the septic shock has increased your blood sugar (glucose) levels.
Advertisement
If fluids and medication haven’t helped increase your blood pressure, you may receive corticosteroids.
Septic shock is a severe, life-threatening condition. The survival rate is low. Survival depends on your age, health, cause of the condition, if you’ve had organ failure and how quickly you receive treatment. Without treatment, most people will die of septic shock. With treatment, 30% to 40% of people with septic shock die.
Many people recover from septic shock, but it can take a long time. You may continue to have symptoms for months or years. These long-term effects are called post-sepsis syndrome. These effects can include:
To help with your recovery, make sure you:
If you have a bacterial infection, receive treatment right away. Antibiotics can help with the infection and prevent sepsis from occurring, which can lead to septic shock.
It’s also important to keep up to date on your vaccines. Vaccines can help prevent some infections, and they greatly lessen the severity of others. Keep in mind, some cases of septic shock can’t be prevented.
Advertisement
If you develop any symptoms of sepsis or septic shock, you should call 911 or go to the emergency room (ER) immediately.
Septic shock is a severe medical condition. The survival rate is low, but people do survive. Survival depends on your age, health, cause of the condition, if you’ve had organ failure and how quickly you receive treatment. Without treatment, most people die of septic shock. With treatment, 30% to 40% of people with septic shock die.
Sepsis causes septic shock. Bacterial infections are the most common cause of sepsis. The source of the infection can be anywhere in your body. Most often, the infection will start in your lungs, abdomen or urinary tract. In some people, toxins are released by the bacteria and get into your bloodstream. This causes sepsis.
Sepsis can be divided into three stages. The stages are sepsis, severe sepsis and septic shock:
Advertisement
Your healthcare provider may suspect sepsis if you’ve had an infection and you suddenly develop a fever or hypothermia, rapid heart rate or breathing rate, or low blood pressure. Your healthcare provider will run additional tests to confirm the diagnosis.
Septic shock is a severe condition. Be prepared by knowing the signs and symptoms of sepsis and septic shock. If you develop any of the symptoms, call 911 or get to the emergency room ASAP. While septic shock can be a scary diagnosis, immediate treatment is important and could save your life. If you have experienced septic shock, make sure to see your healthcare provider regularly for follow-up visits. They may also be able to provide you with additional resources to help you in your recovery.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Whether you need stitches, a broken bone set or think your appendix might be causing your abdominal pain, Cleveland Clinic’s emergency medicine team is here to help.
