Cardiac tamponade describes a heart that has so much fluid around it that it can’t pump enough blood. The force of this fluid makes it hard for your heart to do its job. This is a medical emergency. A healthcare provider has to remove the extra fluid with a needle or surgery. You need quick treatment for a good outcome.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
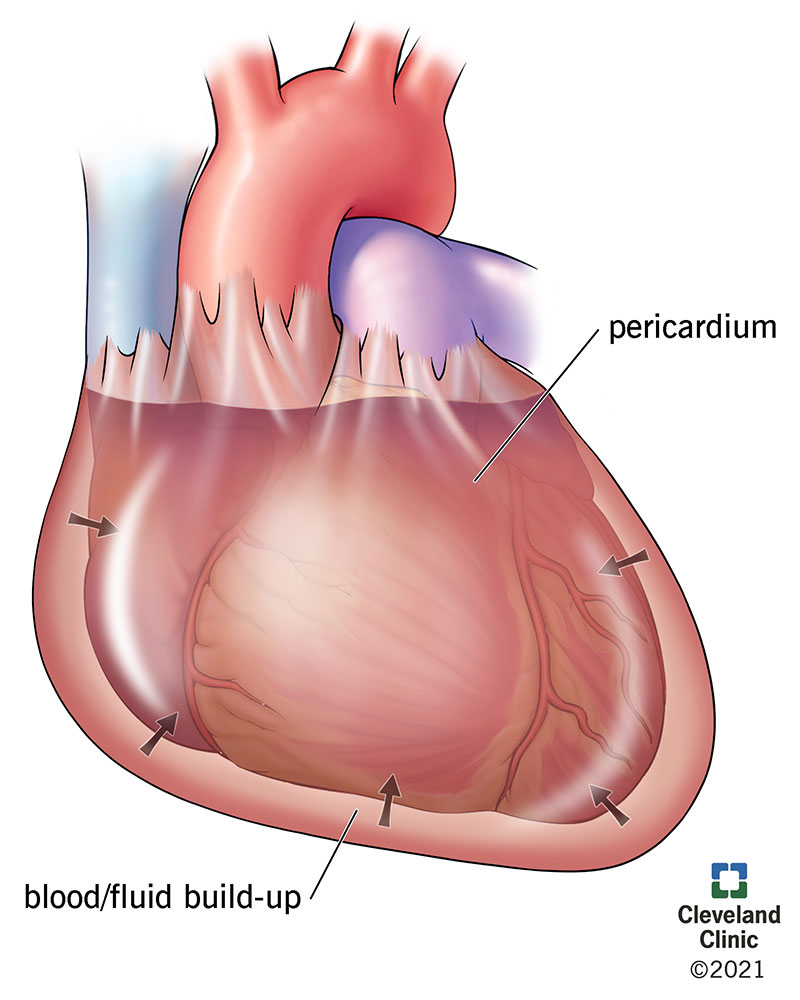
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21906-cardiac-tamponade-illustration-01)
Cardiac tamponade happens when the fluid sac around your heart fills with too much blood or other fluid and puts pressure on your heart. This prevents your heart’s chambers from filling properly.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When your heart can’t fill with blood properly, it can’t pump as much and your blood pressure drops. Your heart may beat faster (more than 100 beats per minute) to try to pump more blood.
Cancer, infections, trauma and certain diseases can cause cardiac tamponade. Without treatment, it’s life-threatening.
Inside your chest, a sac called the pericardium surrounds your heart. The pericardium has two layers and pericardial fluid that holds your heart in place.
Cardiac tamponade — or pericardial tamponade — happens when the pericardium fills with fluid (usually pericardial fluid or blood). Because the fluid has nowhere to go, your heart runs out of room and can’t expand enough to fill effectively.
Pericardial effusion is the technical term for when the pericardium is filling up with fluid. Effusions can consist of blood, discharge and other blood component products. A pericardial effusion doesn’t always cause cardiac tamponade, especially when the fluid builds up slowly over time. This is because it has time to stretch and make more room for fluid, and the process may not cause symptoms. Cardiac tamponade is when pressure from surrounding fluid keeps your heart from beating properly.
Advertisement
This condition can happen to people of all ages. About 2 out of every 10,000 people get cardiac tamponade from other diseases.
When this condition happens quickly, cardiac tamponade symptoms may include:
When the condition happens more slowly, you may also have these cardiac tamponade symptoms:
Cardiac tamponade causes include:
In some cases, cardiac tamponade can also happen after a medical procedure. Some of these include:
Fluid is more likely to build up in your pericardium if you have:
Cardiac tamponade complications can include:
Cardiac tamponade is dangerous because it ultimately limits the amount of blood your heart can pump (cardiac output). This deprives your body of blood and oxygen. Eventually, it can cause your heart to stop entirely, a potentially fatal condition called cardiac arrest.
Several different tests and methods can help diagnose cardiac tamponade. Healthcare providers are most likely to start with a physical exam. This will include:
Advertisement
Hallmark cardiac tamponade signs are those known as Beck’s triad:
However, only 10% to 40% of people with cardiac tamponade have Beck’s triad.
Tests to diagnose cardiac tamponade include:
Treatment for cardiac tamponade requires removing the fluid from around your heart with a procedure called pericardiocentesis. A provider may also need to repair damage related to the fluid buildup.
Cardiac tamponade treatment may include using a needle (pericardiocentesis) or performing surgery.
Surgery may be a better option if:
In especially severe cases, such as when your heart stops because of cardiac tamponade, a provider can do a thoracotomy by the bedside in the emergency room (ER).
Your provider will need to treat the cause of your cardiac tamponade, as well. Depending on what caused your cardiac tamponade and which treatment you had, you may receive pain medications, antibiotics or other medications.
Advertisement
Pericardiocentesis and surgery can have the following complications:
You should feel better right away when a provider removes the excess fluid from your pericardium. You may have a drainage tube for a day or two so the fluid can keep draining. Echocardiograms can show how much fluid is left in your pericardium. This helps your provider decide when it’s time to remove the drain.
Your healthcare provider can give you guidance on what you should and shouldn’t do while you’re recovering from cardiac tamponade and any procedure that treats it. If you had surgery, it’s likely that your provider will tell you to avoid physical activity during the healing process.
If a disease is what caused your cardiac tamponade, how you manage it will change depending on your situation. Your provider can guide you on what you can and should do once you go home.
If you get quick treatment for cardiac tamponade, you’ll probably have a good outlook. Your prognosis gets worse with a delay in treatment.
Advertisement
Because either diseases or injuries can cause it, cardiac tamponade is extremely difficult to predict and prevent. However, it may be possible to avoid it with early detection and treatment of a pericardial effusion, especially after an injury or with conditions that you know you have.
When you go home from the hospital after cardiac tamponade treatment, keep taking medicines your provider prescribed for you. Going to follow-up appointments is important, too. Cardiac tamponade can happen more than once. A provider can keep an eye on the condition that caused it.
You should have another echocardiogram about one or two weeks after your cardiac tamponade treatment. You’ll also need to have a follow-up appointment with a cardiologist at that time.
Cardiac tamponade is a medical emergency and needs immediate care. If you have any injury to your chest, especially near your heart, you should seek urgent medical attention. This includes injuries from any impact, whether it penetrates your skin or not. You should also seek urgent medical attention if you’re recovering from cardiac tamponade and any of the symptoms return.
You should also go to the hospital if you had surgery or pericardiocentesis and you show any symptoms of an infection. These include:
Questions to ask your healthcare provider may include:
Cardiac tamponade is a serious medical condition, and it’s normal to feel fear or anxiety if you have it. Caring for your mental health can be an important part of recovery. Your healthcare provider can connect you with counseling or other mental health services that can help you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether your pericardial disease comes on acutely without warning or is chronic, Cleveland Clinic has the best treatments for this heart condition.
