During ERCP, healthcare providers use an endoscope and X-rays to observe injectable dye traveling through your pancreatic and bile ducts. ERCP helps providers identify and diagnose conditions related to your ducts, like gallstones, tumors and strictures. Through the endoscope, they can also treat them during the procedure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
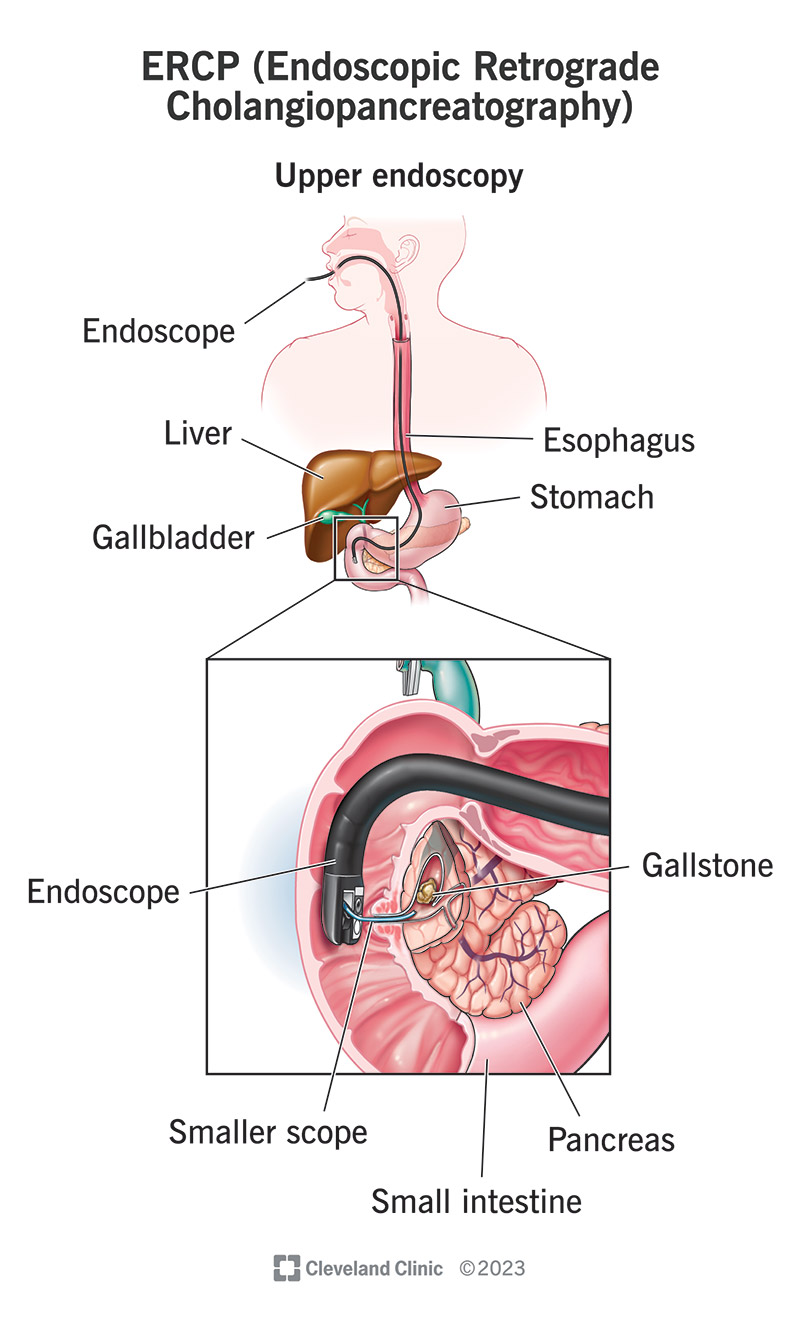
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/4951-ercp)
If your healthcare provider suspects you might have a problem in your biliary system, they might order an ERCP test to look for it. ERCP stands for endoscopic retrograde cholangiopancreatography. It’s a type of imaging test that allows healthcare providers to look inside your bile ducts and pancreatic ducts.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The long name spells out the different types of technology involved in the process. “Endoscopic” refers to endoscopy, which means passing a tiny camera on a tube down your throat and into your small intestine (while you’re under sedation). They pass a smaller tube through the endoscope to reach your bile ducts.
Through this smaller tube, they inject a contrast dye backward into your bile ducts and pancreatic duct. This is what the “retrograde” refers to. “Cholangiopancreatography” refers to the photographs they take. “Cholangio” is “related to the bile ducts,” and “pancreato” is “related to the pancreas.”
Contrast dye helps the insides of your tiny bile ducts and pancreatic ducts show up better in X-rays. This allows healthcare providers to see possible blockages in your ducts — like gallstones, tumors or scar tissue causing narrowing of your ducts. Through the endoscope, providers can also treat these issues on sight.
Your provider might suggest an ERCP if you have symptoms that suggest a problem in your biliary system, such as:
The ERCP procedure can help diagnose and treat common issues affecting your biliary ducts, such as:
Advertisement
ERCP combines endoscopy with fluoroscopy, a type of moving X-ray. Fluoroscopy can help show how well fluids are flowing through your biliary ducts. If fluids are leaking, or if they’re stalling and backing up in your biliary system, your provider will be able to see this and look for the source of the issue.
The endoscope allows your technician (endoscopist) to physically access the site. This is how they inject the contrast dye that helps make fluoroscopy work. It also allows them to treat issues when they find them. Endoscopists can use long, narrow tools to perform minor procedures through an endoscope.
A gastroenterologist typically performs an ERCP. Gastroenterologists are specialists in conditions related to your digestive system, which includes your biliary system. They’re also specialists in performing endoscopies. They train to perform endoscopic procedures that can substitute for minor surgeries.
Your healthcare provider will give you personalized instructions to follow before your procedure. In general, they’ll ask that you:
ERCP is an outpatient procedure, which means you go home the same day. The procedure can take one to two hours. You’ll receive anesthesia through an IV to sedate you. You may or may not be awake, but either way, you probably won’t remember any of it. You’ll need someone to drive you home afterward.
During the diagnostic portion of the ERCP procedure, your provider will:
Advertisement
If your provider finds an issue during the procedure, they’ll do what they can to fix it through the endoscope, using tiny instruments. Your endoscopist may:
After the procedure, you’ll remain at the medical center for an hour or two while the anesthesia wears off. Then your driver can take you home. You’ll be a little groggy or spacey for the rest of the day. You may have some mild discomfort for a day or two after the procedure. Symptoms might include:
Advertisement
Complications occur in approximately 5% to 10% of ERCP procedures. The risks depend partly on your preexisting conditions and what type of therapeutic procedure you have during ERCP. Your gastroenterologist will discuss the potential risks with you in advance. Possible complications include:
If you’re pregnant during the procedure, there’s a low risk of harm to the fetus from the radiation during fluoroscopy. Your doctor will ask you in advance if there’s any chance you’re pregnant. If so, they’ll attempt to reschedule the procedure or minimize your radiation exposure, if necessary.
Advertisement
Your endoscopist should be able to discuss your ERCP procedure with you immediately afterward unless you still feel groggy from the anesthesia. They’ll tell you what they found and what they were able to do to fix it. If they took a tissue sample for biopsy, those results might take a few weeks to come back.
If your ERCP didn’t find anything, you might need a different type of test next. If the procedure wasn’t successful in fixing your issue, or if your biopsy results reveal a new problem, you might need to follow up with a different type of procedure. Your healthcare provider will discuss the next steps with you.
Contact your provider if you experience severe or unusual symptoms after ERCP, such as:
ERCP is an advanced technique in endoscopy. A standard upper endoscopy procedure (esophagogastroduodenoscopy) only goes as far as your upper GI tract. An ERCP uses an extension with the standard endoscope — a second catheter that slides inside the first — to reach your biliary ducts.
This mini endoscope extension allows an endoscopist to operate directly on your ducts. ERCP is the only endoscopic procedure that allows this. While other endoscopic procedures, like MRCP and EUS, can visualize your bile ducts and pancreatic ducts, they don’t provide the same access for treating them.
ERCP isn’t surgery in the traditional sense, which means cutting into your skin to access your organs. ERCP is an endoscopic procedure, which means it goes into your body through a preexisting opening — in this case, your throat. But an endoscopist may operate through the endoscope during an ERCP.
Healthcare providers sometimes refer to operations through an endoscope as endoscopic surgery. These operations are surgical in the sense that they might involve cutting or stitching inside your body. But they’re generally minor procedures, and they involve fewer risks and a shorter recovery than classic surgery.
You might have an ERCP for pancreatitis if your healthcare provider believes that something in your bile ducts or pancreatic ducts is causing it. Gallstones stuck in your ducts are among the most common causes of acute pancreatitis. If this happens to you, you might need ERCP to remove the blockage.
If you have chronic pancreatitis, the inflammation may have caused scarring and stricture in your pancreatic ducts. In this case, you might need ERCP to help stretch them out again or place a stent to prop them open. This helps to ensure that pancreatic juices can keep flowing through the ducts.
Endoscopic retrograde cholangiopancreatography is a diagnostic test that can turn into a therapeutic procedure. While it’s a little more invasive than a standard imaging test, it’s less invasive than a surgical procedure, and it can accomplish both purposes at once. Most people find it tolerable and worthwhile.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Having an endoscopy can be lifesaving. Cleveland Clinic’s providers will help you feel comfortable with the process so you can get the care you need.
