Guillain-Barré syndrome (GBS) is a rare condition that causes sudden numbness and muscle weakness that can affect most of your body. It happens when your immune system responds abnormally and attacks your peripheral nerves. Most people make a full recovery from GBS with treatment and rehabilitation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Guillain-Barré syndrome (pronounced “ghee-AHN buh-RAY”) is a rare autoimmune condition in which your immune system attacks your peripheral nerves. It leads to symptoms like numbness, tingling and muscle weakness that can progress to paralysis. But with treatment, most people fully recover from the condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Guillain-Barré syndrome (GBS) can occur at any age, but it most commonly affects people between 30 and 50.
Guillain-Barré syndrome is rare. About 100,000 people worldwide develop GBS every year. To put that into perspective, the world population is about 7.8 billion. That means healthcare providers diagnose GBS in about 1 in 78,000 people each year.
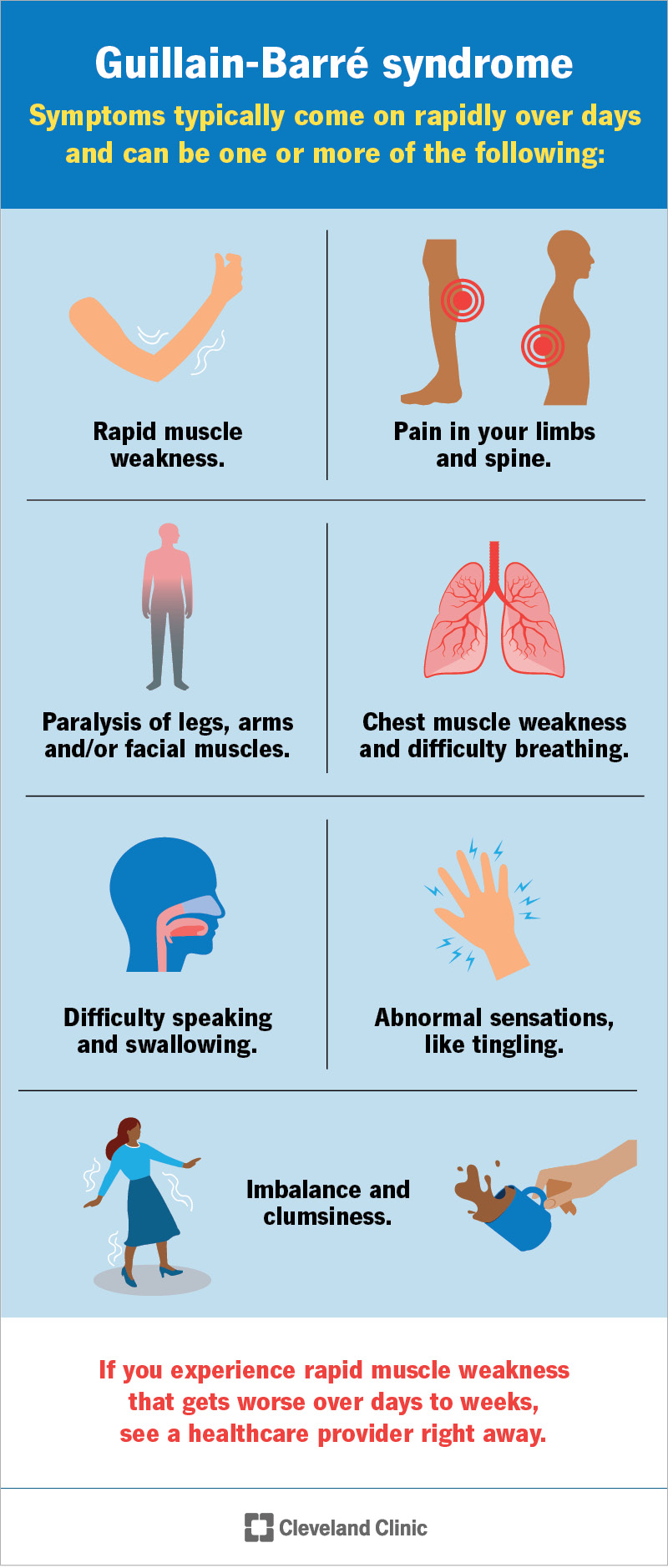
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15838-guillain-barre-syndrome)
Guillain-Barré syndrome affects your peripheral nerves, which control muscle movement, pain signals, and temperature and touch sensations. Thus, GBS causes issues related to these functions.
The first symptoms of Guillain-Barré syndrome are muscle weakness and/or tingling sensations (paresthesia). These symptoms typically come on suddenly. They usually affect both sides of your body and start in your feet and legs and spread up to your arms and face. Muscle weakness in your legs may make it difficult to walk or climb stairs.
The severity of GBS can range from very mild to severe. Depending on the severity of the condition, other symptoms may include:
Advertisement
The symptoms of GBS can progress over hours, days or a few weeks. Most people reach the most severe stage of weakness within the first two weeks after symptoms appear. By the third week, about 90% of people are at their weakest.
If you experience sudden muscle weakness that gets worse over hours or days, see a healthcare provider right away. It’s important to start treatment for GBS as soon as possible.
If GBS affects your autonomic nerves, it can lead to life-threatening complications. Your autonomic nervous system controls the automatic functions of your body that you need to survive, like your heart rate, blood pressure and digestion. When you have issues with this system, it’s called dysautonomia.
Complications due to GBS-related dysautonomia can include:
Guillain-Barré syndrome is a post-infectious, immune-mediated neuropathy. This means:
Researchers have identified some infections and other immune system-related factors that can trigger Guillain-Barré syndrome, including:
Healthcare providers typically diagnose Guillain-Barré syndrome based on your symptoms and medical history. They’ll ask how and when your symptoms started and if you’ve been sick recently. They’ll also do physical and neurological exams to look for signs of muscle weakness and weak or absent deep-tendon reflexes (hyporeflexia or areflexia).
Advertisement
However, many other neurological conditions share the same symptoms as GBS. So, your provider will likely do other tests to rule out other possible conditions. These tests may include:
If you have Guillain-Barré syndrome, you’ll likely need to receive medical care in a hospital’s intensive care unit (ICU). This is so your healthcare team can monitor you for any complications of GBS, like difficulty breathing or blood pressure fluctuations.
There’s no known cure for Guillain-Barré syndrome. But some therapies can lessen the severity of the condition and shorten your recovery time. The main treatment for GBS includes one of two options:
Advertisement
Both of these treatments usually shorten your recovery time if you start one of them within two weeks of developing GBS symptoms.
Complications of GBS can develop if the condition affects your autonomic nerves, causing near-total paralysis. Your healthcare team will carefully monitor your breathing, heart rate and blood pressure. They’ll act quickly if any complications develop. Examples of treatments for complications include:
Advertisement
As you begin to improve, your healthcare team may transfer you to a rehabilitation setting. Here, you’ll work with physical therapists and other therapists to regain strength and resume activities of daily living. Types of therapy include:
The prognosis (outlook) for Guillain-Barré syndrome can vary. Most people with GBS improve considerably over a period of months. But about 30% of adults — and even more children — have some remaining muscle weakness three years after diagnosis.
In the majority of cases, the symptoms of Guillain-Barré syndrome improve significantly with time and treatment. Most people start to recover two to three weeks after symptoms first start. The length of total recovery can vary from months to a year or more depending on the severity.
People who recover from Guillain-Barrésyndrome have a normal life expectancy. Less than 2% of people die from GBS in the acute phase — when symptoms are at their worst. Common causes of death related to GBS include:
In most cases, Guillain-Barré syndrome isn’t preventable. Researchers don’t know why some people develop GBS after they get sick and others don’t. But one way you can try to lower your risk of GBS is to stay as healthy as possible. These steps can help:
The recovery process for Guillain-Barré syndrome can be slow for some. Don’t hesitate to lean on loved ones for support — both physically and emotionally. Your healthcare team will also be by your side.
Suddenly and unexpectedly developing weakness or paralysis can be overwhelming. Consider talking to a mental health professional, like a psychologist, if GBS is causing distress. A support group may also help you relate to others who are going through similar experiences and feelings.
Guillain-Barré syndrome (GBS) is a serious condition that can turn your health on a dime. The good news is that most people with GBS recover well with treatment. But this can take time. And the recovery process can be daunting and exhausting. Know that your healthcare team will be with you every bit of the way. Be sure to lean on loved ones for support, too.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your body starts attacking your nerves, you’ll want the best care. Cleveland Clinic is here to treat rare neurological conditions like Guillain-Barré syndrome.
