Your pericardium is a fluid-filled sac that surrounds your heart and the roots of the major blood vessels that extend from your heart. Conditions that affect your pericardium include pericarditis, pericardial effusion and constrictive pericarditis. Symptoms of pericardial problems include chest pain, shortness of breath and heart palpitations.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your pericardium is a protective, fluid-filled sac that surrounds your heart and helps it function properly.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your pericardium also covers the roots of your major blood vessels as they extend from your heart. These are known as your “great vessels,” and they include your:
Your pericardium has several important functions. These include:
Your pericardium is located in your chest, where it surrounds your heart. Your heart is located in the front of your chest, slightly to the left of your breastbone (sternum). If you have dextrocardia, your heart is slightly to the right of your breastbone.
Your pericardium has two main layers:
Advertisement
Your serous pericardium is made of two layers:
Your pericardial cavity is the space between the two layers of your serous pericardium. This space holds your pericardial fluid.
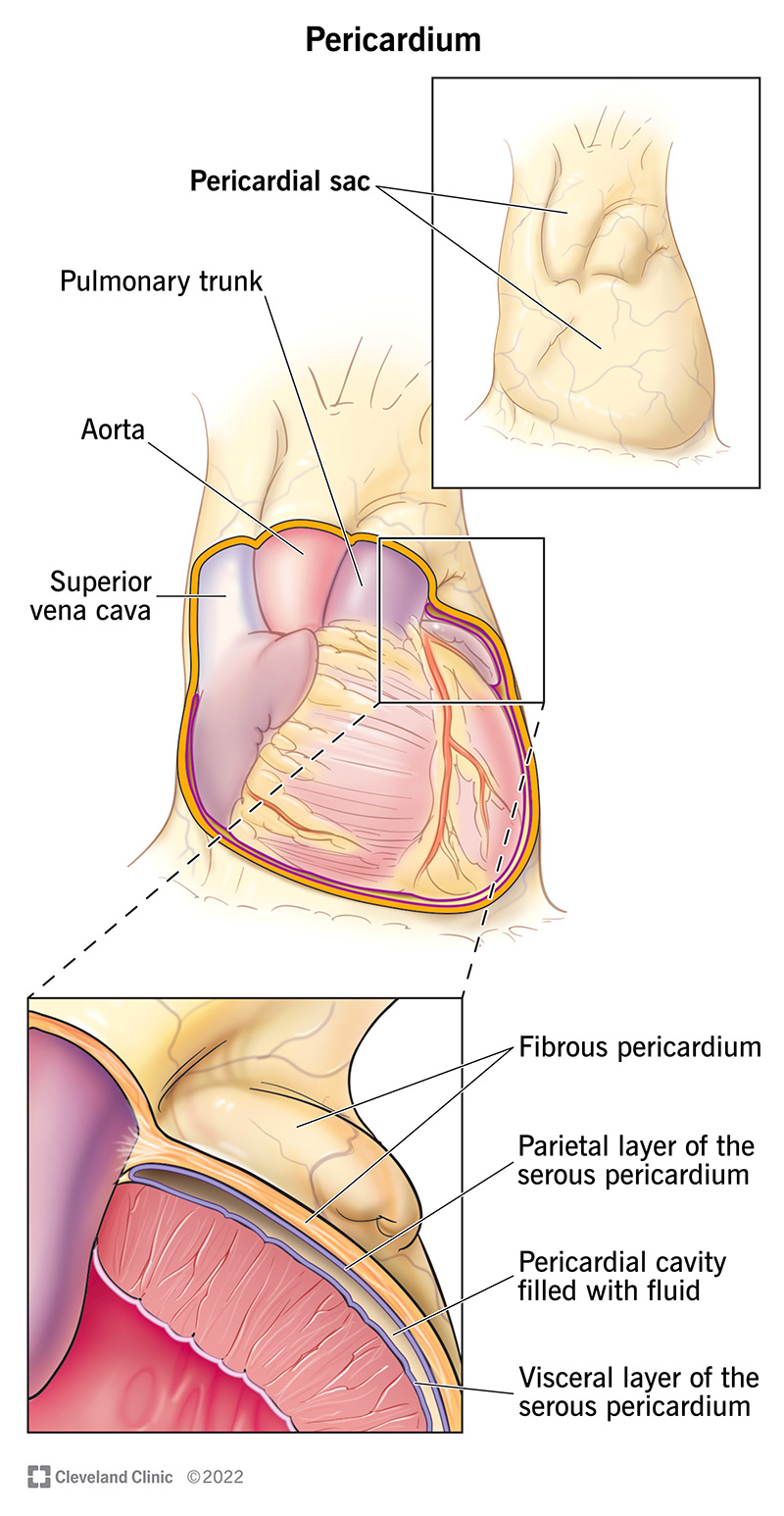
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23561-pericardium)
Conditions and disorders that affect the pericardium include:
Normally, your pericardium is flexible and stretchy. It can easily expand with the heart as the heart fills up with blood and then contracts to pump the blood out to your body. Pericardial conditions and disorders prevent your heart from expanding as it should. As a result, your heart can’t fill and pump blood efficiently to the rest of your body. This can lead to dangerous complications, including heart failure and cardiogenic shock.
Symptoms depend on the specific condition but generally can include:
Your provider may run one or more of the following tests to diagnose pericardial problems:
Treatment depends on your condition and its severity. Your provider will talk with you about your treatment options and the urgency of your situation. Some common options include:
Advertisement
Following a heart-healthy lifestyle is one of the best things you can do. Conditions like heart attacks and heart failure can cause pericarditis and pericardial effusion. So, lowering your risk of those conditions can help you keep your pericardium healthy, too.
Tips for following a heart-healthy lifestyle include:
Other medical conditions and diseases can cause pericardial problems. If you have any of these diagnoses, talk with your provider about how they might affect your heart:
Certain medical procedures and treatments can also cause pericardial problems. Talk with your provider about your risk for pericardial issues after:
In general, do as much as you can to be an active partner in your medical care. Talk with your provider about your risks for cardiovascular disease and how you can reduce them.
Advertisement
Your pericardium is one part of the complex organ known as your heart. You don’t need to learn every detail about your heart anatomy. But learning the basics about your heart and how it works can help you talk with your provider and understand any diagnosis you might receive. This knowledge can also help you navigate treatment plans and make decisions for yourself and your loved ones.
If you have concerns about your pericardium or your overall heart health, call your provider. And don’t hesitate to ask for resources to help you learn more.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether your pericardial disease comes on acutely without warning or is chronic, Cleveland Clinic has the best treatments for this heart condition.
