Your perineum is the thin layer of skin between your genitals (vaginal opening or scrotum) and anus. Inside your body, your perineum consists of tissue that makes up the bottom of your pelvic cavity. It’s a common site for tears during childbirth. Minor tears may heal on their own, while major ones may require stitches.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your perineum is the tiny patch of sensitive skin between your genitals (vaginal opening or scrotum) and anus, and it’s also the bottom region of your pelvic cavity. The perineum may refer to just the part of your body you can see (the skin in between your genitals and your anus). Perineum may also refer to the underlying structures inside your body beneath your pelvic floor.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The perineum is the small patch of flesh located between your vaginal opening and anus.
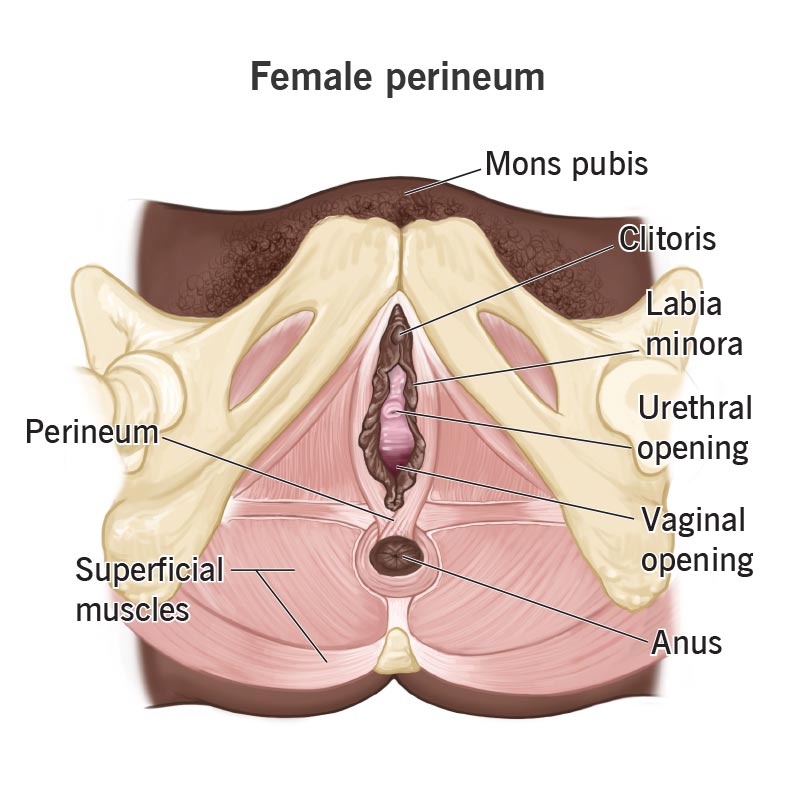
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24381-perineum-female.jpg)
The perineum is the small patch of flesh located between your penis and anus.
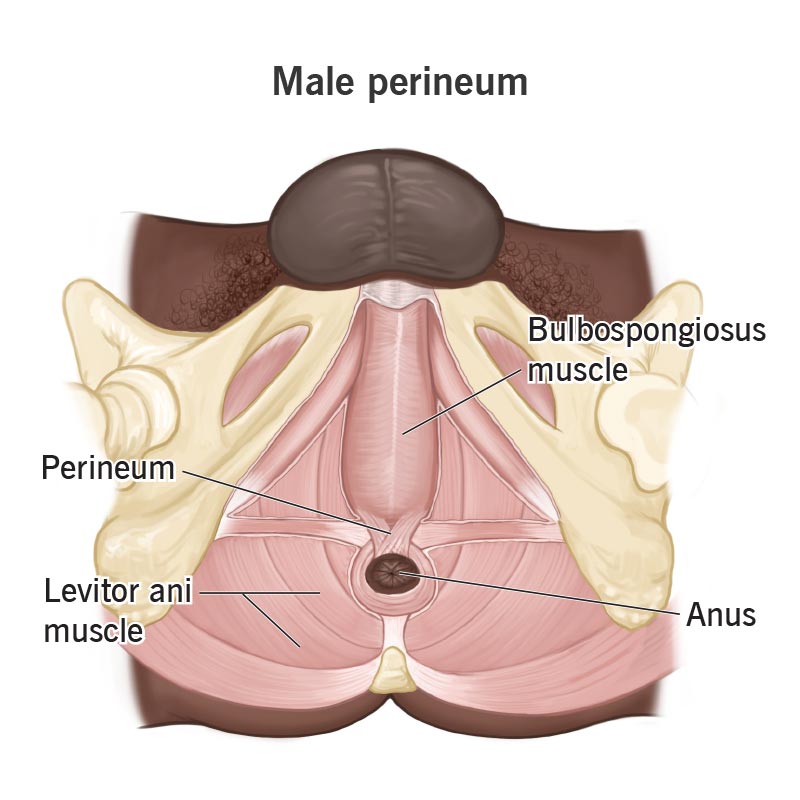
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24381-perineum-male.jpg)
Your perineum is an erogenous zone. The skin covering your perineum contains multiple nerve endings that help with sexual arousal and response.
Inside your body, your perineum contains structures that help you pee, poop and have intercourse. If you’re female, your perineum contains structures that help you give birth vaginally. Your perineum forms a foundation that helps support your pelvic floor muscles, which hold organs like your bladder, colon and reproductive organs in place.
Your perineum is between your genitals and your anus. This part of your perineum that you can see corresponds with structures inside your body that you can’t see. Internally, your perineum is located below the primary muscle of your pelvic floor (levator ani), and it stretches across your pelvic bones.
Advertisement
Diagrams sometimes show the perineum’s boundaries as diamond-shaped, with an imaginary line drawn from one sitz bone in your pelvis to the other. This imaginary line divides the diamond into two triangle-shaped regions: the urogenital triangle and the anal triangle.
A tough mass of fibromuscular tissue called the perineal body is located where your urogenital and anal triangles meet. It plays a significant role in supporting your pelvic floor and injures easily during childbirth.
The average perineum is about 1.5 inches (in) long if you’re female. It’s about 2 inches or more if you’re male.
Underneath your perineum’s skin are multiple layers of connective tissue, fatty tissue, muscles and membranes. An important nerve called the pudendal nerve runs through your perineum and branches out into various parts of your anatomy, including your genitals, pelvic floor muscles and anus. This complex nerve network makes your perineum sensitive to sexual sensations and helps you pee and poop.
Childbirth is the most common cause of injury to your perineum. About 85% of people who give birth vaginally experience a torn perineum. Still, you can injure your perineum regardless of your sex.
Advertisement
Advertisement
Pain is the most common sign that something’s wrong with your perineum. After childbirth, you may experience pain from a torn perineum that makes it difficult to walk or sit.
Other symptoms may signal an issue with your perineum or a condition affecting the surrounding muscles or organs in your pelvic cavity, including:
Your provider can check for an injury, infection or other condition that’s affecting your perineum by doing a physical exam. The exam may include a digital rectal exam, where your provider places a gloved finger into your rectum to feel for any irregularities.
Imaging procedures can help your provider diagnose problems affecting your perineum:
Advertisement
Your provider can assess any cuts or tears on your perineum to determine whether you need stitches to repair your injury. In the meantime, pain management strategies can ease your symptoms as you heal.
Your provider may prescribe antibiotics or incise (cut) and drain an infected cyst. You may need surgery if you have severe hemorrhoids or nerve damage in your perineum.
You can’t prevent your perineum from tearing, but massaging it before childbirth and during delivery reduces the likelihood that it will tear.
Begin massaging your perineum around week 34 of your pregnancy.
Set aside massage sessions that last for five minutes. Plan to massage your perineum three to four times a week.
Carve out a time and space for massaging your perineum that allows you to feel as relaxed as possible. Before you begin, wash your hands with a mild soap to prevent bacteria from entering your vagina.
Your perineum includes the delicate portion of skin between your genitals and anus and the underlying tissues that make up the bottom part of your pelvic cavity. It plays an important role in the structural integrity of your pelvis. That said, don’t be alarmed if your perineum tears during childbirth. Your tear may require stitches, but most injuries heal in time. Your healthcare provider can recommend pain management strategies that ease your symptoms as you heal.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
