Acute pericarditis is a painful condition where the fluid-filled pouch around your heart is inflamed. This can happen because of infections, cancer or heart surgery. While it’s usually not dangerous on its own, it shares symptoms with a heart attack. That means you shouldn’t ignore symptoms and should get medical care right away if you have them.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
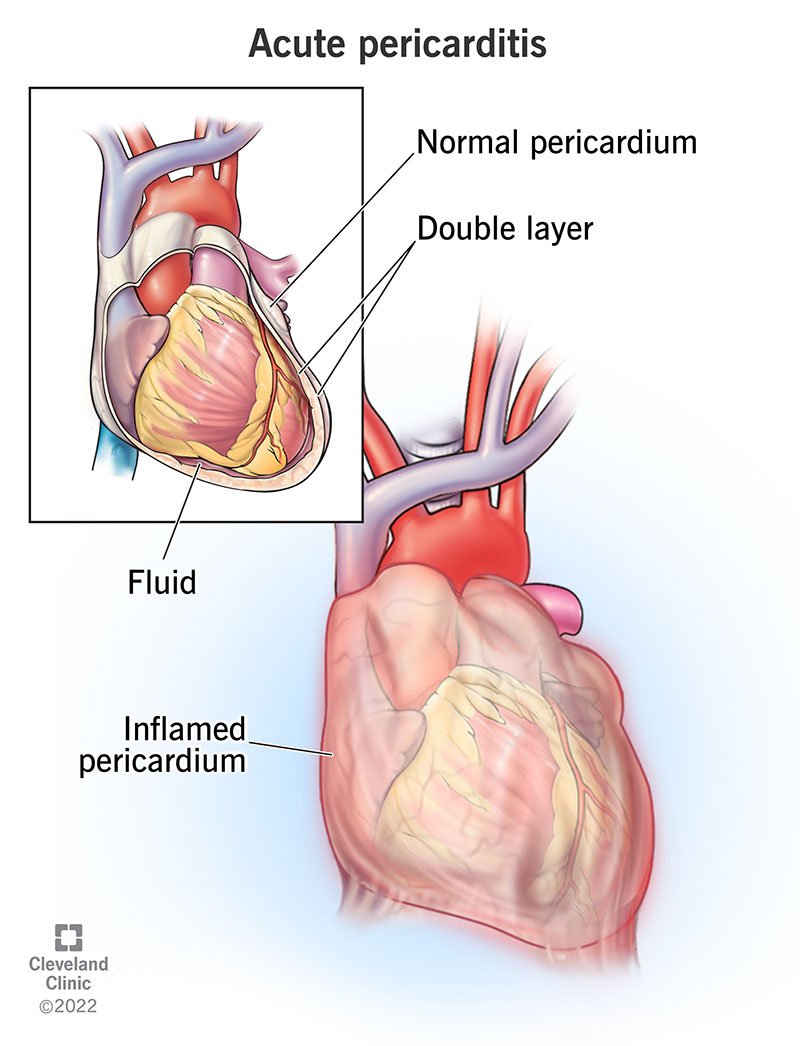
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22918-acute-pericarditis)
Acute pericarditis is painful inflammation of the pericardium, the fluid-filled pouch surrounding your heart. The pain usually gets worse when you’re lying down or when you breathe in. Depending on the cause, it’s almost always treatable, and most people with this condition will recover with few or no complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The pericardium is a double-layered pouch inside your chest. It holds your heart in place, and a thin layer of fluid between your heart and the inside layer reduces friction. The pericardium can provide cushioning and support to protect your heart from outside movement. However, you don't need a pericardium to survive, and many people are either born without one or have theirs removed with surgery and continue to live healthy lives.
Under normal circumstances, the pericardium has enough room inside it for your heart to expand and fill up with blood between heartbeats. Inflammation of the pericardium is usually not dangerous on its own, but it can lead to dangerous complications. These happen when fluid buildup inside the pericardium — a pericardial effusion — compresses your heart.
Swelling and fluid buildup inside the pericardium can fill that space and crowd out your heart. When this happens slowly, sometimes the pericardium can stretch to allow for the extra fluid and your heart to beat properly. But when it happens quickly, the fluid pushes on your heart. So the heart doesn't have room to expand and can’t fill up with blood as it should. This reduces how much blood your heart can pump and causes a condition known as cardiac tamponade, which is a life-threatening medical emergency. Tamponade can stop your heart, which is deadly within minutes.
Advertisement
Acute pericarditis can happen to people at any age but is more common in men. It's also most likely to happen to people between 20 and 50 years old.
Acute pericarditis is very common, making up about 5% of all emergency room visits related to chest pain.
Acute pericarditis can have several symptoms. Some of them are more likely to happen depending on the underlying cause of the pericarditis itself. The possible symptoms include the following.
The main symptom of acute pericarditis is chest pain. While this pain has many similarities to chest pain from a heart attack, there are also some important differences. The pain with acute pericarditis usually has the following features:
Other symptoms are possible with acute pericarditis, but they depend on the other conditions in question. Those conditions could have caused the case of pericarditis, or the case of pericarditis caused them.
Acute pericarditis can happen for many reasons. Potential causes include:
Advertisement
While acute pericarditis can happen because of contagious infections, you can’t spread acute pericarditis to or catch it from other people.
A doctor can diagnose acute pericarditis based on a combination of your medical history and symptoms, a physical exam, and diagnostic and laboratory tests.
Diagnosing acute pericarditis usually requires two or more of the following five signs and symptoms:
Many tests can help diagnose acute pericarditis. The tests you undergo depend specifically on your symptoms, what the healthcare provider suspects, and what other health conditions you have. The possible tests include those listed below.
Advertisement
These tests look for changes in your blood and any signs of certain infections. These usually include:
Diagnostic tests can help determine if you have acute pericarditis, and they can also offer valuable clues as to why you have it. Possible diagnostic tests include:
Advertisement
Some forms of diagnostic imaging can see acute pericarditis, while others can only detect problems that happen because of it. Imaging tests that are possible include:
The potential treatments for acute pericarditis depend on what’s causing it. When there’s a specific underlying cause, treatment focuses on treating that cause or any of its symptoms that lead to acute pericarditis. Your healthcare provider is the best person to explain the potential treatments when there is a known underlying cause. This is especially important because your provider can tailor the explanation to your particular condition(s) and situation.
When acute pericarditis doesn’t have a specific cause that healthcare providers can find, the focus is on treating its symptoms.
Treating the symptoms of acute pericarditis may involve one or more of the following.
Your healthcare provider may also advise you to change your routine and rest while you recover from this condition.
The possible complications from treatment depend strongly on the treatments you receive, especially medications. Your healthcare provider is the best person to tell you what you expect, including possible complications, from treatment for this condition. They can also help guide you on what you can do to avoid these complications and what to do if you have them.
Because it has similar symptoms to a heart attack, you shouldn’t try to self-diagnose acute pericarditis or manage it without first seeing a healthcare provider. Since a heart attack is a life-threatening medical emergency, you should treat chest pain as if it is a heart attack. If it isn’t acute pericarditis, you can have permanent heart damage if you wait too long to get treatment for a heart attack.
The severity of your case, the underlying cause and the treatments used will all affect how long it takes you to feel better after you develop acute pericarditis. In general, most people will feel better with one to three weeks of treatment, but it may take months before you recover fully.
Acute pericarditis is usually treatable and often curable, with most people making a recovery after treatment. Between 20% to 50% of people will have this condition more than once, but certain anti-inflammatory treatment methods may reduce the risk of this happening.
Depending on why you had acute pericarditis, you may have an increased risk of developing constrictive pericarditis, a complication where scarring on your pericardium makes it thicker and less flexible. This can restrict your heart’s ability to pump. This happens in about 20% to 30% of acute pericarditis cases because of tuberculosis or bacterial infections. With cancer- or immune disorder-related pericarditis, that drops to 2% to 5%. In acute pericarditis cases with an unknown or viral cause, it happens in less than 1% of cases.
Untreated acute pericarditis can turn into other conditions, some of which are more serious or even dangerous. Because of that, you shouldn’t let this condition go untreated.
With treatment, acute pericarditis should start to improve within weeks. However, most people will need to avoid physical activity — including exercise and sports — until symptoms improve. It’s common for symptoms to flare if you exercise too early. Your healthcare provider will be able to explain what you should expect and will schedule follow-up appointments to monitor your recovery for any signs of trouble.
Because acute pericarditis happens unpredictably, it isn’t a preventable condition. The only thing you can do is reduce your risk of developing it by avoiding situations or circumstances that can cause it.
The only way to avoid developing pericarditis is to avoid circumstances that can cause it. The ways you can do this include:
If you have a history of acute pericarditis, you should watch for any returning symptoms or if your symptoms change or get worse during your recovery. If you have these symptoms, you should call your healthcare provider or get medical attention if it’s outside of their business hours.
The main symptoms to watch for are:
*This symptom may be a sign of a heart attack, and you should call 911 (or the local emergency services number in your area) immediately.
Acute pericarditis is a condition that’s most likely to cause pain. While it’s usually not a serious condition on its own, it has symptoms similar to those of a heart attack, which is a medical emergency. It can also happen in connection with other conditions like cardiac tamponade, a medical emergency. Because of those similarities and connections, you shouldn’t delay getting these symptoms checked by a healthcare provider. If you have acute pericarditis, it’s usually treatable, but some people may have it more than once.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether your pericardial disease comes on acutely without warning or is chronic, Cleveland Clinic has the best treatments for this heart condition.
