Fournier’s gangrene is a type of flesh-eating disease that affects your genitals or perineum. You’re more likely to get it if you have a penis and scrotum. Symptoms include discoloration, swelling and tenderness. If you have symptoms, get to the emergency room as soon as possible for treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
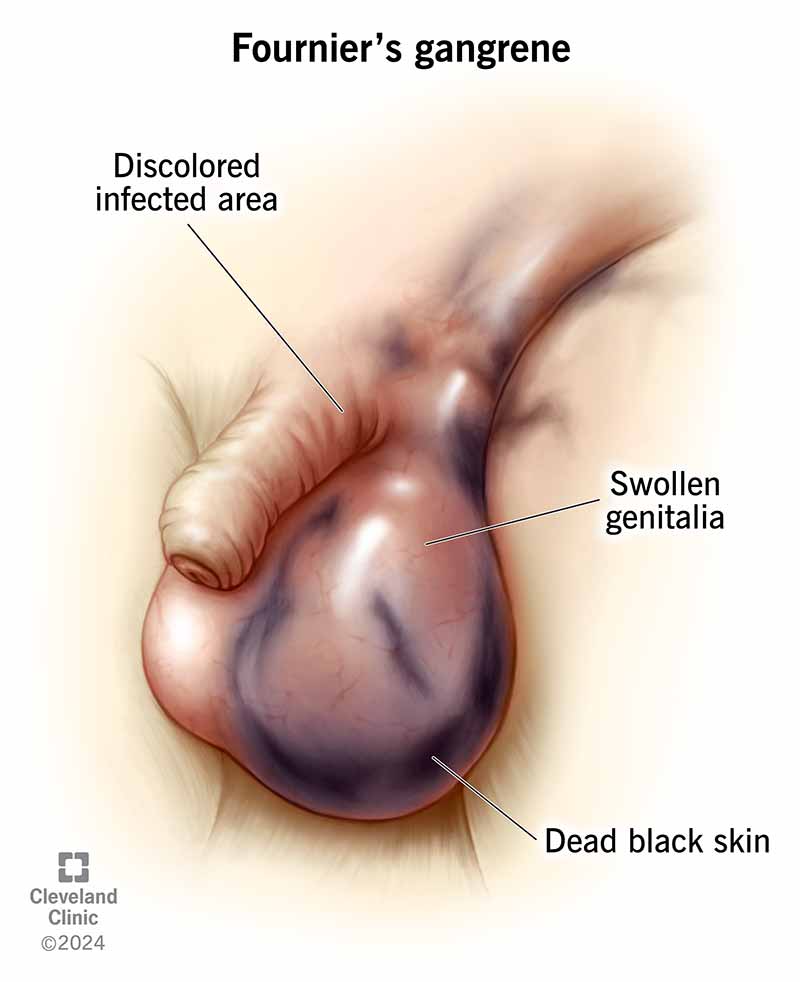
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/fourniers-gangrene)
Fournier’s gangrene (FOR-nee-ayz GANG-green) is a rare, life-threatening bacterial infection of your genitals or surrounding genital areas. It’s a type of necrotizing fasciitis (flesh-eating disease) that worsens quickly and requires emergency care. Necrotizing fasciitis destroys your soft tissues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When bacteria enter your genitals or genital area, they infect your hypodermis (subcutaneous tissue, the deepest layer of your skin) and muscle fascia.
There are arteries within your subcutaneous tissue and muscle fascia. Your pudendal artery takes blood to your:
When bacteria enter the subcutaneous tissue and muscle fascia, they kill the branches of your pudendal artery. When the pudendal arterial tree dies, the bacteria spread further. They travel to the muscles and skin of your genitals and perineum and destroy arteries there, too. From there, they can go through the fascia to other areas of your body, such as your thighs, abdomen and chest.
It’s important to pay attention to the early symptoms of Fournier’s gangrene. By the time the bacteria affect the outer layer of your skin, they have already destroyed the arteries in your subcutaneous tissue and muscle fascia. Fournier’s gangrene gets worse (progresses) quickly. It’s so dangerous that just a few hours can mean the difference between life and death.
Advertisement
Fournier’s gangrene is rare. In the U.S., experts estimate that fewer than 2 out of 100,000 males will get Fournier’s gangrene. It’s even less common in females and children.
Early symptoms of Fournier’s gangrene affect your genitals and perineum. They include:
If you have diabetes, your blood glucose levels might be high, even if you take your insulin as prescribed by a healthcare provider.
You might have other symptoms, as well, including:
Late-stage Fournier’s gangrene symptoms include:
Fournier’s gangrene pain develops suddenly in your genitals and/or perineum. The pain can range from mild to severe.
If you have Fournier’s gangrene, your affected skin will change color. It may look red, purple, brown, blue-gray or black.
Bacteria can enter your genital or rectal areas of your body in several ways. Some examples include:
Anaerobic bacteria or aerobic bacteria can cause Fornier’s gangrene. Anaerobic bacteria can’t live or grow in environments that contain oxygen. Aerobic bacteria can live and grow when oxygen is present.
The most common aerobic bacteria that can cause Fournier’s gangrene include:
The most common anaerobic bacteria that can cause Fournier’s gangrene include:
Anyone at any age can get Fournier’s gangrene. But males are 10 times more likely to get it than females.
You’re at a higher risk of developing Fournier’s gangrene if you have any of the following conditions:
You’re also at a higher risk of Fournier’s gangrene if:
Advertisement
Fournier’s gangrene complications may include:
Fournier’s gangrene may also cause death.
A healthcare provider will review your medical history, ask about your symptoms and examine your skin. If there’s time, they’ll likely order imaging tests.
Often, there’s no time for tests. You may need immediate surgery if Fournier’s gangrene progresses to a dangerous point. But if there’s time, a healthcare provider may order the following imaging tests:
Advertisement
Surgery is the best treatment for Fournier’s gangrene. It’s often necessary to skip the diagnosis process and immediately surgically remove the damaged tissues (debridement). This often leaves a large wound. Many people with Fournier’s gangrene need many surgeries to remove dead tissue. They also need daily or twice-daily dressing changes on the wound. You may also need:
After surgery, healthcare providers will likely prescribe antibiotics that target many different types of bacteria (broad-spectrum antibiotics). If you also have sepsis, you’ll receive anticoagulants (blood thinners) to reduce your risk of developing blood clots.
After the surgeon removes the damaged tissues, you’ll likely need reconstructive surgery to help restore the appearance and function of your affected genital tissues. This happens after providers treat the infection and the wound is clean.
Finally, you may need hyperbaric oxygen therapy (HBOT). During HBOT, you enter a pressured chamber that fills with 100% oxygen. Extra air pressure helps your body absorb more oxygen. The oxygen helps:
Advertisement
Rarely, a surgeon will have to remove your entire penis, scrotum or labia.
No, there aren’t any at-home treatments for Fournier’s gangrene. If you have Fournier’s gangrene symptoms, go to the emergency room. You need surgery and antibiotics as soon as possible.
Your body is unique, and how long it takes you to recover from Fournier’s gangrene may be different from others. You may be in the hospital from three to six weeks. A healthcare provider will give you a better idea of what to expect.
Go to the emergency room if:
The sooner you get treatment, the greater chance you have of recovering.
You may also wish to ask a healthcare provider the following questions:
Fournier’s gangrene is life-threatening. Your outlook depends on many factors, including how quickly you see a healthcare provider and the amount of dead or infected tissue. Fournier’s gangrene affects more and more tissue the longer you wait to get care. It’s important to get treatment right away to prevent serious and fatal complications.
Most people must stay in a hospital for at least three weeks to treat Fournier’s gangrene. You’ll likely need to spend even more time at home to recover. A healthcare provider will give you a better idea of when you can expect to return to work or school. Recovery can be a long process.
Staying healthy and managing other medical problems, like diabetes or substance use disorders, are the best ways to prevent Fournier’s gangrene. You can help reduce your risk of bad complications by regularly checking your genitals for signs of infection, including discoloration, swelling and tenderness.
You may also be able to reduce your risk by:
Improving your blood flow may also help reduce your risk. You can help improve your blood flow by:
Yes, it’s possible that your hygiene habits can increase your risk of Fournier’s gangrene. Not regularly and thoroughly cleaning your genitals and the surrounding area with soap and clean water can increase your chances of developing Fournier’s gangrene.
In rare cases, insect (bug) bites or stings can cause Fournier’s gangrene. Ant bites were responsible for one reported case. Healthcare providers have reported that spider and tick bites are responsible for causing gangrene in other parts of your body.
You have a higher chance of getting Fournier’s gangrene if you take sodium-glucose cotransporter-2 (SGLT2) inhibitors to manage Type 2 diabetes. Examples of these inhibitors include:
It’s important to remember that Fournier’s gangrene is rare. Very few people who have diabetes get it.
No, Fournier’s gangrene isn’t a sexually transmitted infection (STI). You won’t get this infection from anyone else, and they won’t get it from you.
Yes, Fournier’s gangrene is an emergency. Fournier’s gangrene is fatal in just under 30% of people who have it. Go to the emergency room as quickly as possible if you have symptoms of Fournier’s gangrene.
Go to the emergency room if:
The condition got its name from Jean Alfred Fournier, a French physician who first identified it. Gangrene is a condition that causes your tissues to die because of a bacterial infection.
Looking at Fournier’s gangrene symptoms and its treatments would frighten anyone. But remember — it’s a very rare type of necrotizing fasciitis. Fewer than 2 out of every 100,000 males get it, and it’s even less common in females. You can help reduce your chances of developing Fournier’s gangrene by regularly checking for symptoms and keeping the area clean. If you have any symptoms, make sure to have a healthcare provider check you out right away.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you need stitches, a broken bone set or think your appendix might be causing your abdominal pain, Cleveland Clinic’s emergency medicine team is here to help.
