Dysautonomia is a nervous system disorder that disrupts autonomic body processes. These are automatic functions like your blood pressure and heart rate. Having dysautonomia means these functions don’t work properly, causing disruptive symptoms. These symptoms are often manageable, but diagnosing and treating dysautonomia is sometimes difficult.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Dysautonomia” is the general term for disorders that disrupt your autonomic nervous system (ANS). It can describe several disorders, each with varying symptoms. Dysautonomia can range from mild to severe. Other less common names for dysautonomia are autonomic dysfunction or autonomic neuropathy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your ANS is a subdivision of your nervous system. The term “autonomic” means ”self-governing,” and the ANS manages all of your body system processes you don’t think about. That includes your blood pressure, body temperature, breathing, digestion, heart rate, sweating and much more.
If you have dysautonomia, one or more of these ANS processes aren’t working as they should. As your ANS does so many things for you, dysautonomia can cause a lot of different symptoms. These include, but aren’t limited to, chest pain, mood swings, fainting, fatigue and dizziness.
Various forms of dysautonomia are relatively common. More than 70 million people worldwide have some form of it. It can be congenital (meaning it’s something you have at birth), or you can develop it at any point in life. The average time of onset is between the ages of 50 and 60.
Dysautonomia is often something that healthcare providers have limited experience with, though. That’s because the condition can vary widely and take many forms. Dysautonomia is often a complicated condition to detect, diagnose and treat.
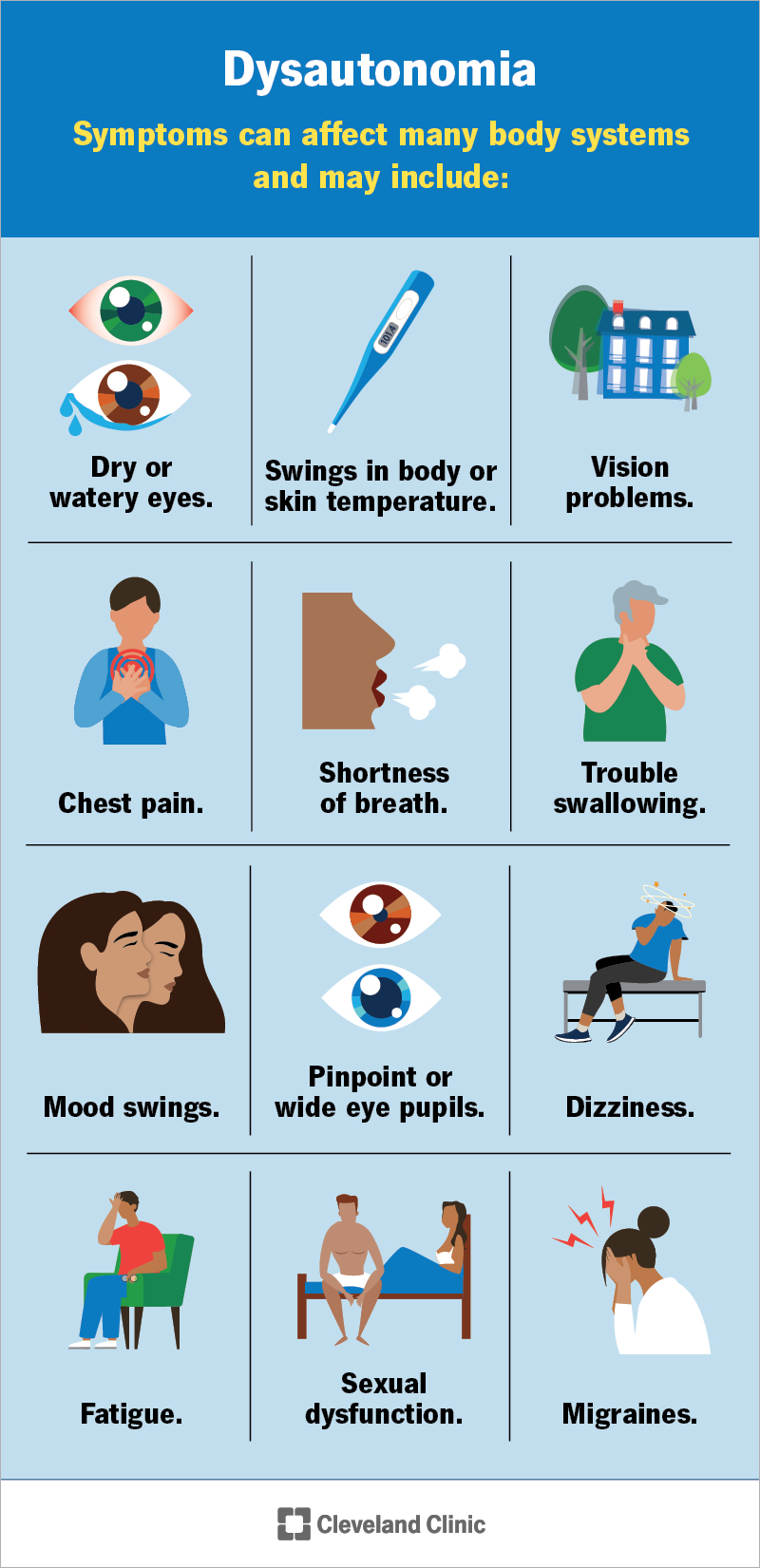
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/6004-dysautonomia)
Symptoms of dysautonomia can affect many body systems, and they may look different depending on the system they affect, like:
Advertisement
There are two main types of dysautonomia, primary and secondary:
Primary dysautonomias happens on their own, without a specific cause. They aren’t as common as secondary dysautonomia (secondary means something else is causing it).
A specific example of a primary type is an inherited form called familial dysautonomia. Any of the following can increase your odds of having it:
Another primary form is “idiopathic” dysautonomia, which means it happens for a reason that healthcare providers can’t explain or detect.
There are conditions that can cause or contribute to dysautonomia. Some examples include (but aren’t limited to):
Advertisement
Because dysautonomia affects vital body processes, there are many possible complications. Most of the complications revolve around symptoms of dysautonomia, especially when they’re severe or disrupt your usual routine and activities.
Serious symptoms and complications generally include:
Your healthcare provider is the best person to tell you more about the possible complications you might experience and how to avoid them or limit their effects.
A healthcare provider can diagnose dysautonomia using a combination of methods and tests. Diagnosing dysautonomia is often partly a process of elimination. It also involves determining how and when symptoms happen and finding the pattern that links them.
But even experienced providers may find dysautonomia challenging to diagnose. That’s because dysautonomia can cause symptoms throughout your body that might not seem connected. Providers may also link symptoms to whatever condition is causing dysautonomia but not realize dysautonomia is also happening.
Advertisement
Some of the tests that may help with diagnosing dysautonomia (or rule out other conditions) include:
Many other tests are possible, depending on your symptoms. Your healthcare provider can tell you more about tests that may help.
There’s no cure for dysautonomia, but many symptoms are manageable. The treatment approach for dysautonomia depends strongly on many factors, especially what’s causing it.
Some treatment approaches that might help include:
Advertisement
When dysautonomia occurs because of a medication or medical treatment, stopping that medication or reversing that treatment is usually a priority.
Because there are so many possible treatments for dysautonomia, your healthcare provider is the best source of information about treatment options. They can provide details that are most relevant to your situation and needs. They can also tell you about possible side effects and complications to watch for and what you can do to limit or avoid those.
Dysautonomia can look very different from person to person, even among family members. Your symptoms may be totally different from someone else’s. Your symptoms and how they impact your life can also vary widely.
Many people with dysautonomia may experience difficulties with getting a diagnosis. You’re not alone if you experience frustration, anxiety or other difficult emotions surrounding your symptoms. These feelings are common for those with dysautonomia.
Some forms of dysautonomia may be temporary, but it’s usually a lifelong condition.
Dysautonomia is an unpredictable condition. Some people may experience frequent symptoms. Others may go months or even years without any. It’s difficult to predict what your life will look like living with dysautonomia, but your healthcare provider can help you understand what’s possible or likely and what you can do to limit the impact on your life.
Depending on the cause, dysautonomia may be a minor concern. But some forms or causes — especially chronic or incurable conditions — may have larger impacts. In severe cases, the symptoms may affect your ability to work or participate in activities you enjoy. This condition may also cause deadly complications.
Dysautonomia happens unpredictably and for reasons experts don’t yet understand. It isn’t possible to prevent it or lower your risk of having it.
Dysautonomia is a complex condition. Many people with it struggle to find a provider who can diagnose and treat it. Many may experience frustration or anxiety surrounding medical care because they don’t know what’s causing their symptoms, and healthcare providers can’t find an explanation for why the symptoms happen.
If you’re having symptoms of dysautonomia and experience these feelings, you’re far from alone. You can also take proactive steps to help yourself get a diagnosis and treatment. Some things you can do include:
Your healthcare provider will likely recommend certain changes to what you eat and drink if you have dysautonomia. The recommendations often include (but aren’t limited to):
Your healthcare provider will likely recommend a regular schedule for follow-up visits. Those visits are important even if nothing seems to have changed. They can help your provider track your symptoms (even if they haven't changed). Your provider can also check vital signs you can’t feel that are important indicators for dysautonomia, like your blood pressure.
You should also call or see your provider if:
Dysautonomia can cause many serious symptoms, especially ones related to your blood pressure. Lightheadedness and dizziness often reverse themselves if you sit or lie down (this makes it easier for blood flow to reach your brain). Most people will also regain consciousness after fainting for the same reason.
But some symptoms are difficult to tell apart from a medical emergency. You should always call 911 or your local emergency services number when in doubt. Symptoms that need emergency attention can include (but aren’t limited to):
There are other symptoms you may need to watch for. Your healthcare provider can advise you which symptoms mean you need medical attention.
Some of the questions you may want to ask your healthcare provider include:
Dysautonomia can have triggers that make symptoms happen suddenly or worsen. Knowing and tracking your triggers (especially with a journal/diary) can help you learn and avoid them. Common triggers can include (but aren’t limited to):
You might have other triggers not listed here. If you think you might have a trigger but aren’t sure, tell your healthcare provider about your concern. They may be able to suggest a test or method to check.
Dysautonomia can be frustrating, especially when you don’t know what it is or why it’s happening. For some people, getting a diagnosis may take months or even years. Though challenging to diagnose and treat, many people can manage their symptoms and live their lives with limited disruptions.
If you suspect you have dysautonomia, a healthcare provider can review your symptoms with you and help you find a specialist with experience in treating this condition. That way, you can go about your day, limiting the effect of your symptoms and focusing on the things that matter to you.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
