Vasodilation is the medical term for when blood vessels in your body widen, allowing more blood to flow through them and lowering your blood pressure. This process happens normally in your body without you realizing it. It can be caused by things you eat or drink, and medications you take. Vasodilation can also be a symptom of certain diseases.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
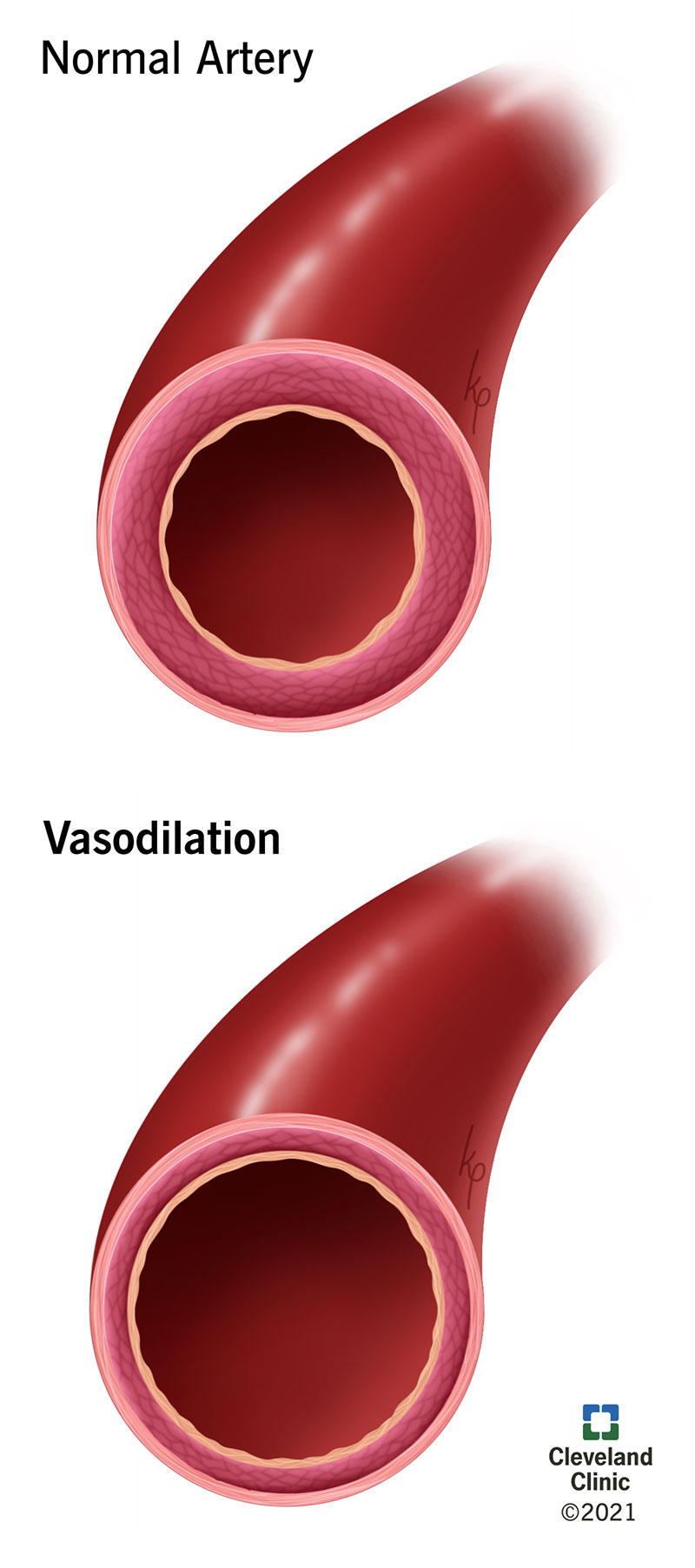
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23352-vasodilation-illustration)
Vasodilation is the medical term for when blood vessels in your body widen, allowing more blood to flow through them and lowering your blood pressure. This is a normal process that happens in your body without you even realizing it. It’s also something that can be caused by things you eat or drink, and medications that you take. Vasodilation can also be a symptom of certain diseases.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your blood has many different purposes in your body, including:
The blood vessels in your body aren’t just tubes that stay the same size all the time. Blood vessels also contain muscle, and that muscle controls just how wide or narrow your blood vessels are at any given time. When blood vessels get wider, that’s vasodilation. The opposite process, when blood vessels constrict and get narrower, is called vasoconstriction.
Vasodilation happens commonly when you:
Advertisement
Yes, there are many things you can eat or drink that can cause vasodilation and, by extension, a decrease in blood pressure.
There’s a wide range of medications that cause vasodilation, either as their main purpose or as a side effect. Many types of blood pressure medications cause vasodilation because that’s their main purpose. Another common medication that causes vasodilation is nitroglycerin, which makes it useful in the treatment of heart attack and chest pain. Erectile dysfunction medications like sildenafil (Viagra®) also rely on vasodilation.
If vasodilation has caused a large drop in blood pressure, this can be treated in multiple ways.
Yes, depending on what causes it, when it happens or how strong the effect is, vasodilation can have negative effects on your body. In extreme cases, vasodilation (and other symptoms associated with it) can be life-threatening.
Examples of life-threatening conditions with vasodilation as a factor include:
Advertisement
For the most part, vasodilation isn’t a cause for concern. In fact, since you can’t see it you may not notice that you have vasodilation. You can see its effects, however. Watch for conditions like fainting, which can be caused by a drop in blood pressure. If there’s a severe drop in blood pressure and shock, it could be life-threatening.
Symptoms of shock may include:
If someone passes out and you suspect that they're in shock, you should do the following:
Advertisement
Vasodilation is a natural process that increases blood flow and decreases blood pressure. Vasodilation is mostly beneficial, as it helps deliver oxygen and nutrients throughout your body. But, vasodilation can be harmful in some cases, leading to severe hypotension (low blood pressure). Be on the lookout for signs of shock, including altered mental state, clammy skin and shallow or rapid breathing. Call your healthcare provider if you or someone you know develops worrisome symptoms.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
