A herniated (slipped or bulging) disk occurs when the soft, jelly-like center of a disk in your spine pushes against and leaks out of its outer ring. This can lead to pain, numbness and weakness in your neck, back or legs. Herniated disks usually heal on their own within four to six weeks. If symptoms persist, see a healthcare provider.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
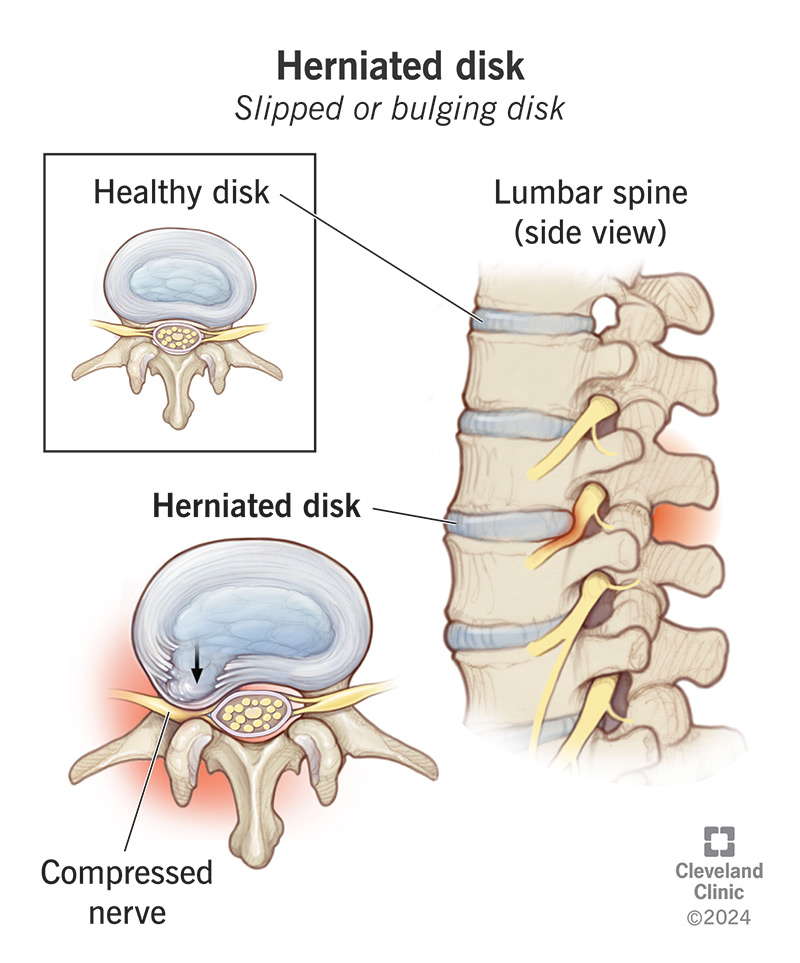
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/herniated-disk)
A herniated disk occurs when one of the disks in your spine (backbone) tears or leaks due to natural wear and tear or injury. This puts pressure on your spinal cord and irritates your spinal nerves, leading to pain, numbness and weakness.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You have a series of bones (vertebrae) in your spine, stretching from the base of your skull to your tailbone. Between your vertebrae are round cushions called disks. The disks act as buffers between your bones, allowing you to bend and move with ease. Over time, the disks become less effective and may become displaced. When this occurs, it’s called a herniated disk.
Other names for a herniated disk include:
Every year, more than 3 million people in the U.S. get a herniated disk. Bulging disks are a leading cause of neck, back and leg pain. They can happen anywhere along your spine, but they most often occur in your lower back (lumber spine) or your neck (cervical spine). It’s rare for a herniated disk to be in your upper-to-mid back (thoracic spine).
If you’ve experienced a slipped disk, you know the pain can be severe. The good news is that most cases resolve on their own without the need for surgical treatment. If you’ve had symptoms for more than a few weeks, reach out to a healthcare provider. They can explain your treatment options and get you back to enjoying the activities that you love.
Herniated disk symptoms vary depending on where the problem is in your spine. Although pain is a common symptom throughout your back, the location of the slipped disk may lead to other symptoms.
Advertisement
It’s common for a herniated disk in your lower back to cause “sciatic nerve” pain (sciatica). This sharp pain usually shoots down one side of your buttocks into your leg and sometimes your foot. Other symptoms of a slipped disk in your lower back may include:
Symptoms of a bulging disk in your neck may include:
Each disk in your spine has a soft, gel-like center and a firmer outer layer, kind of like a jelly doughnut. With time, the outer layer weakens and can crack. A herniated disk happens when the inner “jelly” substance pushes through the crack and presses on your spinal cord. The leaked material may press on nearby spinal nerves, causing the symptoms of a herniated disk.
Several factors can contribute to a disk rupture. Herniated disk causes include:
People ages 30 to 50 are most likely to get a herniated disk. The problem affects men twice as often women. In addition, the condition tends to run in families. Other risk factors include:
Your healthcare provider will do a thorough physical exam. During the exam, your provider will assess your pain, muscle reflexes, sensation and muscle strength. They may perform a straight leg raise test. With this test, your provider will have you lie on your back. Then, they’ll raise your leg straight in the air. If you experience any pain down your leg, you likely have a ruptured disk.
Your provider may also perform a neurological exam. They may also order imaging tests, including:
In most cases, pain from a slipped disk goes away in time. To ease pain while your disk heals, you can:
Advertisement
You may need more advanced herniated disk treatment if your symptoms aren't getting better. Your healthcare provider might recommend:
Herniated disks get better on their own or with nonsurgical treatment for 9 out of 10 people. If other treatments don’t relieve your symptoms, your healthcare provider may recommend surgery. There are multiple surgical techniques for relieving pressure on your spinal cord and nerves.
In rare cases, a large ruptured disk might injure nerves to your bladder or bowel. That may require emergency surgery. For non-emergency cases, herniated disk surgery is an option when other treatments don’t work. There are various ways to perform spinal decompression surgery, but the goal is to relieve pressure on your nerves.
The most common procedure is called a microdiskectomy. With this minimally invasive spine surgery, your provider will make a small cut (incision) through the skin near the slipped disk. They’ll insert a microscope and small tools through the incision to remove the herniated part of the disk.
Advertisement
Other surgical treatment options include:
For the majority of people, herniated disk pain gets better on its own or with simple medical care. You’ll probably feel better within a month. If you don’t, you should see a healthcare provider. Some people need more aggressive medical measures, like spinal injections or herniated disk surgery.
An untreated herniated disk can get worse. That’s especially true if you continue the activities that caused it — for instance, if it developed because of your work. A worsening ruptured disk may cause chronic (ongoing) pain and loss of control or sensation in the affected area. See a healthcare provider if you still have symptoms after four to six weeks of conservative care.
It’s not always possible to prevent a bulging disk. But you can reduce your risk by:
Advertisement
Initially, you can treat ruptured disk pain at home. But you should see a healthcare provider if:
Questions to ask your provider include:
Having a herniated disk can make you reluctant to move. But don’t just head to bed — too little movement can make pain worse when you get up again because muscles stiffen. Try to stay active and follow your healthcare provider’s recommendations for stretching. Gentle movement coupled with an over-the-counter pain reliever helps most people feel better in a few weeks.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Back pain can stop you in your tracks. But you don’t have to live like that. Cleveland Clinic is here to help you get moving again.
