Paresthesia is the feeling of tingling, numbness or “pins and needles.” Everyone experiences this feeling at some point in their lives. It’s most often a harmless sign that a limb is “asleep” and you need to shift position or move around. But when it won’t go away or happens often, it can be an important medical condition symptom.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Paresthesia” is the technical term for the sensation of tingling, burning, pricking or prickling, skin-crawling, itching, “pins and needles” or numbness on or just underneath your skin. It can affect places on and throughout your body and happens without an outside cause or warning.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Paresthesia (sometimes known as “paresthesia of skin”) is a very common experience. Everyone experiences it at some point, and it can happen for many reasons. Many of the common causes are harmless and are just a reflection of how your body works normally. But in some cases, paresthesia can signal a medical issue.
There are two main forms of paresthesia:
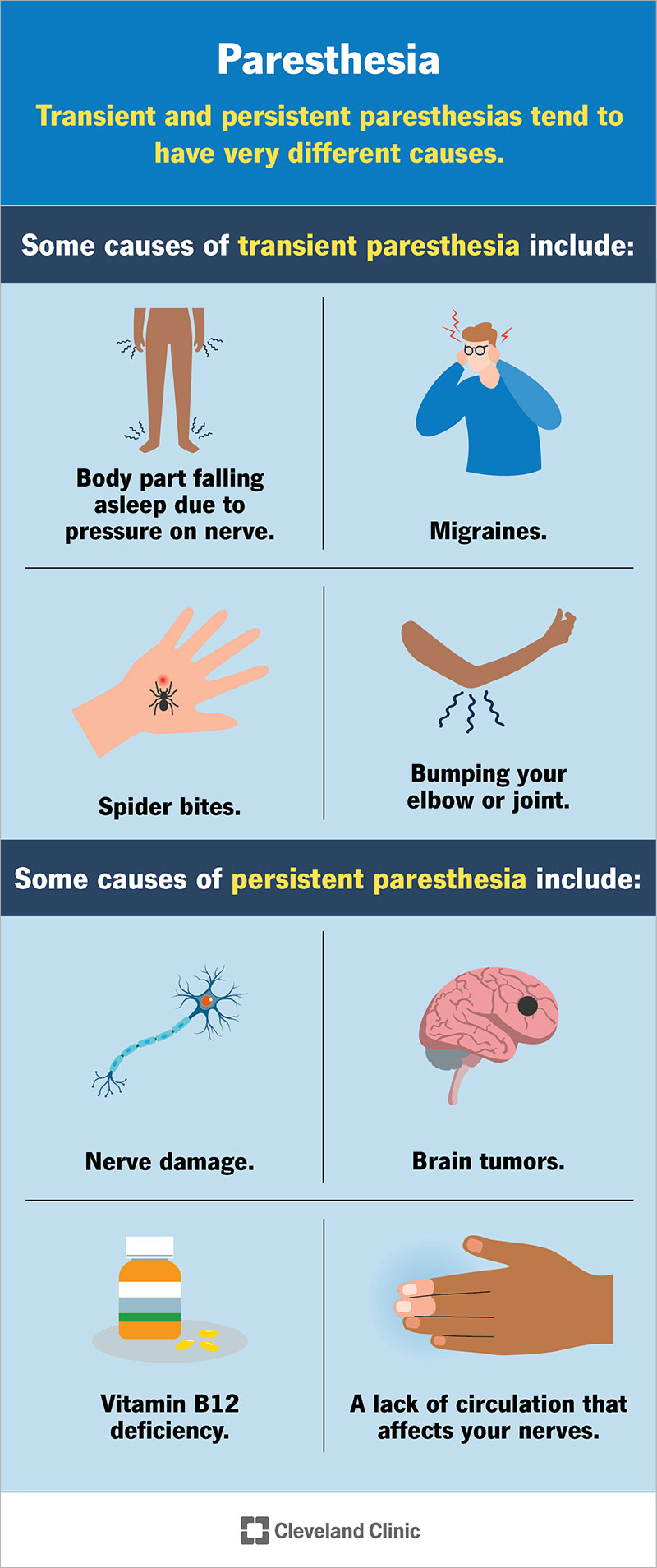
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24932-paresthesia)
Transient and persistent paresthesias tend to have very different causes.
Transient paresthesia is very common, and it’s usually harmless. It commonly happens because of body positioning that puts pressure on a nerve or limits blood flow (like folding a kink into a hose to keep liquid from flowing through). That can cause the affected body part to “fall asleep” (the technical term for this is “obdormition”). Paresthesia is the feeling of pins and needles that happens when you change position and release the pressure on the nerve or blood vessels in that body part.
Advertisement
Transient paresthesia can also happen if you hit certain body parts against solid objects. For example, bumping something with your elbow can cause a sharp, shock-like feeling of tingling or pain in your ulnar nerve. That’s known as “hitting your funny bone,” as your ulnar nerve is at the lower end of your main upper arm bone, your humerus.
Some other causes of transient paresthesia include:
Persistent paresthesia means it’s constant or happens very often. It’s more likely to be from serious causes, which tend to fall into certain categories.
Circulatory causes
One broad category is circulatory causes. A lack of circulation that affects your nerves can disrupt how those nerves carry signals to and from your brain. That can cause paresthesia.
Thoracic outlet syndrome is an example of a circulatory condition that may cause paresthesia. When it’s chronic, Reynaud’s syndrome can also be a form of circulatory-related paresthesia.
Nervous system causes
Neurological causes can involve your brain, spinal cord or nerves anywhere in your body. Some examples of neurological causes include:
Metabolic and endocrine causes
Metabolic and endocrine causes include vitamin deficiencies, conditions that affect certain hormones and more. Examples include:
Infectious diseases
Infectious diseases can commonly cause paresthesia when they affect nerves or parts of your brain. Examples of these conditions include:
Advertisement
Autoimmune and inflammatory diseases
Autoimmune conditions are when your immune system attacks parts of your own body. Paresthesia is one of the possible symptoms of an autoimmune condition that attacks your nerves. Inflammatory conditions can also cause swelling and tissue changes that affect nerves. These conditions can include:
Toxic effects
Like many tissues in your body, your nervous system is vulnerable to toxins and poisons. Examples of toxic sources of paresthesia include:
Other causes
Other conditions can also cause paresthesia. These can involve organ problems or conditions that don’t fall under the ones mentioned above. A few examples include:
Advertisement
Some forms of paresthesia — especially transient forms like a limb falling asleep — don’t need treatment. But many other forms of paresthesia may need treatment. The treatments depend on the underlying cause, which means the treatments can vary widely. Your healthcare provider is the best person to tell you about the possible treatments and which they recommend.
Most causes of paresthesia need treatment. Many of these conditions, especially several circulation-related and neurological causes, are dangerous or life-threatening without treatment. Other conditions that cause it, while not dangerous, are disruptive and can negatively affect your quality of life without treatment.
You should talk to a healthcare provider if you have paresthesia that affects the same body part on both sides, such as your hands or feet. You should also talk to a provider if you frequently have paresthesia that isn’t posture/body position-related. They can tell you what’s causing your paresthesia and whether or not it needs treatment.
If you have paresthesia frequently or constantly, you shouldn’t treat it on your own without first talking to a healthcare provider.
Paresthesia can be a symptom of serious medical conditions, some dangerous or even life-threatening. It’s important to talk to a healthcare provider if you have paresthesia that affects the same body part on both sides or if it happens with other symptoms (weakness or loss of function, loss of balance) that disrupt your life (even if the paresthesia doesn’t seem connected to the other symptoms).
Advertisement
A healthcare provider can evaluate your paresthesia and any related symptoms. Once they do, they can advise you on what’s causing your paresthesia and what you can do about it.
“Neuropathy” is a blanket term for any disease that affects a nerve. Paresthesia can be a symptom of neuropathy but can also happen for many other reasons. A healthcare provider can tell you if you have paresthesia because of neuropathy or for another reason.
Numbness is when you can’t feel sensations in the affected area. Paresthesia is a sensation you may feel when there’s a disruption in your sense of touch in the affected area.
Paresthesia and numbness are like neighbors when it comes to physical sensations. You often feel paresthesia just before numbness sets in, or paresthesia can be what you feel when sensation returns.
Paresthesia is something that everyone experiences at some point in their life. Most of the time, it’s from simple, harmless reasons like sitting in a position that causes your leg to fall asleep or sleeping on your hand for an extended period, making it feel numb for a while.
But paresthesia can also signal more serious health conditions. If you have paresthesia that keeps happening for unknown reasons, or if it happens with other symptoms, you should talk to your primary care provider or another healthcare provider. They can pin down what’s causing your paresthesia and help you understand why it’s happening and what — if anything — needs to be done about it.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
