Leprosy (Hansen’s disease) is a bacterial infection that can damage your nerves, muscles, eyes, skin and respiratory tract. It can cause permanent paralysis, blindness, and damage to your hands, feet and face. There’s no need to isolate from others as it doesn’t spread easily. It’s curable with antibiotics.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
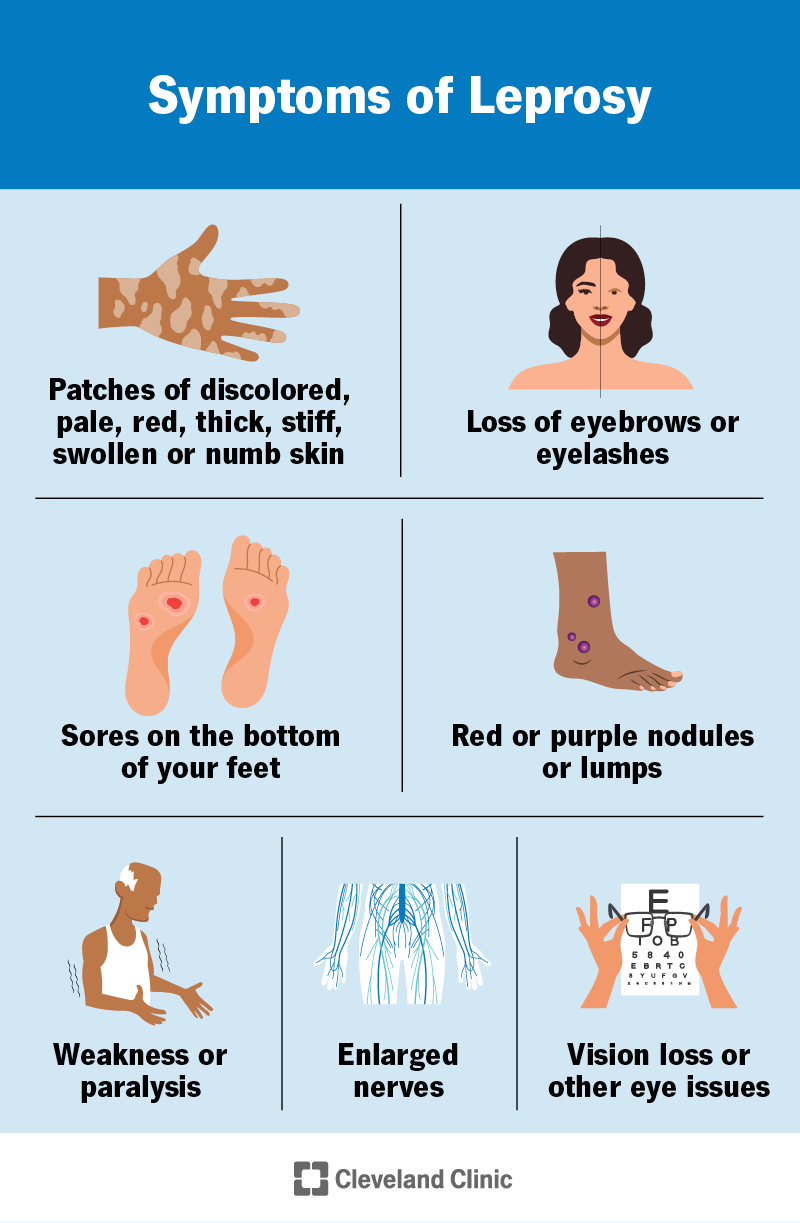
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23043-leprosy-hansens-disease)
Leprosy is a bacterial infection that damages your nerves, muscles, skin, eyes and respiratory tract. It can cause patches of pale or discolored skin, loss of sensation (numbness) and permanent disabilities.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Leprosy was once a mysterious disease that created a lot of fear. People with leprosy were often treated unfairly and isolated from others. We now know the cause and that it’s a treatable disease. It doesn’t spread easily from person to person.
Leprosy is also called Hansen’s disease. Some people prefer that name because of the stigma associated with the word “leprosy.”
Yes, leprosy still exists today. About 200,000 people are diagnosed around the world each year. It’s rare in the U.S.
Symptoms of leprosy include:
Leprosy develops slowly. It takes several years — sometimes, decades — to develop symptoms after exposure.
Mycobacterium leprae bacteria cause leprosy. Experts don’t fully understand how the disease spreads, but they think it’s transmitted through airborne droplets when an infected person coughs or sneezes.
Yes, leprosy is contagious (spreads from person to person). But it’s not easy to get. You have to spend a long time — many months — in close contact with someone to get leprosy. Most people’s immune systems fight it off. You’re not contagious if you’re receiving treatment.
Advertisement
You’re at higher risk for leprosy if you live in areas where it spreads. This includes parts of Asia, Africa and South America.
Complications of leprosy include:
A healthcare provider diagnoses leprosy by doing a physical exam, looking at your skin and getting a nerve or skin biopsy. They may also get blood tests or perform tests of your nerves or muscles (like nerve conduction tests).
Depending on your symptoms, a provider might diagnose you with:
Leprosy is curable. Healthcare providers use a combination of three antibiotics, known as multidrug therapy (MDT), to kill the bacteria. Antibiotics to treat leprosy include:
You’ll have to take these medications for six to 12 months. Take all medications as prescribed, even when your symptoms start to improve. There’s no need to isolate from others while in treatment.
A provider might also recommend surgery to remove nodules and help with nerve damage.
Any time you develop skin sores, numbness or muscle weakness, it’s important to schedule an appointment with a healthcare provider. They can determine if your symptoms are due to leprosy or another health condition.
If you’ve been diagnosed with leprosy, get treatment right away. The sooner you begin treatment, the less likely it is that you’ll have severe or lasting symptoms. Your provider will continue to monitor you over the next couple of years.
Antibiotics can cure the infection, but nerve damage and disabilities caused by leprosy can be permanent. They may get worse even years after treatment.
When treated, someone with a mild form of leprosy can expect to live about as long as someone without it. If left untreated for too long, leprosy can lead to severe complications and death.
It’s not easy to contract leprosy. If you’re in close contact with someone who has it, your provider may recommend getting tested yearly to make sure you can treat an infection early, before you have any symptoms.
Advertisement
Yes, some leprosy communities still exist. In the past, misunderstanding and fear around the disease led to the belief that people with leprosy needed to be isolated from others. Now, we know that that isn’t true. Most people are treated on an outpatient (at home) basis. But some people still live in the communities, either due to stigma or because they’ve made it their home over many years.
No, leprosy isn’t a sexually transmitted infection (STI). It’s thought to infect your respiratory tract.
Yes, some do. A species of armadillo native to the southern U.S. and Mexico can carry leprosy and spread it to humans.
Leprosy was shrouded in mystery for centuries. This led to fear and misunderstanding. Today, we understand the cause. We know that leprosy is curable — and not even very contagious. Unfortunately, the stigma around it often remains. Healthcare professionals around the world work every day to end the stigma and change the way people think about leprosy.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Have a virus, fungus or bacteria? Some of these “bugs” won’t go away on their own. Cleveland Clinic’s infectious disease experts are here to help.
